Colon cancer is a malignant neoplasm that occurs in the mucous membranes of the colon and rectum. Damage to the gastrointestinal tract occurs due to gene mutation. Pathological changes lead to the degeneration of normal cells into malignant ones. As a result, tumor cells begin to invade adjacent tissues and, over time, spread throughout the body.
Intestinal cancer at the initial stage develops almost asymptomatically.
Therefore, patients often turn to an oncologist when the disease is in an advanced state and tumor cells have already spread to the lymph nodes and metastasized to neighboring organs. IMPORTANT:
Cancer develops in the large intestine. The large intestine is made up of three sections: the cecum, colon, and rectum—cancer can develop in any of them.
Kinds
Based on histological characteristics, intestinal cancer is divided into:
- adenocarcinoma - a formation of malignantly changed glandular cells and occurs in 95% of all cases of the disease;
- lymphoma - a tumor formed from fibrous tissue of the intestinal wall;
- carcinoma - a formation consisting of epithelial cells;
- sarcoma is a malignant tumor that forms mainly on the outer wall of the intestine from connective tissue cells;
- melanoma - the basis are skin cells called melanocytes.
Tumors are classified according to the type of growth:
- exophytic - growing on the inner wall in the intestinal lumen, as a result of which obstruction of the organ gradually develops;
- endophytic – growing into the intestinal wall with subsequent formation of ulcers and a high risk of metastases upon contact with healthy tissues;
- diffuse – tumors growing to the sides from the focus without narrowing the intestinal lumen;
- mixed - having characteristics of two or three of the listed types.
List of sources
- Tsukanov A.S., Shelygin Yu.A., Achkasov S.I., Frolov S.A., Kashnikov V.N., Kuzminov A.M., Pikunov D.Yu., Shubin V.P. Principles of diagnosis and personalized treatment of hereditary forms of colorectal cancer. Bulletin of the Russian Academy of Medical Sciences. — 2019
- Association of Oncologists of Russia. Practical recommendations for drug treatment of patients with colon cancer. — 2014
- V.V. Martynyuk. Colon cancer (morbidity, mortality, risk factors, screening). St. Petersburg Medical Academy of Postgraduate Education. — 2000
Symptoms
In case of intestinal cancer, the first symptoms are manifestations of general intoxication, developing due to the growth of a malignant neoplasm and the immune response, as well as due to impaired digestive function. Among them:
- fatigue, general weakness;
- joint pain as a result of an autoimmune reaction;
- a steady increase in temperature to a little over 37 degrees;
- unexplained weight loss;
- aversion to the smell of meat or some other products;
- nausea;
- pale skin;
- flatulence, bloating, colic;
- dark stool with lots of mucus.
Subsequently, as the intestinal tumor grows, the symptoms increase and new signs appear;
- cramping abdominal pain with a frequency of 15-20 minutes;
- asymmetrical increase in abdominal volume;
- frequent vomiting due to general intoxication;
- alternating diarrhea and stool retention;
- traces of blood in the stool.
When intestinal obstruction occurs due to the tumor blocking the intestinal lumen, the intestinal wall stretches excessively, blood circulation in it is disrupted, resulting in necrosis of the deformed tissue and peritonitis.
Symptoms of colon damage
The main clinical signs of cancer are presented:
- deviations in the standard functioning of the gastrointestinal tract with dyspeptic disorders, changes in the structure of feces, lasting more than 1 month;
- the appearance of blood particles in the stool;
- discomfort in the abdominal area, flatulence, periodic pain syndrome;
- a feeling of incomplete emptying of the intestines;
- deterioration of condition, loss of body weight.
The early stages of cancerous lesions are asymptomatic. The first clinical manifestations of the disease occur with a significant increase in tumor volume and may be associated with its location.
Causes and risk factors
At the moment, there is no reliably established list of causes of intestinal cancer, but experts know factors that increase the risk of developing a malignant tumor.
- Benign neoplasms. This includes adenomas and polyps that form in the intestines, but there is no exact data on what exactly triggers the process of malignant degeneration of cells.
- Chronic inflammation. These are nonspecific ulcerative colitis, Crohn's disease, dysbiosis of various types, colon diverticulosis (formation of peculiar pockets in the intestinal wall).
- Unbalanced diet. A lack of plant fiber in combination with a large amount of highly processed meat products causes impaired peristalsis and irritation of the intestinal wall.
- Impact of external factors. Aniline dyes, carcinogenic compounds, and radioactive radiation can serve as a trigger for the malignant degeneration of cells.
Causes of the disease
Colon cancer most often begins with benign polyps (adenomas). Oncology can develop both inside the intestine and spread beyond it, affecting surrounding tissues.
Risk factors for developing colorectal cancer:
- Age—the risk of developing the disease increases with age. Before age 40, a diagnosis of colorectal cancer is very rare. The risk increases after age 50, with peak incidence occurring in the eighth decade of life.
- Obesity (in people with a body mass index (BMI) greater than 30, the risk of developing the disease increases by 50-100 percent compared with people of the same weight, that is, a BMI below 24.99);
- Unhealthy diet high in animal fats, red meat and processed foods and low in vegetables, fruits and dietary fibre;
- Low physical activity;
- Smoking (it is estimated that up to 20% of colorectal cancer cases are related to smoking);
- Previous radiation therapy to the abdomen;
- Taking immunosuppressants after organ transplantation;
- Alcohol abuse;
- Previous gallbladder removal;
- HPV (human papillomavirus) infections;
- A history of cervical, vulvar, or vaginal cancer.
A tendency to intestinal cancer can be inherited. Yes, genes, along with a poor lifestyle, are the most common cause of colon cancer. It is estimated that 15-30% of colorectal cancer cases are genetic.
However, genetic factors are not just the fact that someone in the family previously suffered from colorectal cancer and could pass on the defective gene to their descendants.
Genetic factors also include:
- familial adenomatous polyposis syndrome, which is considered a so-called precancerous condition (colorectal cancer develops in 75-95% of patients with familial adenomatous polyposis);
- Lynch syndrome (formerly called hereditary nonpolyposis colorectal cancer). This is the most common cause of genetically determined colorectal cancer, accounting for 1-3% of cases;
- inflammatory bowel diseases (for example, ulcerative colitis increases the risk of colon cancer by 20 times).
IMPORTANT:
Patients with a family history of colorectal cancer, especially those over 40 years of age, should undergo annual medical examination and genetic testing.
Stages
Clinical symptoms of intestinal cancer directly depend on the stage of the disease.
- The tumor develops within the epithelium and does not penetrate other tissues; there are no metastases. Clinical manifestations are absent or so insignificant that they do not attract the patient’s attention. Diseases are discovered accidentally during histological examination of removed polyps.
- A malignant neoplasm grows into the submucosal or muscular layer without affecting adjacent lymph nodes. The disease may manifest itself in the form of initial general symptoms.
- The tumor grows through the entire intestinal wall and can affect neighboring organs. Metastases are present in regional lymph nodes. Severe symptoms include general malaise and intestinal dysfunction.
- The malignant node gives multiple metastases to distant organs. The patient experiences constant abdominal pain, intestinal bleeding, and severe intoxication with tissue breakdown products.
Questions and answers
How to recognize bowel cancer?
The initial symptoms of bowel cancer are similar to a number of other, less dangerous diseases, so patients often do not pay attention to them. If for no apparent reason:
- loss of appetite, aversion to meat dishes;
- stomach ache periodically;
- there is constant discomfort in the abdomen, gas formation has increased;
- prolonged constipation began, alternating with bouts of diarrhea;
this means that you should contact a gastroenterologist or proctologist for examination as soon as possible.
Is there a cure for bowel cancer?
Patients with intestinal tumors can be treated at any stage of cancer. The chances of complete relief from malignant pathology remain even in the most advanced cases.
Colon cancer with metastases: how long do patients live?
Without medical care, the life of a patient with metastases to other organs is 6-11 months, depending on the rate of development of secondary tumors. When completing a course of treatment, the five-year survival rate in patients with metastases is 30-45%, i.e. at least thirty people out of a hundred live more than five years after surgery.
Attention! You can cure this disease for free and receive medical care at JSC "Medicine" (clinic of Academician Roitberg) under the State Guarantees program of Compulsory Medical Insurance (Compulsory Medical Insurance) and High-Tech Medical Care. To find out more, please call +7(495) 775-73-60, or on the VMP page for compulsory medical insurance
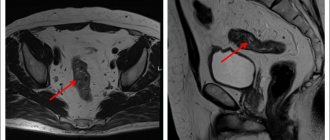
Diagnostics
The main difficulty in diagnosing intestinal cancer is the patient’s failure to see a doctor in a timely manner.
In the early stages, clinical manifestations are mild, which makes it difficult to make a primary diagnosis.
To identify a tumor, a number of tests are prescribed.
- General and biochemical blood tests. The level of hemoglobin, the number of red and white blood cells, the level of bilirubin, the presence of tumor markers, etc. are examined.
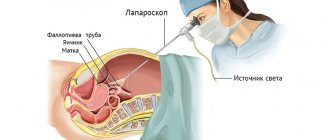
- Colonoscopy. Using a special probe inserted into the anus, an oncologist or gastroenterologist examines the large intestine for the presence of tumors and ulcerative defects. If suspicious areas are detected, a biopsy is performed followed by histological examination of the tissue.
- Irrigoscopy. X-ray contrast examination of the large intestine reveals deformed areas, tumors, compactions and other structural abnormalities.
- Ultrasound of the abdominal cavity. The study makes it possible to clarify the size of the tumor, detect germination into other organs and metastases in the lymph nodes, liver, mesentery, and other organs.
- CT scan of the abdomen. The most accurate and informative study allows you to estimate the size of the tumor, determine the stage of cancer, germination into organs, and the presence of metastases.
Colon cancer - symptoms and treatment
Surgery
Surgery is the main method of radical tumor removal. In the early stages of the disease, only its implementation is sufficient. For common processes, treatment is always complex: in addition to surgery, radiation therapy, chemotherapy and targeted therapy may be required. For minimally invasive neoplasms, gentle organ-preserving interventions are performed, which are performed endoscopically [1]. In other cases, resection (removal) of the intestine in compliance with the rules of ablastics:
- the tumor is removed en bloc with the tissues involved in the process: regional lymph nodes are also subject to removal. In addition to the therapeutic purpose, removal of lymph nodes also has a valuable diagnostic value - their morphological study provides information about the presence of metastases and helps to accurately determine the stage of the process. This has an impact on further treatment tactics, in particular the need to prescribe postoperative chemotherapy or radiation therapy;
- there must be a sufficient distance from the visible edge of the tumor to the edge of resection - ideally, about 30-40 cm of intestine is removed. The resulting material is sent for urgent histological examination to determine the presence of tumor cells at the resection margins.
For rectal cancer, radical treatment involves chemoradiotherapy . In some cases, this allows you to save the rectum and anal sphincter.
Surgical treatment can be performed in one or two stages . In one-stage treatment, tumor removal and restoration of intestinal continuity are performed during one operation, when the resection edges are connected by anastomosis . This is possible if several conditions are met:
- the connected areas are sufficiently supplied with blood;
- there is no tension in the stitched areas;
- low risks of infectious complications.
If these conditions are not met, there is a high probability of developing anastomotic leakage, necrosis and infectious complications. To avoid this, two-stage interventions are performed. At the first stage, the tumor is removed, and the adducting end of the intestine is brought to the anterior abdominal wall in the form of a colostomy, through which the intestinal contents will be released.
After the patient completes antitumor treatment, the results of which are satisfactory, doctors carry out reconstructive interventions to restore intestinal continuity.
If there are distant metastases, it is recommended to remove them surgically at the same time as the primary tumor. Such operations are called simultaneous and are performed by a combined team involving surgeons of related specialties [5].
Endoscopic stenting
One of the common complications of colorectal cancer is intestinal obstruction. In addition, with metastasis to the liver, obstructive jaundice can develop. Both conditions are life-threatening and require immediate medical attention. One of the methods to solve the problem is stenting - installation of a special frame that ensures straightening of the pathologically narrowed area. In case of intestinal obstruction, the introduction of a stent into the site of obstruction straightens the tumor masses, allows you to expand the intestinal lumen and ensure the free passage of intestinal contents. Thus, intestinal obstruction is relieved, which makes it possible to more thoroughly prepare for surgery. This is especially important in oncology practice, since such patients, for example, have time to undergo neoadjuvant chemotherapy. In patients at high risk of surgical or anesthetic complications, stenting is the main method of correction of intestinal obstruction.
With the development of obstruction of the bile ducts, a similar intervention is performed on the hepatobiliary system . Using an endoscope, a stent is inserted into the narrowing site through the common bile duct, which is located in the duodenum. Alternatively, bougienage and balloon dilation may be used.
Chemotherapy
Chemotherapy for colon cancer is carried out after surgery (adjuvant) and is prescribed in the following cases:
- presence of regional metastases;
- involvement of the entire thickness of the intestinal wall in the process;
- poorly differentiated tumors;
- the presence of malignant cells at the resection margins.
Neoadjuvant chemotherapy treatment of primary unresectable tumors is also possible. In this case, several courses of chemotherapy are prescribed, and after their completion, the possibility of radical surgery is re-evaluated.
Chemotherapy is recommended to be prescribed no later than 28 days from the date of surgery (in the absence of contraindications). In this case, the main therapy lasts 3-4 months, after which maintenance therapy is carried out.
Treatment can be supplemented with targeted drugs - bevacizumab, cetuximab, panitumumab. These drugs act on specific processes that determine the vital activity of tumor cells. They are prescribed after molecular genetic testing. Some drugs are used only with chemotherapy, others can be used both in monotherapy and as part of combination therapy [2][5].
Targeted therapy
Targeted drugs act on cellular mechanisms that ensure carcinogenesis - the process of formation and development of a malignant tumor. They cannot completely destroy cancer, but they significantly slow down its growth and progression. Due to their highly specialized action, these drugs are prescribed only after special tests are carried out that reveal the presence of mutations for which targeted therapy is indicated or, conversely, is ineffective.
For example, adding bevacizumab, cetuximab, or panitumumab to standard chemotherapy regimens for the treatment of metastatic colon cancer increases overall survival from 18 months to 29 months. Bevacizumab inhibits the activity of endothelial growth factor, which reduces tumor vascularization. Cetuximab and panitumumab act on the epidermal growth factor receptor (EGFR), which is responsible for the differentiation, proliferation and survival of malignant cells.
Radiation therapy
Radiation therapy is mainly used in the treatment of rectal cancer, since other parts of the intestine have pronounced physiological mobility, which makes it impossible to clearly position the tumor for planning radiation fields [3]. In other cases, it is used for palliative purposes for the treatment of distant metastases.
For rectal cancer, radiation therapy is used as part of a combination treatment together with chemotherapy. In some cases, this makes it possible to carry out organ-preserving treatment without removing a colostomy [3].
Dispensary observation
Once treatment for colon cancer has been successfully completed, there is still a risk of recurrence. It is highest during the first three years, so all patients require regular follow-up. Typically, doctor's examinations, ultrasounds and blood tests for carcinoembryonic antigen (CEA) are carried out at the following frequency:
- in the first 2 years - every 2-3 months;
- over the next 3 years - every six months;
- then - annually.
In addition, it is necessary to undergo a colonoscopy every two years. If pathological changes are detected during these examinations, the doctor will prescribe a computed tomography scan, bone scan and other diagnostic methods.
Features of rehabilitation
After surgery for colon cancer, the doctor gives standard recommendations regarding nutrition and return to physical activity. The recovery time depends on the type of surgery and the method of performing it (endoscopic, laparoscopic or open through an incision). If the patient has a permanent colostomy, they will be told how to properly care for it before discharge.
Some chemotherapy side effects persist after treatment is completed. In this case, the doctor will prescribe the necessary treatment to relieve them and give the patient recommendations on lifestyle. Many people who have recovered from cancer experience psycho-emotional problems and are constantly afraid of relapse. In such cases, the help of a psychologist is required.
Treatment
The choice of treatment for bowel cancer depends on the stage of the disease.
- At the zero stage, i.e. If polyps are detected, they are removed using colonoscopy, without opening the abdominal cavity
- At the first stage, the segment of intestine with the tumor and part of the mesentery are surgically removed.
- In the second stage, chemotherapy is given before surgery to shrink the tumor. After surgery, the remaining cells are destroyed using chemotherapy or radiation therapy.
- For stage three colon cancer, surgical treatment is performed in combination with chemotherapy or radiation therapy. Areas affected by cancer and regional lymph nodes are removed.
- At the fourth stage, the nature of the operation depends on the degree of spread of malignant tumors. If it is impossible to remove the tumor, palliative treatment is performed to exclude intestinal obstruction.
Prevention
Lifestyle factors can contribute to the development of bowel cancer, so the following lifestyle changes should help reduce your risks:
- body weight control;
- regular exercise;
- maintaining a diet rich in whole grains, cereals, fruits and vegetables;
- reducing consumption of fats, salt and sugar;
- to give up smoking;
- reducing or stopping alcohol consumption.
Bowel cancer develops slowly and, if detected early enough, is limited to parts of the bowel and can be successfully removed. If a person is over 50 years old, an annual screening test will help detect any changes. Source: Preventing Stomach and Colon Cancer. V.V. Egorenkov. Practical Oncology, T. 12, No. 2 - 2011..
Article sources:
- Prevention of stomach and colon cancer. V.V. Egorenkov. Practical Oncology, T. 12, No. 2 - 2011.
- Colorectal cancer: a guide for patients. Information for patients based on clinical guidelines from the European Society of Medical Oncology (ESMO). — 2021.
- Expression of the icam-1 gene in tumor cells of patients with colon cancer. Knyazev D.I., Novikov D.V., Sakharnova T.A., Presnyakova N.B., Kuznetsova O.S., Kazatskaya Zh.A., Spiridonova N.A., Alyasova A.V., Novikov V. .IN. Bulletin of Nizhny Novgorod University named after. N.I. Lobachevsky No. 2, 2010. p. 528-531
- Modern aspects of surgical treatment of colorectal cancer. Dauletbaev D.A., Kaliaskarov E.Sh., Menayakov M.T., Serikov N.S., Aubakirov E.A. Bulletin of the Kazakh National Medical University No. 1, 2021, p. 226-229
- Locally advanced colon cancer – aspects of surgical tactics. Kutukov V.V., Sluvko L.V., Sevostyanov V.V. Tyumen medical journal No. 2, 2010. p. 79-80
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Rehabilitation
In the first few days after surgery, the patient is given intravenous nutrition. In the future, it is necessary to adhere to special nutritional principles, consuming only liquid and pureed foods. A special diet for intestinal cancer is prescribed taking into account the individual characteristics of the body, but the menu must include liquid dishes, fresh and boiled vegetables and fruits. In addition, during the recovery period it is necessary to avoid physical and psychological stress, regularly visit a doctor, and take prescribed tests.