gormed.su
Diseases of the small intestine are so common that many patients treat them extremely lightly and are in no hurry to visit a doctor. This leads to the fact that, for the most part, people with already advanced pathologies are seen by a gastroenterologist. If you experience any symptoms related to the digestive organs, you should make an appointment with a doctor at the Professor Gorbakov Clinic. We receive treatment from the best specialists in this field.
The small intestine is the part of the gastrointestinal tract responsible for the basic processes of digestion. Topographically, it begins immediately after the stomach. The intestines are closely connected with organs such as the liver, gallbladder and pancreas. The small intestine consists of the duodenum, jejunum and ileum. Its loops are located in the upper abdomen.
The most common intestinal diseases are:
- duodenitis;
- duodenal ulcer
- enteritis;
- Crohn's disease;
- dysbacteriosis;
Symptoms of diseases of the small intestine
The main cause of pathologies of the small intestine is the failure of the digestive processes and insufficient intestinal absorption. Therefore, among the symptoms characteristic of these disorders, the following predominate:
- Stool disorder. It can manifest itself in the form of diarrhea or constipation. In severe pathology, traces of blood may appear in the stool and involuntary release of fatty, saturated feces.
- Abdominal pain of a pulling nature and moderate intensity. A distinctive feature is that it intensifies in the afternoon and decreases after defecation. If a patient complains of severe cramping pain, then in most cases we are talking about an inflammatory process in the intestines.
- Another characteristic symptom is bloating. In some cases, it may be accompanied by the sounds of rumbling and fluid transfusion in the abdomen. There is an increase in intensity at night. The body reacts especially acutely to the consumption of foods that cause increased gas formation.
- General clinical symptoms. These include weakness, sudden weight loss, hair loss, swelling and others.
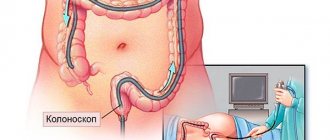
One of the most accurate methods for diagnosing diseases of the small intestine is the study of biopsies taken from the jejunum. They may indicate both the presence of inflammation and the formation of a tumor process. Typically, the sample is taken during a gastroscopy.
In addition, radiography is actively used, during which the swelling of the folds (or their smoothing) and hyperemia of the mucous membrane are clearly visible.
A biochemical blood test is also required; it shows an increase in alkaline phosphatase and active enterokinase, and in more severe forms, a decrease in enzyme activity.
A blood test is characterized by an increase in ROE and C-reactive protein, which indicates an inflammatory process. In addition, a study of the level of immunoglobulins and albumins is carried out.
In order to exclude the infectious nature of the disease, bacteriological and scatological examination of feces is carried out.
An ultrasound of the abdominal organs is performed to exclude concomitant pathologies.
Pharmacotherapy for diseases of the small intestine, the cost of which depends on the nature and stage of the disease, includes the following groups of drugs:
- Antibiotics. They are aimed at destroying pathological microflora and are used with drugs that restore intestinal biocenosis, such as bifidumbacterin or lactobacterin. Their combination with antifungal agents is possible.
- Glucocortecosteroids. They are used for severe disease and are aimed at improving regenerative processes.
- Enzyme preparations. Prescribed for increased acidity and functional failure of the pancreas and gall bladder.
- Medicines that help reduce hypoxia of the intestinal wall.
- Parenteral nutrition consisting of a mixture of amino acids and glucose solution.
- Bismuth preparations. Helps compact stool.
When treating diseases of the small intestine, it is important not only to follow all the doctor’s instructions, but also to follow a proper diet. Thus, it is possible to achieve long-term remission and tissue regeneration after the subsidence of the acute inflammatory process.
The use of butyric acid for radiation injuries of the intestine
One of the promising methods of drug prevention for maintaining remission in patients with UC is the use of the drug butyric acid and inulin, Zakofalka, as part of complex therapy (for example, in combination with mesalazine).
A decrease in the level of butyric acid in inflammatory bowel diseases (IBD) has been found in many studies, which served as the basis for studying the effectiveness of its use in IBD. One of the reasons for the decrease in butyric acid in patients with IBD is a significant decrease in the number of microbes that synthesize this metabolite. The state of mucosal and fecal microflora associated with it was studied in patients with Crohn's disease, ulcerative colitis and in healthy people. There is a sharp decrease in bacteria that synthesize butyric acid (in particular Faecalibacterium prausnitzii) both in the feces and in the colon mucosa in patients with IBD, compared with healthy individuals.
Application of Zakofalk as a means of enhancing primary therapy for the prevention of exacerbation of ulcerative colitis
justified by the decrease in the concentration of this metabolite in these patients and the main effects of butyric acid on the colon mucosa:
1. Anti-atrophic effect - restoration of trophism of the colon mucosa.
2. Anti-inflammatory effect. Restoring the barrier functions of the colon.
3. Regulation of the processes of normal maturation and development of cells in the colon mucosa.
4. Antidiarrheal effect – regulation of water and electrolyte balance in the colon.
5. Prebiotic effect – creating a favorable environment for the growth of your own beneficial microflora.
The effectiveness of Zakofalk has been confirmed in a large number of studies. Thus, in a large study conducted on the basis of 19 gastrocenters that are part of the IBD study group in Italy, patients with mild to moderate forms of ulcerative colitis (number of patients = 196), who did not achieve a satisfactory response to standard mesalazine therapy within 6 months Zakofalk was added 1 tablet 3 times a day. After 6 months, patients receiving a combination of mesalazine and Zakofalk showed a statistically significant decrease in the frequency of bowel movements, blood and mucus, as well as a reduction in the clinical activity index - 86% were in clinical remission (had no symptoms of the disease).
To prevent exacerbation (maintain remission) of ulcerative colitis, Zakofalk in combination with the main therapy (mesalazine) is used 1 t 3-4 times a day, the minimum course is 3-6 months, maintenance therapy is possible 1 t 2 times a day for a long time.
Causes
- Intestinal infections. Intestinal infections most often cause acute inflammation of the jejunum. The leading role belongs to rotaviruses, enteroviruses, salmonella, and campylobacteria. In some cases, after suffering an acute intestinal infection, jejunitis becomes chronic. Chronicity of the process can be facilitated by helminthic infestation (giardiasis, ascariasis, strongyloidiasis).
- Nutritional factor. Errors in nutrition in themselves are not the cause of jeunitis, but they predispose to the onset of the disease. The development of jeunitis is facilitated by the predominance of high-carbohydrate foods in the diet, abuse of spicy seasonings, and dry food.
- Alcohol abuse. The toxic effect of alcohol on the mucous membrane causes functional disorders, thereby leading to the development of chronic jeunitis.
- Food allergies. The most allergenic are cow's milk, nuts, fish, and chocolate.
- Exposure to certain drugs and toxins. Mercury, phosphorus, lead, arsenic, and zinc have a toxic effect on the small intestine. The development of chronic jejunitis is facilitated by long-term treatment with non-steroidal anti-inflammatory drugs, cytostatics, and glucocorticosteroids.
- Ionizing radiation. Radiation enteritis, in most cases, develops during radiation therapy for malignant diseases of the pelvic and abdominal organs.
- Insufficiency of the major duodenal papilla. Due to insufficiency of the duodenal papilla, bile constantly leaks into the intestine, which contributes to the development of jeunitis.
- Previous operations on the gastrointestinal tract. In the development of jejunitis, operations on the stomach (resection, vagotomy, gastrostomy) are of greatest importance.
- Ischemia of the wall of the small intestine. Chronic ischemia disrupts the ability of the mucous membrane to regenerate and contributes to the occurrence of dystrophic changes in the jejunum.
- Concomitant pathology. Secondary jeunitis can develop against the background of other gastrointestinal diseases (with gastroduodenal ulcers, hepatitis, cirrhosis of the liver, diseases of the biliary tract, pancreas), with severe renal failure with the development of uremia; for eczema; psoriasis; endocrine pathology (diabetes mellitus, thyrotoxicosis); systemic connective tissue diseases; cardiovascular diseases; immunodeficiencies.
Symptoms
Acute colitis can be recognized by the following signs:
- bloating, flatulence;
- pain on palpation;
- rumbling;
- frequent loose stools, sometimes mixed with blood;
- decreased appetite;
- general signs of intoxication;
- elevated temperature;
- dehydration.
- In case of severe intoxication of the body, a change in the color of the tongue is observed - it becomes gray and becomes coated.
The chronic form of colitis is characterized by:
- frequent constipation and diarrhea;
- periodic aching pain in the abdomen, especially on the sides;
- pain before defecation;
- flatulence;
- weakness.
Enteritis
Acute form
Acute enteritis is treated in a hospital.
Acute toxic enteritis is treated in gastroenterology departments; infectious enteritis is an indication for hospitalization in an infectious disease ward. Patients are prescribed bed rest, dietary nutrition (mechanically and chemically gentle food, limiting the content of carbohydrates and fats), drinking plenty of fluids (if necessary, hydration therapy measures), symptomatic and restorative treatment. With the development of severe dysbacteriosis, drug correction of the intestinal flora is carried out, and diarrhea is stopped with astringents. In case of protein metabolism disturbance, polypeptide solutions are administered. Treatment of acute enteritis usually takes about a week; discharge from the hospital is carried out after acute symptoms subside.
Patients with severe enteritis, as well as enteritis of toxic origin (the further course of which is difficult to determine in the first hours of the disease) must be hospitalized. Patients with infectious enteritis are hospitalized in infectious diseases hospitals.
Chronic form
It is advisable to treat exacerbation of chronic enteritis in a hospital setting. Patients are prescribed bed rest and dietary nutrition (diet No. 4). During the acute period, food should be as rich in proteins as possible; it is better to limit fats and carbohydrates. It is necessary to avoid rough foods, spicy, sour foods, and foods that can damage the mucous membrane of the digestive tract. Avoid foods containing large amounts of fiber and milk. The amount of fats and carbohydrates is gradually increased.
During the period of remission, a balanced diet is recommended, containing all the necessary substances, vitamins and minerals in sufficient quantities. Correction of digestive enzyme deficiency is carried out using enzyme preparations: pancreatin, pancitrate, festal. Stimulate absorption with drugs containing nitrates, preferably long-acting. Protective agents (essential phospholipids, milk thistle fruit extract) help restore the functionality of the cell membranes of the intestinal epithelium.
Loperamide is prescribed to suppress excessive propulsive bowel movements. For patients with severe diarrhea, astringents, enveloping and absorbent drugs, and antiseptics are recommended. Herbal medicine can be used for these purposes (decoctions of chamomile, sage, St. John's wort, bird cherry and blueberry fruits, alder cones).
Dysbacteriosis is corrected with the help of probiotics and eubiotics. Intravenous infusion of amino acid solutions is prescribed for severe absorption disorders with severe protein deficiency. If symptoms of enteritis develop against the background of small intestinal tumors (polyps, diverticula), their surgical removal is necessary.
Classification
By etiology
1. Primary:
- infectious;
- toxic;
- parasitic;
- allergic;
- medicinal;
- radial;
- nutritional;
- postoperative;
- congenital intestinal anomalies and fermentopathy;
- with insufficiency of the duodenal papilla.
2. Secondary (occurs against the background of other diseases).
By the nature of morphological changes
- without atrophy;
- with moderate partial villous atrophy;
- with subtotal villous atrophy.
According to the clinical course
In relation to chronic jeunitis:
- mild course;
- moderate course;
- severe course.
Diet for intestinal diseases
In addition to medications, diet is an important component of therapy. Without it, coping with the disease and returning to a normal lifestyle is quite difficult. The diet should consist of seasonal vegetables and fruits, lean meat and fish, steamed, baked or boiled, as well as fermented milk products.
The following should be completely excluded from the menu:
- Fast food;
- Fatty, spicy and fried foods;
- Legumes;
- Canned food, sauces;
- Carbonated drinks.
Experienced medical doctors know how to treat intestinal inflammation quickly and effectively. After seeing a gastroenterologist, you can immediately take the necessary tests; the clinic’s prices are affordable for everyone. You can make an appointment or find out more information on the website or by calling the 24-hour hotline +7 (863) 333-20-11.