Diseases of the rectum treatment in Rostov-on-Don : doctors of medical sciences, candidates of medical sciences, academicians, professors, corresponding members of the academy. Make an appointment, consultation, reviews, prices, addresses, detailed information. Make an appointment with a leading surgeon in Rostov-on-Don without waiting in line at a time convenient for you.
We also recommend:
Intimate surgeryConsultation with an abdominal surgeon
Kasatkin Vadim Fedorovich
Kasatkin Vadim Fedorovich Corresponding Member of the Russian Academy of Medical Sciences (RAMS), Professor, Doctor of Medical Sciences, surgeon, oncologist
More details
Kruglov Sergey Vladimirovich
Kruglov Sergey Vladimirovich Professor Doctor of Medical Sciences, surgeon of the highest qualification category, Honored Doctor of the Russian Federation.
More details
Burikov Maxim Alekseevich
Burikov Maxim Alekseevich Head of the surgical department - surgeon of the highest qualification category, candidate of medical sciences.
More details
Author of the article: Kutenko Vladimir Sergeevich.
Causes of proctitis
Proctitis
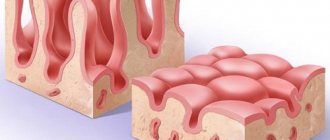
Microflora is present in the rectum of every person. When favorable conditions arise, these opportunistic microorganisms begin to actively multiply, which leads to the development of inflammation.
Inflammation can be triggered by poor nutrition - eating too many spicy foods, spices and significant doses of alcohol. Venous stagnation (impaired blood flow through the veins), observed with chronic constipation, also contributes to the development of proctitis. In addition, with constipation, hard feces often injure the rectal mucosa, which facilitates the penetration of infection.
The infection can enter the rectum from other areas of inflammation. Therefore, proctitis can be a complication of a number of intestinal diseases (ulcerative colitis, Crohn's disease, dysentery) or accompany diseases of the pelvic organs (cystitis, prostatitis, vaginitis).
The causative agents of inflammation of the rectal mucosa are often sexually transmitted infections (herpes, cytomegalovirus, chlamydia, trichomonas); proctitis can also be caused by pathogens of “classical” sexually transmitted diseases - gonorrhea and syphilis.
How common is rectal fistula?
The incidence in European countries is about 10-25 people per 100 thousand population. Mostly people of working age suffer from rectal fistulas. Men get sick 2-3 times more often than women.
Important! This disease, being benign, can dramatically reduce a person’s quality of life. A serious and most common complication of inadequate treatment of perianal fistulas is impaired holding function due to damage to the muscular apparatus of the anal canal.
Symptoms of proctitis
Proctitis can occur in both acute and chronic forms.
Acute proctitis has more severe symptoms, but is rare. The chronic form of proctitis is more common. Chronic proctitis can develop gradually, remaining unnoticed for a significant time.
Symptoms of acute proctitis
Acute proctitis begins suddenly and is manifested by a complex of rather severe symptoms:
- constant pain in the rectum. The pain may radiate to the lower back or perineal area;
- mucopurulent or bloody discharge;
- painful false urge to defecate (tenesmus);
- feeling of heaviness in the pelvis;
- sometimes there is an increase in temperature to 37.5-38°C.
Symptoms of chronic proctitis
Chronic proctitis can manifest itself with symptoms such as:
- periodic pain in the anus, rectum or left lower abdomen;
- mucus in stool;
- itching and burning in the anus.
Pain in the anus
The need for this article has been long overdue. She just begs to be on the page. The topic of pain in the anus is so relevant, so necessary, that there is no point in remaining silent. Let's get closer to the topic.
But, dear readers, this article is of a review, abstract nature. Its goal is to orient the patient in his actions. I recommend that anyone interested in their health in this area read thematic articles that reflect the essence of the problem in more detail.
There are quite a few different reasons that can cause pain in the anus.
First, let's highlight the cause of pain in the anus that is not directly related to the anus (anal canal and rectum).
There is such a medical term - proctalgia . It is literally translated as pain in the rectum. This pain is associated with problems in the nervous system. Occurs with osteochondrosis of the spine, intervertebral hernias, after stress. Most often, this pain is associated with tension in the levator ani muscle.
In fact, this is some kind of analogue of radiculitis and it is treated in the same way. When starting to treat proctalgia, it is necessary to exclude the presence of other diseases. An examination by a proctologist is mandatory.
Another periodically occurring variant of pain in the anus, weakly associated with the anus itself, is coccydynia - pain in the coccyx area. It can intensify when walking and putting pressure on the tailbone. This disease has many causes, both neurological and various others. Often in the history of coccydynia there are injuries to the coccyx area, sometimes even its fractures. Almost always, pain in the coccyx area was preceded by a fall on the butt.
What to do with coccydynia? Treatment in any case begins after examination by a proctologist. The doctor may prescribe an additional x-ray of the tailbone and recommend examination by other specialists, for example a neurologist. Treatment is mainly physiotherapeutic in nature. Some doctors perform blockades and recommend removing the coccyx, but such manipulations do not significantly alleviate the patient’s condition.
Now you can get closer to problems directly related to the anal canal and anus.
In first place in terms of frequency of occurrence is hemorrhoids ! And there is no escape from this. According to a study conducted by WHO, about 85% of the population periodically experience problems associated with hemorrhoids.
Just a few words about the essence of the disease. During the development of a human embryo, the formation of hemorrhoidal plexus veins occurs in the lower part of the rectum. Under the influence of certain factors, the veins of these plexuses expand and first internal and then external hemorrhoids are formed. Unfortunately, hemorrhoids can bother not only adults, but also children.
Dear readers, please note that hemorrhoids develop gradually. And you may never notice the onset of the disease. Someday you will notice discomfort in the anus, a feeling of incomplete emptying after stool, and slight itching in the anus. In most cases, these are the initial manifestations of hemorrhoids! Uncomplicated hemorrhoids do not hurt!
Hemorrhoids can hurt in the following cases:
- Thrombosis of the external hemorrhoid. In the veins of the external hemorrhoidal plexus, blood coagulates, causing a blood clot and inflammation. This whole thing is starting to hurt. The greater the thrombosis, the stronger the pain.
- Prolapse of internal hemorrhoids. The nodes begin to fall out after stool in the third degree. The disease progresses: “bumps” then fall out when walking and with little effort. First they straighten themselves, then you need to straighten them with your hands. Pain during prolapse is usually moderate and goes away after reduction.
- Prolapse and thrombosis of internal hemorrhoids. The situation is serious, it hurts very much, requires urgent medical attention and qualified help.
Medicines in the treatment of hemorrhoids are necessary only to relieve inflammation. Unfortunately, drug treatment for hemorrhoids does not lead to the disappearance of the disease. Hemorrhoids must be removed. Removal methods vary and correspond to different stages of the disease. We will not consider them here.
The second place among patients seeking treatment is currently occupied by sphincteritis . It has displaced the anal fissure, which is now in third place. Let me explain the essence of such a disease as sphincteritis - this is an inflammation of the structures of the anal canal. I will explain the details and details in another article (I will write a little later).
Sphincteritis itself occurs quite rarely. This requires severe digestive disorders: pancreatitis, peptic ulcer of the stomach and duodenum, long-term and persistent gastritis and duodenitis, stool disorders after taking antibiotics, irritable bowel syndrome, severe dysbiosis, infectious diseases and some other pathological conditions. Perhaps we can say that the butt with such diseases does not often bother you and severe pain does not happen often either. With successful treatment of the underlying disease, sphincteritis most often goes away.
But! There is one important BUT. All of the above is true if the patient does not have hemorrhoidal disease! Hemorrhoids are an “interesting” sore. Even doctors rarely pay attention to the very essence of the pathogenesis (development) of this disease. Hemorrhoids lead to hemodynamic disorders (blood stagnation) in the anal canal and nearby organs. This is especially pronounced with a sedentary lifestyle. And as a result of these congestion in the anus, many patients experience inflammation of the anal canal - sphincteritis - even without any digestive disorders. This inflammation is wavy in nature - periodically intensifies and weakens under the influence of many factors.
That is, hemorrhoids themselves tend to lead to inflammation of the anal canal and the appearance of pain, itching, discomfort and other unpleasant sensations. And if stool disorder also occurs (I described the most common causes above), then the situation becomes quite serious. And therefore, dear readers, you already understand that treating sphincteritis without removing hemorrhoids (if any) is unpromising. So we treat them together, and sometimes in turn.
We get to such an “interesting” disease as anal fissure, which also causes pain in the anus. Why did I put the word interesting in quotes? Yes, because anal fissure is quite difficult to treat. Currently, fissure is the third most common disease that causes pain in the anus.
The fissure is characterized by pain during bowel movements and for some time after it. At first, the pain is mild, and there may be some bleeding. Over time, the pain intensifies and can last for several hours. Blood discharge often decreases. Increased pain is associated with the development of scars around the crack and inflammation. Sentinel tubercles appear outside and inside. These are signs of the transition of an acute anal fissure to the chronic stage.
Chronic anal fissure, as a rule, does not heal with conservative (medicinal) treatment. Medical manipulation is required. The relationship here is simple: the older the crack, the more difficult the manipulation.
A very important point in the treatment of anal fissures: most often they appear in a pathologically changed anal canal against the background of other diseases (hemorrhoids, sphincteritis). It is difficult to treat such cracks.
Cryptitis is inflammation of the crypt (the exit of the anal gland into the rectum). The pain with cryptitis is intense, associated with stool, sometimes there is mucous or purulent discharge from the anus. The disease is relatively rare and is treated conservatively. I put cryptitis in fourth place only because cryptitis can lead to the next, more common problem.
Paraproctitis and rectal fistula . The diseases are not rare, but they are not that common. Acute paraproctitis is the initial stage of development of chronic paraproctitis (rectal fistula).
The essence of acute paraproctitis is perfectly described in the book “Fundamentals of Coloproctology” - “acute inflammation of the peri-rectal tissue, caused by the spread of the inflammatory process from the anal crypts and anal glands.” Simply put, pus accumulates in the anal glands. There is a lot of it and it is very “evil”. This pus needs to be released before it causes big trouble.
So, dear patients, if you have swelling, hardening, fever up to 38 degrees or higher, or pain in the anus, then go to a hospital where there is proctology. We'll have to have surgery urgently!
How can a non-specialist distinguish acute paraproctitis from thrombosis of the external hemorrhoid? It's complicated. If you have a high temperature, go to the hospital!
Rectal fistula . Almost always – the next stage of development of acute paraproctitis. The fistula itself does not cause pain; it is a pathological passage between the rectum and the surface of the body near the anus (sometimes quite far away). It happens that the fistula closes for some time (months, years), and then again festeres and behaves like acute paraproctitis. Only the inflammation is not as strong and the pain is less. Fistula can only be treated surgically in a hospital. Subcutaneous fistulas can be opened on an outpatient basis.
Epithelial coccygeal duct or pilonidal sinus . Essentially, this is a narrow cavity in the area of the sacrum and coccyx, formed when embryonic development is disrupted. You can live your whole life with this move and not know about it. If it becomes inflamed, pain occurs in the anus. But it hurts mainly in the tailbone area, and there is swelling there too. In case of acute inflammation, it is necessary to open it urgently. For chronic inflammation - a planned operation in the proctology department.
Stenosis (narrowing) of the anal canal . The essence of the problem is that the anus narrows and makes it difficult for feces to pass through. It goes without saying that bowel movements, especially if the stool is dense, can be painful. This condition can occur after operations on the anus, inflammation (sphincteritis, anal fissure), or with cancer of the anal canal. Children have congenital narrowing. We're talking about adults.
In case of inflammation of the anal canal, anal fissure - treatment of the corresponding disease. For anal cancer, treatment by an oncologist is necessary; timely diagnosis is very important.
Trauma (rupture) of the anal canal . Most often as a result of an accident or sexual activity. The patient’s actions depend on the intensity of the pain: the more painful it is, the faster you seek help. For minor pain, when there is a tear in the skin covering the anal canal (essentially an acute anal fissure), treatment is outpatient. In case of significant ruptures (rupture of the sphincter and even levators), urgent surgical intervention is required in the proctology department.
Anal cancer . The onset of the disease occurs with symptoms such as discomfort, secretion of mucus, blood, and anal itching. That is, the symptoms are common to various diseases of the rectum and anal canal, so early diagnosis is of primary importance in treating the disease.
Some other diseases may also be accompanied by pain in or near the anus: prostatitis, cysts, teratomas, osteomyelitis and some others. A description of these problems is beyond the scope of this article.
Sincerely, Vitaly Arkadyevich Ilyin , proctologist, candidate of medical sciences
Make an appointment Return to the list of publications
Methods for diagnosing proctitis
Since the manifestations of chronic proctitis are irregular and quite easily tolerated, they, as a rule, do not cause much concern and do not prompt you to consult a doctor. Meanwhile, without proper treatment, the disease progresses. Inflammation can spread to other parts of the intestine, to the tissue surrounding the rectum (paraproctitis), leading to the formation of scars that narrow the intestinal lumen and contribute to constipation.
Therefore, as soon as it becomes clear that there are some problems with the anus, you should definitely see a proctologist.
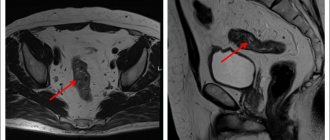
The diagnosis of proctitis is established on the basis of a proctological examination, during which the doctor performs a digital rectal examination. To confirm the diagnosis, instrumental diagnostic methods are used: anoscopy and sigmoidoscopy. A biopsy and laboratory tests are also performed.
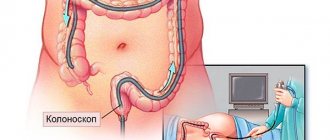
Sigmoidoscopy
Sigmoidoscopy is carried out using special endoscopic equipment, which allows the doctor to examine the condition of the walls of the rectum over a significant extent - up to 30 cm. Sigmoidoscopy requires preliminary preparation, since the intestines must be cleared of feces.
Biopsy
A biopsy is performed during sigmoidoscopy. Tissue from the rectal mucosa is taken for examination. A biopsy is performed for differential diagnosis with tumor processes.
Coprogram
Stool tests are being carried out. A coprogram (general stool analysis) allows you to determine the type of proctitis, identify digestive disorders and detect the presence of blood in the stool. Bacteriological analysis of stool is used to identify the pathogen that caused the inflammation.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Anesthesia and pain relief after surgery
The vast majority of surgical interventions for rectal fistulas are performed under subarachnoid or, as it is also called, spinal anesthesia. It refers to regional anesthesia methods that block the transmission of nerve impulses in a specific part of the body. A distinctive feature of any method of regional anesthesia is the minimum number of complications, in particular from the cardiovascular system, respiratory system, and brain. At the same time, you are conscious or, at your request, are in a superficial medicated sleep (sedation).
In the case of subarachnoid anesthesia during perineal surgery, the blockade of the nerve impulse occurs at the lumbosacral level. In our clinic, anesthesiologists and resuscitators prefer to perform a “saddle” block, which provides ideal anesthesia of the perineum with virtually no motor block, i.e. with preservation of motor function. If necessary, anesthesia can be supplemented with intravenous sedation. All this ensures maximum comfort for the patient and ideal working conditions for the surgeon.
If you are constantly taking a number of medications, for example, antihypertensives, those that affect blood clotting, or others, be sure to inform your anesthesiologist-resuscitator about this a few days before surgery.
Surgical interventions on the perineum can also be performed under general anesthesia.
After the operation, you will be prescribed pain relief as planned for several days, which can be easily done at home using tablets. These include local anesthetic drugs, intravenous analgesics and, in case of severe pain, potent drugs.
Treatment methods for proctitis
Treatment of proctitis includes the use of medications, diet and physical therapy. In case of complications, surgical treatment is performed.
Drug therapy
Treatment for proctitis involves the use of antibacterial therapy. Antibiotics are prescribed depending on what infection caused the inflammation.
Typically, patients are also prescribed medicinal enemas and baths. For this purpose, decoctions of medicinal herbs are used to relieve irritation in the intestines, eliminate inflammation and have an antiseptic effect. Rectal suppositories are also used.
Antispasmodics and antihistamines are used to relieve pain and spasms.
Diet correction
If you have proctitis, you should follow a special diet. Food should not be fatty, salty, hot, spicy or sour. In case of exacerbation, it is necessary to avoid eating fresh fruits and vegetables. Alcohol should not be consumed during illness.
Physiotherapy
For patients with proctitis, prolonged sitting is contraindicated: this leads to weakening of the pelvic muscles and congestion in the pelvis and legs. To speed up recovery, it is recommended to perform a set of exercises prescribed by your doctor.
More information about the treatment method
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
What complications can there be after surgery?
Currently, with the availability of standardized technology and an integrated approach to the diagnosis and treatment of rectal fistulas, unpleasant consequences are minimized. However, it should be noted that the risk of complications always exists.
The most serious complication after surgery for rectal fistulas is the development of anal incontinence. The risk of its occurrence is especially high during repeated interventions, when the anatomy is significantly changed and the holding function may be initially compromised. It is worth noting that when operations are performed by an experienced specialist who performs this type of intervention on an ongoing basis, the risk of incontinence is practically absent.
In addition, bleeding may develop both in the early postoperative period and several days after surgery. The nature and severity of the complication are determined only after examination. Stopping bleeding is usually possible in a dressing room. In some cases, repeat surgery may be required.
In addition, when treating complex and recurrent fistulas, due to pronounced scar changes, the sutures fixing the mucomuscular flap may diverge, which leads to inflammation in the wound and requires repeated interventions.
What is the likelihood of the disease returning?
The risk of disease relapse with complex, high fistulas is slightly higher than with simple intrasphincteric fistulas and depends on the type of fistula, its location, and the presence of previous surgical interventions. Treatment of recurrent fistulas is a particularly difficult task for a coloproctologist. Previous operations on the anal canal create gross cicatricial deformities, changing the anatomy and significantly impairing the function of retention, and a long course of the disease or inadequate previous treatment can lead to the formation of additional streaks and passages. In such conditions, planning of surgical intervention should be carried out after a full examination.
The success of the upcoming surgical intervention largely depends on a comprehensive assessment of the available data using various diagnostic methods and a mandatory conversation with the surgeon. An important factor is also the implementation of surgical intervention in a specialized hospital, where this type of treatment is based on world research data, their own many years of experience and is carried out by specialists who have successfully completed training and courses to improve their skills in treating this disease.
Important! The skill of a coloproctologist is judged all over the world by the ability to correctly operate anorectal fistulas, since since the existence of proctology, the treatment of fistulas has been and is now perhaps the most difficult section of diseases of the anorectal zone!