- Types of rhinosinusitis
- Factors predisposing to the development of rhinosinusitis
- Reasons for the development of rhinosinusitis
- Development mechanism
- Symptoms of rhinosinusitis
- Diagnosis and recommended clinical studies
- Laboratory research methods
- Instrumental research methods
- Differential diagnosis
- General principles of treatment
- Forecast
Rhinosinusitis is an inflammation of the mucous membrane of the paranasal sinuses.
Types of rhinosinusitis
- Acute (duration of illness less than 12 weeks and complete disappearance of symptoms after recovery).
- Recurrent (from 1 to 4 episodes of acute rhinosinusitis per year, periods between exacerbations (when there are no symptoms of the disease and no treatment is carried out) last at least 8 weeks).
- Chronic (presence of symptoms for more than 12 weeks).
Localization
- maxillary sinus (sinusitis),
- sphenoid sinus (sphenoiditis),
- frontal sinus (frontitis),
- in the cells of the ethmoid bone (ethmoiditis).
Depending on the etiological factors, acute and recurrent rhinosinusitis is divided into:
- viral,
- bacterial,
- fungal.
Chronic are divided into:
- bacterial,
- fungal,
- mixed.
Taking into account the characteristics of pathogenesis:
- hospital,
- odontogenic,
- polyposis,
- developed against the background of immunodeficiency states of rhinosinusitis,
- acute (fulminant) form of mycosis of the paranasal sinuses.
Chronic fungal rhinosinusitis is divided into:
- allergic (eosinophilic) fungal sinusitis,
- mushroom ball,
- superficial sinonasal mycosis,
- chronic invasive form of mycosis.
Disease prognosis
On the one hand, for 60-80 percent of patients, complete recovery from acute rhinosinusitis takes about two weeks. On the other hand, the duration of chronic sinusitis can last for years, and in some cases even for a lifetime. Therefore, it is important to eliminate the causes, and not just carry out local anti-inflammatory treatment in the stages of exacerbation.
Complications of sinusitis are quite rare with timely and correct treatment. However, the chronic inflammatory form can spread to the adjacent periosteum, bone and soft tissue. More serious treatment in a hospital is necessary for complications of the organs of vision and orbit, meningeal membranes or brain.
Factors predisposing to the development of rhinosinusitis
- Rhinitis.
- Intolerance to non-steroidal anti-inflammatory drugs.
- Anomalies in the structure of the nasal cavity and paranasal sinuses (deviated nasal septum; bulla of the middle turbinate; additional anastomosis of the maxillary sinus, etc.).
- Immunodeficiency states (X-linked agammaglobulinemia; common variable immunological deficiency; deficiency of IgG subclasses; selective IgA deficiency; hyper-IgM syndrome; HIV).
- Diseases accompanied by a slowdown in MCT (Kartagener's syndrome; Young's syndrome; cystic fibrosis).
- Wegener's granulomatosis.
- Hyperplasia of the pharyngeal tonsil, adenoiditis.
- Gastroesophageal reflux disease.
- Fistula between the oral cavity and the maxillary sinus.
Reasons for the development of rhinosinusitis
The main causative agents of acute bacterial rhinosinusitis are Streptococcus pneumoniae and Haemophilus influenzae. Other pathogens include Moraxellacatarrhalis, Staphylococcusaureus, Streptococcuspyogenes, Streptococcusviridans, etc. The main anaerobic pathogens of rhinosinusitis are anaerobic streptococci. However, the spectrum of pathogens causing acute bacterial rhinosinusitis can vary significantly depending on geographic, socio-economic and other conditions.
The list of nosocomial pathogens that developed against the background of immunodeficiency conditions and odontogenic rhinosinusitis, along with the bacteria mentioned above, includes Staphylococcus epidermidis, Pseudomonasaeruginosa, Proteus spp., and in immunodeficient patients also saprophytic bacteria and fungal microflora. In recent years, the role of chlamydia and other atypical microflora in the etiology of rhinosinusitis has been discussed.
Fungal sinusitis is most often caused by Aspergillus fungi (in most cases A. fumigatus), less often by Candida, Alternaria, Bipolaris, etc.
The acute invasive form of mycosis of the paranasal sinuses is most often caused by fungi of the Mucoraceae family: Rhizopus, Mucor and Absida.
Additional materials
Dear visitors, due to the fact that the topic is quite extensive both in terms of types and localization, as well as treatment methods, you can familiarize yourself with additional materials on the site covering various information about sinusitis.
Development mechanism
Rhinosinusitis almost always develops when mucociliary clearance is impaired, when optimal conditions are created for the development of a bacterial infection.
The trigger point in the development of acute bacterial rhinosinusitis is usually ARVI. It was revealed that in almost 90% of patients with ARVI, changes in the paranasal sinuses are detected in the form of swelling of the mucous membrane and stagnation of secretions. However, only 1-2% of such patients develop acute bacterial rhinosinusitis.
In the development of chronic rhinosinusitis, in addition to disturbances of mucociliary transport, abnormalities in the structure of the intranasal structures and ethmoidal labyrinth play an important role, blocking the patency of the natural openings of the paranasal sinuses and disrupting the mechanisms of sinus cleansing. The presence of two or more anastomoses of the maxillary sinuses also creates conditions for the throwing of infected mucus that has already been in the nasal cavity and back into the sinus. Under conditions of chronic inflammation in the mucous membrane, focal or diffuse metaplasia of multirow columnar epithelium occurs into multilayer epithelium, devoid of cilia and having lost the ability to remove bacteria and viruses from its surface through active mucociliary transport.
Nosocomial rhinosinusitis is most often caused by prolonged nasotracheal intubation.
Odontogenic sinusitis develops against the background of chronic foci of inflammation, cysts or granulomas in the roots of the teeth of the upper jaw, as a result of pieces of filling material, tooth roots entering the maxillary sinuses, or the formation of a fistula between the oral cavity and the maxillary sinus after tooth extraction.
A key role in the pathogenesis of polypous rhinosinusitis is played by eosinophils and IL-5, which causes their proliferation, migration into tissues and degranulation.
Mucopurulent discharge from the affected paranasal sinuses can be transported by the ciliated epithelium directly through the mouth of the auditory tube, which is the trigger point in the development of an exudative or chronic inflammatory process in the middle ear.
Superficial sinonasal mycosis is caused by the growth of fungal mycelium on crusts formed in the cavities of the operated paranasal sinuses, on the surface of neoplasms and on accumulations of antimicrobial drugs or glucocorticosteroids for topical use that remain in the nasal cavity for a long time.
Why does inflammation occur?
As already mentioned, each sinus is connected to the nasal cavity by small openings, through which the resulting mucous masses are released. If suddenly such secretion becomes impossible or difficult, mucus accumulates and stagnates. Favorable temperature promotes the proliferation of pathogenic microorganisms, causing inflammation to occur. This condition also develops in the case of anatomical features, when the normal outflow of mucus is difficult (deviated nasal septum, abnormal structure of the sinuses, etc.)
The second common cause is a viral infection. In response to the penetration of the pathogen, the sinuses begin to actively produce secretions in order to remove the infection from the body, but at some point there is too much of it that the mucous masses cannot come out. During infection, the nasal cavity swells, which also interferes with the normal outflow of mucopurulent secretions.
Also provoking factors are swelling due to breathing cold air, swelling caused by allergic reactions, polyposis, weak immunity, untreated teeth and other dental problems.
Symptoms of rhinosinusitis
The main symptoms of rhinosinusitis are:
- difficulty in nasal breathing,
- headache,
- nasal discharge.
Variable symptoms:
- decreased sense of smell,
- stuffy ears,
- increase in body temperature,
- general malaise,
- cough (more common in children).
With inflammation in the maxillary and frontal sinuses, the pain is localized in the face, nose and eyebrow area. Sphenoiditis is characterized by pain in the center of the head and the back of the head. The discharge is mucous, purulent and can come away when you blow your nose or drain down the back wall of the throat. The latter is more typical for lesions of the sphenoid sinus and the posterior parts of the ethmoid labyrinth. Chronic rhinosinusitis is accompanied by the same symptoms as acute, but outside of exacerbation they are much less pronounced.
Anatomy of the sinuses
The paranasal (paranasal) sinuses are a kind of air-carrying “pockets” in the skull. They are located around the nasal cavity and are connected to it through anastomoses (small holes).
There are four groups of sinuses. Based on their names, you can immediately understand their location:
- maxillary (maxillary) - paired;
- frontal (frontal) - paired;
- cells of the ethmoid labyrinth are paired;
- wedge-shaped - variable, can be paired or unpaired.
They perform several important functions: receptor (when air enters the sinus from the nose, it gives a signal to the brain how alert its mucous membrane should be: whether it needs to react with swelling when, for example, too cold air enters), protective (if foreign particles, irritation and the desire to sneeze arise, through which the nasal passages are cleared) and the olfactory sense.
Filled with air, they also reduce the weight of the skull, participate in the formation of the voice and are a kind of “airbag” for facial injuries.
Diagnosis and recommended clinical studies
The diagnosis of rhinosinusitis is established on the basis of:
- Anamnestic data.
- Clinical manifestations.
- Laboratory test results.
- Results of instrumental examination methods.
Acute bacterial rhinosinusitis is characterized by a connection with an episode of acute respiratory viral infection suffered 5-10 days ago.
Patients with a history of odontogenic and fungal sinusitis often have previous complex fillings of the teeth of the upper jaw, as well as a long history of repeated visits to an otolaryngologist and repeated diagnostic punctures of the maxillary sinuses, during which no contents were obtained.
Polypous rhinosinusitis is characterized by gradual progression of the main symptoms: difficulty in nasal breathing and decreased sense of smell. Often patients are bothered by the painful sensation of constant flow of a very viscous secretion down the back wall of the nasopharynx. In many cases, polypous rhinosinusitis is combined with bronchial asthma, intolerance to non-steroidal anti-inflammatory drugs, and cystic fibrosis.
Prevention
Follow these steps to reduce your risk of chronic rhinosinusitis:
- avoid upper respiratory tract infections;
- reduce contact with people suffering from respiratory diseases (colds, ARVI);
- if cold symptoms persist (7 days or more), do not delay going to the doctor;
- manage your allergies. Work with your doctor to keep your symptoms under control;
- avoid tobacco smoke and polluted air, replace filters in your car on time, and clean the air conditioner in a timely manner;
- humidify the air in the house at low humidity;
- avoid hypothermia.
Laboratory research methods
Bacteriological research
This is a study designed to isolate bacteria and study their properties in order to make a microbiological diagnosis. The material for the study can be obtained from the nasal cavity or from the affected sinus during puncture. When collecting material, there is a high probability of “traveling” microflora entering.
Study of mucociliary transport
Allows you to assess the condition of the mucociliary apparatus of the mucous membrane, that is, to identify one of the most important pathogenetic disorders in rhinosinusitis.
In clinical practice, the measurement of transport time is most widely used. One of the variations of this method is to measure the time during which a marker (charcoal, carmine, ink, foam, etc.) moves from the anterior parts of the nasal cavity to the nasopharynx. Due to its simplicity, the saccharin test has become more widespread.
Its principle is to measure the time it takes a particle to travel a conventional distance - from the anterior parts of the nasal cavity to the taste buds in the pharynx. Saccharin time in healthy people can range from 1 to 20 minutes, averaging 6 minutes. However, these indicators are very conditional.
Instrumental research methods
- Rhinoscopy. Anterior rhinoscopy against the background of diffuse congestive hyperemia and edema of the nasal mucosa reveals a typical sign of purulent rhinosinusitis - the presence of pathological discharge in the anastomosis area of the affected paranasal sinuses. With sinusitis and frontal sinusitis, the discharge can be seen in the middle nasal passage, and with sphenoiditis - in the upper.
- Endoscopic examination requires a minimum of time and is painlessly tolerated by the patient. The study includes three main points: sequential examination of the lower, middle and upper nasal passages. The method allows you to identify an additional anastomosis of the maxillary sinus. With a choanal polyp, a formation is detected, the stem of which comes from the anastomosis of the maxillary sinus.
- Diaphanoscopy. Illumination of pericutaneous formations or cysts with a narrow beam of light. Allows to identify a decrease in pneumatization of the maxillary and frontal sinuses.
- Ultrasound is a fast, non-invasive method that is used mainly for screening purposes, to diagnose inflammatory diseases and cysts of the maxillary and frontal sinuses. Both special devices for scanning the paranasal sinuses and standard equipment are used. The sensitivity of ultrasound in diagnosing sinusitis is lower than that of X-ray and CT.
- X-rays of the paranasal sinuses are usually performed in the nasomental projection. To clarify the condition of the frontal and sphenoid sinuses, an additional study can be carried out in the nasofrontal and lateral projections. X-ray of the ethmoid bone sinuses is not very informative. Poor quality radiography often leads to diagnostic errors.
- CT , which is performed in a coronal projection, is the most informative method and is gradually becoming the “gold standard” for studying the paranasal sinuses. CT not only makes it possible to establish the nature and extent of pathological changes in the paranasal sinuses, but also reveals the causes and individual features of the anatomical structure of the nasal cavity and sinuses, leading to the development and recurrence of rhinosinusitis. High-resolution CT allows you to visualize structures that are not visible with conventional radiography.
- MRI , although it provides better visualization of soft tissue structures, is not one of the main methods for diagnosing rhinosinusitis. This method gives virtually no idea of the patency of the air spaces connecting the paranasal sinuses with the nasal cavity. MRI is indicated only in certain situations - for example, if a fungal infection of the paranasal sinuses is suspected or the possible tumor nature of the disease, as well as with orbital and intracranial complications of rhinosinusitis. MRI is the most informative method for differential diagnosis between a cerebral hernia (meningoencephalocele) and a tumor or inflammatory process in the roof of the ethmoidal labyrinth.
- Diagnostic puncture and probing make it possible to assess the volume and nature of the contents of the affected sinus and indirectly obtain an idea of the patency of its natural opening.
To assess the patency of the anastomosis of the punctured sinus, a simple scheme is used, taking into account 3 degrees of violation of the patency of the anastomosis (see table). To do this, using a syringe connected to a needle or drainage tube, the contents are first aspirated, and then the sinus is washed.
Assessment of the patency of the natural anastomosis of the paranasal sinuses
| Normal patency of the anastomosis | During aspiration, air or liquid contents of the sinus enter the syringe; when rinsing, the liquid flows freely into the nasal cavity |
| Obstruction of the 1st degree | During aspiration, negative pressure is created; during rinsing, the liquid freely enters the nasal cavity (valve mechanism and negative pressure in the sinus) |
| Impairment of patency II degree | Aspiration from the sinus is impossible; rinsing is possible only by increasing pressure on the syringe plunger |
| Level III obstruction | Neither aspiration nor lavage of the sinus is possible: there is a complete blockage of the anastomosis |
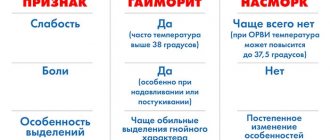
Differential diagnosis
For viral and bacterial MS, simultaneous damage to several sinuses ( polysinusitis ) is more typical.
Isolated damage to one sinus ( monosinusitis ) is typical of fungal and odontogenic rhinosinusitis .
Signs of rhinosinusitis caused by typical pathogens (S. pneumoniae and H. influenzae) are a decrease in the sense of smell, the presence of a fluid level on the X-ray and the effectiveness of traditional therapy.
Distinctive features of rhinosinusitis caused by other microorganisms: foul-smelling nasal discharge, a total decrease in pneumatization of the paranasal sinuses on X-ray, slower positive dynamics of the X-ray picture during treatment.
Allergic (or eosinophilic) fungal rhinosinusitis is characterized by the detection of multiple polyps during endoscopy, as well as a very characteristic discharge of yellow, green or brown color with a very viscous rubber-like consistency. A similar discharge - allergic mucin - is found in all affected sinuses during surgery.
Odontogenic sinusitis usually acquires a primarily chronic course, accompanied by the formation of polyps, granulations or fungal stones in the sinus.
The chronic invasive form of mycosis is accompanied by the formation of fungal granulomas with their invasion into bone structures and soft tissues of the face.
Polypous rhinosinusitis is characterized by the formation and recurrent growth of polyps, consisting predominantly of edematous tissue infiltrated with eosinophils.
Complications of sinusitis
The course of sinusitis can be benign if the disease is detected and treated in time. The acute form is usually treated with conservative methods. In case of a chronic course, it is necessary to consider surgical elimination of the causes of inflammation: removal of the polyp, septoplasty (for deformation of the septum) and other types of surgical assistance.
In severe or untreated cases, inflammation can develop in nearby structures, for example, with frontal phlegmon or abscess of the soft tissues of the face. With sinusitis, a “breakthrough” of inflammation into the orbit may occur. Which then leads to irreversible vision defects.
If sinusitis leads to infection in the brain, this can lead to meningitis, encephalitis and abscesses. As a result, lifelong neurological disorders may occur: paralysis, seizures, etc.
Sinusitis can cause various complications. Although they are quite rare, without proper and timely treatment, dangerous consequences are inevitable.
General principles of treatment
The main goals of treatment for rhinosinusitis are:
- Reducing the duration of the disease.
- Prevention of the development of orbital and intracranial complications.
- Eradication of the pathogen.
From this perspective, the basic method of treating acute bacterial rhinosinusitis (moderate and severe forms) and exacerbation of chronic rhinosinusitis is empirical antibacterial therapy.
The main indications for prescribing antimicrobial drugs include:
- Anamnesis characteristic of rhinosinusitis.
- Severity of clinical manifestations.
- The presence of purulent discharge in the nasal passages.
Antibacterial therapy, taking into account the type and sensitivity of a specific pathogen identified during a bacteriological study, does not at all guarantee success due to the high probability of “traveling” microflora entering the test material during sampling. In addition, the results of in vitro sensitivity studies of the identified microorganism do not always correlate with the clinical effectiveness of individual antibacterial drugs. The reasons for this may be a significant increase in antibacterial activity as a result of the unidirectional effect of the antibiotic and its metabolite and the ability to specifically achieve bactericidal concentrations precisely at the site of infection.
Antibacterial therapy for acute bacterial rhinosinusitis
On an outpatient basis, oral antimicrobial drugs are predominantly prescribed.
Taking into account the spectrum of typical pathogens and Russian data on their antibiotic resistance, the drug of first choice for acute bacterial rhinosinusitis is amoxicillin.
In the absence of a noticeable clinical effect, after three days the drug should be replaced with an antibiotic active against penicillin-resistant S. pneumonia and β-lactamase-producing H. influenzae. In this case, III-IV generation cephalosparins or new fluoroquinolones are prescribed.
If you are intolerant to penicillin drugs (and due to possible cross-allergic reactions, cephalosporins should also not be prescribed), the drugs of choice are macrolides.
If the patient is hospitalized, the parenteral route of administration of antimicrobial drugs is preferable.
Antibacterial therapy for exacerbations of chronic rhinosinusitis
When treating exacerbations of chronic rhinosinusitis, oral amoxicillin/clavulanate is considered the drug of choice.
Alternative drugs (prescribed in case of ineffectiveness of the antimicrobial drugs of choice) currently include fluoroquinolones of the III-IV generations. In patients under 16 years of age, alternative drugs include macrolides. Considering the significant role of obstruction of the natural openings of the paranasal sinuses in the pathogenesis of rhinosinusitis, vasoconstrictor drugs, which are prescribed either locally or orally, are of great importance in its treatment.
In the treatment of acute and chronic rhinosinusitis, herbal medicines that have anti-inflammatory and mucolytic effects are also used.
Puncture and probing of the paranasal sinuses
These methods allow you to rinse the affected sinus with an antiseptic solution, remove pathological secretions from it, and administer medications (antiseptics, proteolytic enzymes, glucocorticosteroids). In some cases, puncture and lavage of the paranasal sinuses can eliminate the blockade of its natural anastomosis. It is believed that regular removal of exudate during purulent rhinosinusitis protects local immune factors from proteolysis and increases the content of Ig and complement in the affected sinus by 2-3 times, stimulating the mechanisms of local antibacterial defense. The most common and easier to perform is puncture of the maxillary sinus. It is most often used in the treatment of rhinosinusitis.
Forced drainage method
The method has certain advantages over treatment with repeated punctures. The presence of a catheter creates an additional path for evacuating secretions from the affected sinus, increases air exchange, and eliminates negative pressure when the natural anastomosis is blocked or acts as a valve.
Other methods
Nasal showers, rinsing the nasal cavity with a warm isotonic solution and physiotherapy (ultrahigh-frequency currents, microwave therapy, ultrasound).
Surgery
Indications for surgical treatment for bacterial rhinosinusitis arise when antibiotic therapy is ineffective and orbital or intracranial complications develop.
In surgical treatment, the prevailing trend is towards minimal invasiveness. Less traumatic functional endoscopic interventions give better results, are accompanied by fewer complications, and are less likely to contribute to the progression of the disease and the development of bronchial asthma than classical operations with radical removal of the mucous membrane and nasal turbinates.
Therapy for fungal forms of rhinosinusitis
For a fungal ball, antifungal medications are not prescribed. Treatment is surgical (endoscopic). Complete removal of fungal masses from the paranasal sinuses guarantees recovery. Treatment of allergic fungal rhinosinusitis is surgical (in the presence of large polyps). Treatment of superficial sinonasal mycosis involves removing the substrate for the growth of fungal mycelium.
How to cure sinusitis?
Before treatment for sinusitis begins, the diagnosis must be confirmed. Modern diagnostics may include: rhinoscopy (examination of the nose), sinus scanning (ultrasound examination of the sinuses), endoscopy. In severe cases, X-rays or CT scans may be needed.
Only an ENT doctor can offer an effective treatment regimen. Conservative treatment of the disease usually includes:
- antibiotic treatment - dosage and drug are prescribed exclusively by an ENT doctor. Even if after several days of treatment the symptoms of the disease begin to subside, you cannot interrupt the course of taking antibiotics.)
- taking antihistamines to eliminate swelling;
- local use of vasoconstrictor drops;
- rinsing the nasal passages with saline solutions;
- washing the sinuses in an ENT clinic (the “cuckoo” method and washing with a YAMIK catheter) are very effective in treating inflammation and clearing mucous masses;
- physiotherapeutic procedures in an ENT clinic.
If conservative therapy does not help, the doctor prescribes surgery. Typically, indications are frequent relapses of the disease, purulent or polypous sinusitis, odontogenic sinusitis.