Rectum
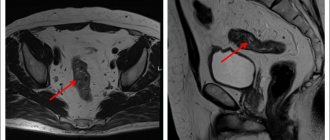
The rectum is a tube with muscular walls consisting of longitudinal and transverse layers, it is fixed in the pelvis by ligaments and has a length of about 15 cm. The rectum then passes through the rectosigmoid junction into the sigmoid colon. The rectosigmoid junction has the appearance of a bend of 70-120 degrees. For 10-15 cm from the anus, the rectum has practically no painful endings and does not contact the small intestine located in the abdomen. Due to these features, when performing sigmoidoscopy, discomfort occurs only when it is necessary to examine the rectosigmoid section and the final segment of the sigmoid colon and is caused by passage through the rectosigmoid junction and contact through the wall of the sigmoid colon with the small intestine, on the surface of which there are many pain receptors, while diagnosis of the rectum itself is practically painless.
Preparing for treatment
Before surgery, diagnostic tests are usually performed to check your general health and ensure that the surgery can be performed. This may include blood sampling, chest x-ray, electrocardiogram (ECG), angiography, CT or ultrasound, or endoscopy. You should follow a diet that excludes legumes, baked goods, alcohol, fresh fruits and vegetables. A liquid diet is administered at least the day before surgery, with nothing taken on the day of surgery. Depending on the type of bowel resection, it may be necessary to cleanse the bowel. This usually involves taking a laxative 1-2 days before surgery. Cleansing enemas may also be given in the hospital. Immediately before the procedure, antibiotics are prescribed to help prevent infection. You should also tell your doctor about all the medications, supplements, and herbal products you take.
Anal canal
The anal canal is the terminal part of the rectum, it ends with the anus and has a pronounced muscular wall - the anal canal sphincter complex. This complex consists of external and internal sphincters, which are responsible for voluntary and involuntary retention of feces and gases. In the anal canal, the rectal mucosa transitions into the epithelium (anodermis) of the anal canal, which then passes into the skin of the perianal area. In the skin part of the anal canal there is a very large number of pain receptors, and on the mucous membrane they are practically absent. When an anal canal fissure develops, it is located on the skin part, its bottom is the subcutaneous/superficial portion of the sphincter (constituting no more than 1/10 of its total volume), and with mechanical irritation (bowel emptying), a pronounced spasm of this muscle develops, and intense pain syndrome. That is why performing a drug blockade or dosed sphincterotomy in the case of a fissure with pain that is not amenable to conservative treatment leads to its rapid healing.
Introduction
Paraproctitis - acute or chronic inflammation of the peri-rectal tissue - is a very common disease. In the structure of proctological diseases, it ranks fourth after hemorrhoids, anal fissures, and colitis. Among people with diseases of the rectum, patients with acute paraproctitis account for an average of 15.1%. Paraproctitis is more common in males, mainly in working age (from 20 to 50 years).
Mention of this suffering dates back to the era of Hippocrates, but the treatment of paraproctitis has its own characteristics and remains a difficult task even today.
Patients with acute paraproctitis often end up in hospitals on duty with general surgeons, so their competence in diagnosing and treating this pathology is extremely important.
In this publication, we have tried to present modern methods of diagnosis and treatment of paraproctitis in an accessible manner.
Anal fissure: symptoms, causes and treatment from experienced doctors at the MEDSI clinic
Table of contents
- Causes
- Symptoms
- Anal fissure in children
- Chronic fissure
- Consequences (complications) of anal fissures
- Diagnostics
- How to treat anal fissure?
- Prevention
- Advantages of treatment at MEDSI
An anal fissure (anal fissure) is a tear in the lining of the rectum. As a rule, pathology develops in people who suffer from chronic constipation or lead a sedentary lifestyle. Fissures are diagnosed in approximately 20% of patients who consult a doctor with the problem of discomfort in the rectal area. The pathology can be either independent - arising from exposure to traumatic factors, or secondary - a consequence of a number of concomitant diseases (external hemorrhoids, peptic ulcers, disorders of the gastrointestinal tract).
Causes
An anal fissure is caused primarily by trauma to the rectum or constipation and hemorrhoids.
Damage may result from:
- Gastritis, peptic ulcer, colitis
- Congestion in the rectum and pelvis caused by disruption of the cardiovascular system
- Pregnancy during which the uterus puts excessive pressure on internal organs
- Childbirth associated with prolonged pushing
Don't think that an anal fissure will heal on its own. If the patient does not change the nutritional system and eliminate traumatic factors, nothing will change. In addition, acute pathology often becomes chronic. In this case, the patient suffers from severe discomfort and often experiences not only physical, but also psychological problems. If you contact a specialist immediately after detecting signs of pathology, treatment will be carried out quickly using conservative methods. In advanced cases, treatment of chronic anal fissure is often only possible through surgery.
Symptoms
The main symptoms of anal fissure that require consultation with a doctor and treatment are:
- Discomfort after defecation
- Pain
- Minor bleeding
Over time, these symptoms are often accompanied by:
- Sphincter spasm
- Unpleasant sensations when sitting
- Constipation
The patient becomes irritable, sleeps poorly, and fears bowel movements.
Anal fissure in children
Children suffer from anal fissures less often than adults, but in some cases the pathology occurs even in newborns. To prevent the disease from becoming chronic and causing complications, treatment should be started as early as possible. Any self-medication is strictly prohibited, since it only relieves symptoms, but does not eliminate the problem, starting the course of the pathology.
Young children cannot report signs of pathology to adults, so you should monitor:
- Baby's behavior when excreting feces
- Stool density
- Child's behavior before going to the toilet. Children often become irritable and nervous and do not want to sit on the potty.
If a child cries before and during bowel movements, is afraid of going to the toilet, or suffers from constipation, you should definitely consult a doctor.
Chronic fissure
The acute form of anal fissure often becomes chronic. Especially often, pathology develops rapidly in the absence of adequate therapy. It develops into a chronic form mainly in women who have recently given birth. This is due to physiological changes in the body of a young mother. With pathology, the patient suffers not only during bowel movements, but also after it, with prolonged sitting and walking. Constant discomfort, itching and bleeding are added to the standard symptoms. The process is often aggravated by self-medication, taking laxatives, using suppositories and enemas.
Consequences (complications) of anal fissures
If an anal fissure is not treated, the following complications arise:
- Constant bleeding
- Infectious processes in the intestinal mucosa
- Prostatitis
- Rectal fistulas
- Colitis
- Acute paraproctitis
All of them are dangerous not only for health, but also for the life of the patient, and also lead to the development of a number of psychological problems.
Diagnostics
To make a diagnosis, a comprehensive examination of the patient is performed.
It includes:
- Examination of the anus
. An anal fissure is diagnosed fairly quickly, as the mucous membranes lose their integrity and become swollen - Finger examination
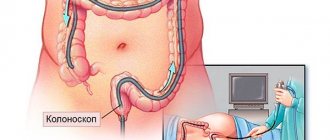
. With such a study, the proctologist can determine the size of the crack and feel its edges - Sigmoidoscopy
. Allows you to examine the rectum to a depth of 20 centimeters
Laboratory diagnostics, colonoscopy and irrigoscopy may also be prescribed.
How to treat anal fissure?
Conservative therapy
Treatment of anal fissure is always carried out comprehensively. It is important to eliminate not only the symptoms of the pathology, but also its cause. The underlying disease must be eliminated. Treatment will be useless if the patient suffers from constipation and hard stool constantly damages the anus.
Typically therapy includes:
- Treatment of the anus with emollient compounds
- Relaxation of anal muscles in warm baths
- Preventing constipation
- Using ointments and suppositories for pain relief, wound healing and inflammation relief
Treatment is determined by the form of the pathology, the factors that provoked its development, and the individual characteristics of the patient. It can only be prescribed by a doctor after a comprehensive diagnosis.
Surgery
Surgical interventions are resorted to when conservative therapy does not give the desired result.
All methods used are divided into 2 types:
- Minimally invasive
. Usually the crack is removed using a laser. Its edges are simply sealed. Recovery after such an intervention does not take much time. Within a few days the patient returns to his normal lifestyle and does not experience discomfort. - Standard
. The sphincterotomy technique is used. During this intervention, the doctor makes an incision and separates the layers of sphincter muscle. Thanks to this, the existing spasm is eliminated, which allows you to reduce tension during bowel movements. Also, suturing of the walls and excision of the mucous membranes on which scars have appeared are carried out.
The choice of surgical intervention technique is made by the doctor.
Prevention
There is a set of preventive measures to prevent the formation of an anal fissure.
This includes:
- Healthy lifestyle. You should completely stop smoking and drinking alcoholic beverages, eating fatty, fried and salty foods, which stimulate problems in the cardiovascular system and digestive tract. It is important to consume foods rich in fiber, vitamins and valuable microelements in sufficient quantities.
- Compliance with personal hygiene rules. You should wash regularly and prevent the development of inflammatory and infectious processes.
- An active lifestyle, including regular, but not excessive or tiring physical activity. It is enough to walk at least 20-30 minutes a day
- Proper drinking regime. You need to drink at least 1.5-2 liters of fluid every day
- Avoiding eating foods that are too hot or cold
It is important not to restrain the urge to defecate and promptly treat any diseases of the gastrointestinal tract.
Advantages of treatment at MEDSI
- Use of current treatment methods. Our clinics use drug blockades, excision of anal fissures and other procedures and interventions.
- Experienced doctors. MEDSI proctologists constantly improve their qualifications and master modern methods of conservative therapy and surgical interventions
- Comfortable conditions. All examinations and treatment are carried out by experienced specialists whom our patients trust. There is no fear or embarrassment during the procedures
- No queues. You can consult a doctor at a convenient time
- Compliance with confidentiality rules
If you want to make an appointment with a proctologist at MEDSI, call +7 (495) 7-800-500.
How is colorectal cancer treated?
Surgery to completely remove the tumor is the only method that offers a chance of curing colorectal cancer. Before surgery, it is necessary to determine whether the tumor is localized in the rectum or whether the process is generalized (for example, it has spread to the liver or lungs). Even if the tumor has spread, treatment is still possible. Currently, small rectal tumors are removed immediately, without preoperative chemoradiotherapy. Large tumors require preoperative treatment. There are currently two treatment options. The first is to irradiate the rectal tumor with fairly high doses of radiation for one week (short course). The second option is a combination of low-dose radiation and well-tolerated chemotherapy for five weeks (long course). Scientific research shows that the purpose of pretreatment (radiation) is to reduce the risk of local recurrence (that is, the likelihood that the tumor will return after surgery). Surgery is performed 6-8 weeks after the end of chemoradiotherapy. Surgical treatment involves complete removal of the rectal tumor. After surgery, surgical samples (tissue that was removed during surgery) are sent for pathological examination, during which the depth of the tumor and the presence of metastases in the lymph nodes will be determined. Based on the results of the pathological examination, the feasibility of additional preventive postoperative chemotherapy is determined.
Observation program after treatment method
After your bowel resection you will need to stay in the hospital for several days. The patient should be given warm, liquid food for 1-2 days after surgery. Solid foods and meals will be introduced gradually. If a colostomy or ileostomy has been performed, a specially trained health care professional will teach the patient how to care for themselves. Temporary ostomies usually remain in place for several months. After the rest of the colon has healed, another operation, an anastomosis, will be performed. The hole in the stomach will be closed. A nasogastric tube is inserted through the nose into the stomach during surgery and may be left in place for 24 to 48 hours after surgery. This eliminates stomach secretions and prevents nausea and vomiting. It will remain until bowel activity resumes. Postoperative patient care also includes monitoring of blood pressure, pulse, respiration and temperature. Fluid intake and output are measured, and the color and amount of drainage from the wound is observed at the incision site. The patient can get out of bed approximately 8-24 hours after surgery. Most patients will stay in the hospital for 5-7 days, although laparoscopic surgery can reduce this stay to 2-3 days. Postoperative weight loss accompanies almost all bowel resections. Weight and strength are slowly restored over several months. You will need to follow a diet prescribed by your doctor. Full recovery from surgery may take two months. Laparoscopic surgery can reduce this time to one to two weeks.
Possible complications during treatment
The side effects that may occur depend mainly on the type of bowel resection and your overall health. They include:
- obstruction (obstruction) of the intestine,
- paralyzed or inactive bowel
- damage to nearby organs such as the bladder, ureter or spleen, anastomotic leak associated with infectious problems,
- excessive bleeding wound infection,
- hernia,
- thrombophlebitis,
- inability to control urination.
The attending physician should be informed of any of the following problems after surgery: severe pain, swelling, redness, drainage or bleeding in the incision area, muscle pain, dizziness or fever, constipation, nausea or vomiting, rectal bleeding or black, tarry stools.
Positron emission tomography (PET).
During their growth, cancer cells spend more energy and absorb more glucose than healthy cells. These characteristics can be used to diagnose a tumor and its metastases. During positron emission tomography (PET), radioactively labeled glucose is injected intravenously and taken up by rapidly growing metabolically active cells (mostly cancer cells), making them visible during the study. Considering the high cost of the method, PET is used to perform specific tasks, such as searching for metastases and diagnosing possible relapse of the disease.
Prognosis after treatment method
The period of time required for recovery varies depending on the initial condition, type of resection, the patient's general health prior to surgery, and the length of bowel removed. The prognosis of bowel resection depends on the severity of the disease. For example, in the case of patients with ulcerative colitis, the disease is cured and most people go on to live normal, active lives. Patients with cancer will have a less positive prognosis (due to possible relapses). Alternatives to bowel resection depend on the specific medical condition being treated.
Which doctor should you contact if symptoms occur?
If you or your loved ones have the described complaints, you should contact a coloproctologist as soon as possible, who, after consultation and examination, will establish a preliminary diagnosis and determine further tactics and urgency of treatment, or, if in doubt about the diagnosis, a list of necessary additional studies.
If surgery is required, you will be offered hospitalization in a hospital, where, after assessing the results of the studies, which, as a rule, do not take much time and are easy to perform, the operation will be performed.
Why do you choose us?
Part of the Perm State Medical University named after. I.M. Sechenova Clinic of Coloproctology and Minimally Invasive Surgery is an example of a new generation of medicine, harmoniously combining the deepest fundamental knowledge, honed skills, a modern multidisciplinary approach and attentive attitude to any category of patients.
KKMH is a guarantee that the surgical interventions performed within our walls correspond to the most current ideas about colorectal surgery. This includes our own department of anesthesiology and intensive care, whose employees ensure a smooth course of the operation and the early postoperative period and treat seriously ill patients. This is an “open intensive care unit”, where you can not only find out the most complete information about the condition of a loved one, but also be with him during a difficult time for him.
The doors of our Clinic are open to patients who were denied treatment in other hospitals due to the complexity of the surgical intervention or the neglect of the process. Elderly patients, patients with a “bouquet” of concomitant diseases (so-called comorbid) are an area of our special interest. The presence in the hospital of such highly professional specialists as a cardiologist, pulmonologist, urologist, etc. allows us to treat patients of any age and with any concomitant diseases.
KKMH is a dynamically developing team of specialists who sincerely and deeply love their work, who are continuously learning and teaching others, who are interested in keeping you healthy.
Treatment of complex fistulas should be divided into 2 stages
At the first stage, a drainage ligature is installed into the fistula tract - a thin, almost invisible suture material (Fig. 7). The main goals of this stage of treatment are: the formation of a direct fistula tract around the ligature, drainage of possible leaks, reduction of the inflammatory process, prevention of self-closure of the external opening for constant drainage of inflammatory and/or purulent discharge.
Figure 7. Drainage ligature
At the second stage, after the acute inflammation subsides (4-6 weeks), the main surgical treatment is performed - excision of the fistula.
Important! Two-stage surgical treatment provides conditions under which radical surgery becomes possible with minimal complications.
Currently, in the treatment of rectal fistulas, various biological materials based on connective tissue (Permacol), fibrin glue, and collagen paste are widely used, which are introduced into the fistula tract, tamponing it. These methods have a lesser effect on the rectal closure apparatus; their use does not lead to the formation of a massive wound defect. However, the rate of disease recurrence is significantly higher than radical surgery.
Promising modern methods for treating fistulas are endoscopic (VAAFT) and laser (FiLaC) technologies for removal of affected tissue. These technologies practically eliminate the possibility of damage to the sphincter apparatus, however, today, the effectiveness in leading clinics in the world does not exceed 50-60%.