What you need to know about rectal prolapse (rectal prolapse)?
This information is intended to help you better understand rectal prolapse (rectal prolapse). It can be useful both for patients suffering from rectal prolapse or rectal prolapse, as well as for their friends, relatives and carers during their illness. We strive to help you understand what kind of disease this is, assess the severity of your condition and introduce treatment methods. Treatment often requires surgery and the material outlines why surgery may be recommended, what the different treatment options are, what it involves and how we can help.
Diet
Despite the fact that there is no diet for rectal prolapse as such, dietary correction is a mandatory component of conservative treatment. Since rectal prolapse is very often caused by chronic constipation, a “Constipation Diet” or a “Fiber Diet” may be prescribed. They are based on the inclusion of high-fiber foods (fiber) in the diet and drinking plenty of fluids. Sources of fiber are products of plant origin: bran, cereals (oatmeal, wheat, barley, pearl barley), garden greens, legumes, raw vegetables/fruits, seeds, nuts (almonds, peanuts). That is, in essence, it is necessary to include large amounts of whole, natural food in your diet.
The basic principles of creating a diet enriched with fiber include:
- adding bran to soups, cereals, fermented milk products, juices, jelly;
- consumption of raw vegetables/after cooking (beets, zucchini, fresh cabbage of various types, carrots, cucumbers, pumpkin, tomatoes) simultaneously with meat/fish (protein) products;
- using day-old bread made from whole grain flour or with added fiber;
- separate consumption of legumes/cereals (barley, pearl barley, millet) cooked in water with vegetable side dishes;
- if possible, more often consume fruits with the skin as a snack, as well as dried soaked fruits as an additive to kefir or various dishes (figs, dried apricots, apricots);
- eating prunes both whole and in the form of infusion;
- daily consumption of fermented milk products: acidophilus yogurt, fermented baked milk, kefir, matsoni, kumiss;
- daily consumption of free fluid (in the amount of 2.0-2.5 l/day).
The following are subject to exclusion/restriction from the diet:
- bakery products made from premium flour, baked goods made from puff pastry/yeast dough;
- chocolate and cream products;
- products/dishes with a high content of tannins (pears, dogwoods, quince jelly, blueberries, bird cherry, cocoa and coffee, strong black tea;
- dishes with a viscous consistency (mashed potatoes, slimy soups, jelly, pureed porridge), slowing down the passage of food through the esophagus;
- seasonings/spices (mustard sauces, horseradish, garlic, pepper) and spicy foods that strongly irritate the gastrointestinal mucosa, as well as difficult-to-digest foods (hard-boiled eggs, fatty meats/fish, canned food, smoked meats);
- foods that directly cause constipation or take a long time to digest (semolina, rice, noodles, potatoes, vermicelli, legumes).
What is rectal prolapse?
Rectal prolapse (the last part of the colon before it exits the anus) is a condition caused by weakness of the pelvic musculo-ligamentous system, which causes the colon to “turn inside out” out through the anus. The disease rarely leads to serious medical problems, but has a significant impact on quality of life.
In general, rectal prolapse is a rare pathology (2.5 cases per 100,000 people). This condition occurs mainly in adults, and women over 50 are six times more likely to develop rectal prolapse than men. Most women with rectal prolapse are over 60 years old, while men are on average 40 years old or younger. These younger patients are more likely to have autism, developmental delays, and psychiatric problems requiring multiple medications. Although surgery is not always required for this disease, conservative tactics do not provide a complete cure. Radical treatment of rectal prolapse requires surgery.
Complications after surgery
It is extremely important to adhere to the recommendations of your doctor to avoid complications. If you follow the rules of personal hygiene and pay attention to the symptoms, the risk of relapse is reduced to zero. Recurrence of the disease is diagnosed if the patient takes a hot bath or visits a sauna.
It is necessary to change the diet . It is worth including fermented milk products, cereals and broths, vegetables and fruits in the menu. Drinking plenty of fluids has a positive effect on the functioning of the gastrointestinal tract. It is strictly forbidden to take any medications without the knowledge of your doctor. Self-medication leads to negative consequences and even death.
Complications arise if the patient does not seek medical help on time. Self-medication is fraught with bleeding . Ulcerative colitis and duodenal ulcer develop. The patient is concerned about incontinence and problems with bowel movements. In advanced cases, necrosis of the walls of the rectum or tissue necrosis develops.
If you do not follow the rules of personal hygiene, an infectious process develops that affects all internal organs and leads to an abscess. The wound begins to fester. Seek help from medical specialists at the private proctology center “Proctologist 81”. Make an appointment at a time convenient for you.
How does rectal prolapse manifest?
Rectal prolapse tends to occur gradually in most cases. At first, during the act of defecation, only the mucous membrane falls out, which soon goes back into the anus. At this time, patients describe “something falling out of the anal canal.” Rectal prolapse is accompanied by a sensation of a foreign body in the anus. In the initial stages, rectal prolapse can be confused with a significant hemorrhoid, and sometimes this can confuse even doctors.
Once prolapse becomes apparent, fecal incontinence (the inability to keep hard, liquid stools and gases in the anus) occurs in 50-75% of cases and is associated with a number of factors. The anal sphincter is a structure consisting of many muscles that help keep feces in the intestines. When the rectum prolapses, the anal sphincter does not perform its function, causing stool and mucus to pass out of the rectum uncontrollably. Damage to the pudendal nerve occurs in many patients with prolapse. The pudendal nerve is responsible for the functioning of the anal sphincter. Damage to it can be the result of direct trauma (birth injury), chronic diseases such as diabetes, or a back injury or surgery. In addition, the anal sphincter is constantly stretched due to the prolapse itself, which becomes an additional risk factor.
Between 25% and 50% of patients report constipation. The constipation that accompanies rectal prolapse occurs as a result of a violation of the anatomy of the rectum, it seems to curl in on itself, creating both a mechanical “blockage” and aggravated by tension, general problems with coordination of the entire pelvic floor and problems with the ability of the colon to move chair forward at normal speed. Over time, the prolapsed rectal lining can thicken and ulcerate, causing severe bleeding.
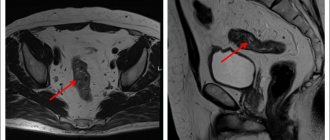
Diagnostics
Diagnosis of rectocele consists of collecting the patient’s complaints, ascertaining the history of the disease and life. This allows us to determine the causes of the disease and suggest existing anatomical defects of the pelvic floor. Next, a standard gynecological examination is performed, which gives an idea of the degree of prolapse and the condition of the perineum. There are four degrees of rectocele:
- 1st degree – when there is a slight prolapse, which is determined only during a gynecological examination and does not reach the entrance to the vagina by more than 1 cm;
- 2nd degree - when the prolapse of the posterior wall does not reach the entrance to the vagina a little or falls below it, but not more than 1 cm;
- 3rd degree - in this case, the rectocele descends more than 1 cm from the entrance to the vagina, but no more than 5-7 cm;
- 4th degree – complete inversion of the posterior vaginal wall.
To clarify what exactly comes out along with the back wall of the vagina, a gynecological examination is always supplemented by a digital rectal examination - examination of the rectum with a finger through the anus.
How to recognize bowel prolapse?
Diagnosing bowel prolapse requires a thorough history and physical examination of the patient. Particular attention is paid to complaints of constipation, fecal incontinence and any complaints of urinary incontinence or vaginal protrusion. Direct examination of the anal area is very important and often reveals decreased anal sphincter tone (the sphincter appears “relaxed”). The patient may be asked to squeeze and relax his anal sphincter while the doctor holds a finger in the anal canal or on the patient's buttock. This helps the doctor understand how the anal sphincter works. Sometimes anal manometry (direct measurement of anal sphincter pressure) may be ordered.
Rectal prolapse and hemorrhoids are not easy to differentiate. To assess rectal prolapse, the patient may be asked to strain while observing it while squatting on the toilet. Although this can be somewhat confusing for patients, it is important to get an accurate diagnosis as the treatment for hemorrhoids and rectal prolapse varies greatly.
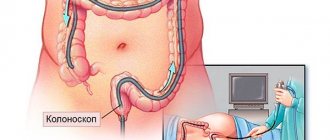
In the process of making a diagnosis, instrumental methods are also used. A colonoscopy is often necessary to rule out any underlying conditions, polyps, or cancer before considering surgical treatment for rectal prolapse. This is a procedure that uses a special instrument called a colonoscope to examine the entire inside of the colon.
If the diagnosis remains in doubt, defecography is prescribed. During the examination, the patient is injected with a radiopaque paste, then he sits on a special toilet chair and X-ray photographs of sequential actions are taken: rest, holding, straining, bowel movement. As already mentioned, rectal prolapse can occur due to general incompetence of the pelvic floor muscles. Between 20 and 35% of patients with rectal prolapse complain of urinary incontinence, and 15% of women experience rectal prolapse into the vagina (the sensation of something sticking out into the vagina). These additional problems can also be identified by defecography.
Many people who suffer from rectal prolapse experience constipation. It is important to note that depending on the severity of symptoms, the patient may be asked to undergo a special test (passing X-ray contrast material through the intestines) to assess the ability of their colon to pass stool. Several x-rays are taken over five days to see how the contrast travels through the small and large intestines, which is called "transit time."
Anal sphincter surgery
An addition to the surgical treatment of a prolapsed rectum is anal sphincter plastic surgery. Plastic surgery is necessary to restore the functionality of the sphincter, retention of the intestines, as well as gases and feces. Narrowing of the anal passage is performed using surgical threads or other synthetic plastic materials.
This type of surgery is indicated only in some cases and has a high risk of complications. More effective is suturing the edges of the sphincter with the resulting defect after resection of the rectum. Strengthening the rectovaginal septum of the perineum is carried out by connecting the edge of the levator muscle with a strong catgut suture.
What will happen if left untreated?
Patients who decide to do nothing after diagnosis (especially early on) can expect the severity and frequency of the prolapse to increase over time, and the rectal prolapse itself to be milder (may simply fall out while standing). If a patient delays treatment for a long period of time, they should be aware that the longer time passes, the greater the likelihood of permanent fecal incontinence problems as the anal sphincter is continually stretched and the chance of nerve damage also increases. The length of time over which these changes will occur varies greatly from person to person. In some cases, the prolapse is minor or surgery is contraindicated for the patient. In these cases, support clothing can help prevent persistent or recurrent loss. Without treatment, rectal prolapse does not develop into cancer.
Operation Delorme
In case of rectal prolapse, Delorme surgery may be indicated, which allows you to completely get rid of the problem. Delorme's operation is considered physiological, since after it is performed the intestine fully retains its functions.
Delorme's operation can be performed in two ways:
- With access through the anorectal opening. First, resection of the prolapsed part of the rectal mucosa is performed. Next, the muscle layer is collected using a thread and fixed in the anal canal area. The remaining part of the mucosa is sutured. Special sutures are placed on the muscle wall to hold the rectum in its anatomical position and strengthen the sphincter. This type of intervention is considered the least traumatic among similar operations and can be prescribed to older people and those with weakened bodies.
- With access through the perineum. The incision is made in the perineal area. First, the prolapsed area is also excised. Subsequently, to strengthen the muscle layer, a synthetic mesh is used, which should fix the anatomical position of the rectum. This operation has a low relapse rate and can be used for all age groups.
Treatment of rectal prolapse
Conservative treatment
All methods of conservative treatment of rectal prolapse, including manual reduction of the organ, pararectal administration of sclerosing drugs, electrical stimulation of the pelvic floor and sphincter muscles, do not guarantee complete cure of the patient. They can only be used in young people and exclusively at the initial stage of the disease. But even under such conditions, it is impossible to guarantee a 100% complete cure and no relapses in the future.
Surgery
Radical treatment of rectal prolapse is only possible through surgery. There are two main approaches for surgical treatment of this disease - transabdominal operations (through the abdomen) and perineal operations (through the perineum). Both approaches aim to prevent the recurrence of prolapse and usually lead to significant improvements in quality of life.
The choice of type of operation depends on two factors: the characteristics of the patient himself and the severity of the disease. The former include the patient's age, gender, bowel function, urinary incontinence, previous surgeries, and the severity of associated medical problems. The second includes: the degree of prolapse, what impact the intervention may have on bowel function and urinary continence, complication rates, recurrence rates and the individual experience of the surgeon.
Most surgeons would agree that the abdominal approach provides the best chance for long-term successful treatment of rectal prolapse. The perineal approach is often better suited for very elderly patients, or patients with very severe comorbidities. For younger men, the perineal approach may also be considered as there is a small chance (1-2%) of causing sexual dysfunction due to nerve damage during the abdominal approach. Although this is not typical, it should be considered when deciding on the type of surgery.
How is the operation performed?
Surgical interventions for rectal prolapse can be performed under various types of anesthesia. The patient and surgeon decide what is appropriate for a given patient based on their particular circumstances. Possible options:
- General anesthesia (full sleep with a breathing tube in place).
- Spinal anesthesia (similar to an epidural injection during childbirth).
- A combination of intravenous relaxants and local anesthesia (painkillers) given around the anus after the relaxers are taken.
Doctors of the University Clinic of Moscow State University. M.V. Lomonosov during surgery on the rectum
Transabdominal operations
Most abdominal techniques involve making an incision in the lower abdomen and separating the rectum from surrounding tissue. Then a rectopexy is performed, in which the rectum is pulled up and attached to the sacrum (the back wall of the pelvis) in various ways. Depending on the surgeon's preferences, the rectum can be fixed with sutures or using a special mesh to the anterior surface of the sacrum. Regardless of the specific technique used, the goal is to hold the rectum in the appropriate position until it is secured there by new scars. In general, both of these methods give very good results: recurrence (recurrence) of rectal prolapse occurs in approximately 2-5% of cases.
It is important to note that while prolapse can be corrected, fecal incontinence or constipation may not always be cured.
In recent years, the popularity of minimally invasive methods such as laparoscopic or robotic interventions has increased. Laparoscopy is a method in which the surgeon enters the area to be operated on without using large incisions. Two small incisions are made in the abdominal cavity, through which special instruments with optics and a light source are inserted. The surgeon observes the operated area on the monitor screen. In this case, the same procedures are performed as for abdominal approaches described above.
One of the promising areas for the development of minimally invasive surgery has been the introduction of robot-assisted operations into practice. In each of these cases, the operation performed is identical to the open access. Potential benefits of minimally invasive techniques include: reduced trauma and blood loss, reduced pain, shorter hospital stay, and earlier return to full activity and work. Not all surgeons have the experience or knowledge to perform these surgeries and therefore they are not always available.
Perineal surgeries
Perineal access allows to reduce the percentage of postoperative complications and trauma, as well as shorten the length of hospital stay, compared with transabdominal interventions. Until recently, it was believed that these benefits were offset by higher relapse rates. However, if performed correctly, perineal surgery can provide good long-term results.
Rectosigmoidectomy
The most common perineal approach is often called a perineal rectosigmoidectomy or "Altemeier procedure", named after the surgeon who popularized this procedure. This approach to surgical treatment of rectal prolapse is performed through the anus without making an abdominal incision. In the operating room, the rectum is deliberately forced to prolapse. A circular incision is made throughout the entire thickness of the intestinal wall. Next, the excess mucous membrane is cut off, after which a hardware or manual anastomosis is applied (connection of the colon to the anus). The absence of an abdominal incision, minimal trauma, and shorter hospital stay make this treatment option preferable for elderly patients with severe comorbidities. This method has a higher recurrence rate (>10%) than abdominal approaches (2–5%), with complication rates ranging from 5 to 24% and including bleeding and pelvic infection. Fecal incontinence may be a more serious problem after this procedure compared to abdominal rectopexy, although most patients already have urinary incontinence. The rectum's job is to serve as a reservoir for stool, and this procedure removes the rectum. As a result, the colon is now doing the work of the rectum, and it may not be able to hold stool as well as the rectum itself. To solve this problem, levatoroplasty can be performed. Levatoplasty is performed at the same time as a perineal rectosigmoidectomy and involves “tightening” the pelvic floor muscles by suturing some of them closer together. This helps with fecal continence in two thirds of patients.