Paired small glands to the right and left of the uterus, in which eggs develop and female sex hormones are produced, are called ovaries. The appearance of pain in them may indicate the development of pathology in the reproductive system, so it is very important to determine why the ovaries hurt using modern diagnostic methods.
Uterine appendages - what are they?
The content of the article
The appendages, that is, the ovaries and fallopian tubes, belong to the pelvic organs. They are located symmetrically on the right and left sides of the uterus. Inflammation of the appendages usually begins with inflammation of the fallopian tubes. Due to the close proximity of the appendages, inflammation of the ovaries quickly occurs. Because of this location, inflammation of the ovaries and fallopian tubes is not usually identified as separate disease entities.
Pelvic inflammatory disease (PID) is most often diagnosed in young, actively sexual women. The symptoms are annoying, and neglect of treatment can lead to the development of a chronic form of the disease and serious complications, including infertility.
Treatment of inflammatory diseases of the pelvic organs in women
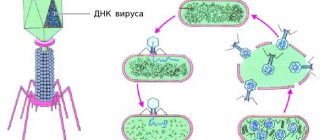
Pelvic inflammatory diseases (PID) are characterized by various manifestations depending on the level of damage and the strength of the inflammatory response. The disease develops when a pathogen (enterococci, bacteroides, chlamydia, mycoplasma, ureaplasma, trichomonas) penetrates into the genital tract and in the presence of favorable conditions for its development and reproduction. These conditions occur during the postpartum or post-abortion period, during menstruation, during various intrauterine manipulations (insertion of an IUD, hysteroscopy, hysterosalpingography, diagnostic curettage) [1, 5].
Existing natural protective mechanisms, such as anatomical features, local immunity, the acidic environment of the vaginal contents, the absence of endocrine disorders or serious extragenital diseases, can in the vast majority of cases prevent the development of genital infection. In response to the invasion of a particular microorganism, an inflammatory response occurs, which, based on the latest concepts of the development of the septic process, is usually called a “systemic inflammatory response” [16, 17, 18].
Acute endometritis always requires antibacterial therapy. The basal layer of the endometrium is affected by the inflammatory process due to the invasion of specific or nonspecific pathogens. Endometrial protective mechanisms, congenital or acquired, such as T-lymphocyte aggregates and other elements of cellular immunity, are directly related to the action of sex hormones, especially estradiol, act in conjunction with the macrophage population and protect the body from damaging factors. With the onset of menstruation, this barrier on a large surface of the mucous membrane disappears, which makes it possible to become infected. Another source of protection in the uterus is the infiltration of the underlying tissues with polymorphonuclear leukocytes and the rich blood supply of the uterus, which promotes adequate perfusion of the organ with blood and nonspecific humoral protective elements contained in its serum: transferrin, lysozyme, opsonins [16].
The inflammatory process can spread to the muscle layer: then metroendometritis and metrothrombophlebitis occur with a severe clinical course. The inflammatory reaction is characterized by a disorder of microcirculation in the affected tissues, expressed by exudation; with the addition of anaerobic flora, necrotic destruction of the myometrium can occur [12].
Clinical manifestations of acute endometritis are characterized already on the 3rd–4th day after infection by an increase in body temperature, tachycardia, leukocytosis and an increase in ESR. Moderate enlargement of the uterus is accompanied by pain, especially along its ribs (along the blood and lymphatic vessels). Purulent-bloody discharge appears. The acute stage of endometritis lasts 8–10 days and requires quite serious treatment. With proper treatment, the process is completed, less often it turns into subacute and chronic forms, and even less often, with independent and indiscriminate antibiotic therapy, endometritis can take a milder abortive course [5, 12].
Treatment of acute endometritis, regardless of the severity of its manifestations, begins with antibacterial infusion, desensitizing and restorative therapy.
Antibiotics are best prescribed taking into account the sensitivity of the pathogen to them. The dosage and duration of antibiotic use are determined by the severity of the disease. Due to the frequency of anaerobic infections, additional use of metronidazole is recommended. Considering the very rapid course of endometritis, cephalosporins with aminoglycosides and metronidazole are preferable among antibiotics. For example, cefamandole (or cefuroxime, cefotaxime) 1.0–2.0 g 3–4 times a day IM or IV drip + gentamicin 80 mg 3 times a day IM + Metrogyl 100 ml IV /in drip.
Instead of cephalosporins, you can use semi-synthetic penicillins (for abortive cases), for example, ampicillin 1.0 g 6 times a day. The duration of such combination antibacterial therapy depends on the clinic and laboratory response, but should not be less than 7–10 days. To prevent dysbacteriosis from the first days of antibiotic treatment, use nystatin 250,000 units 4 times a day or Diflucan 50 mg/day for 1–2 weeks orally or intravenously [5].
Detoxification infusion therapy may include a number of infusion agents, for example, Ringer-Locke solution - 500 ml, polyionic solution - 400 ml, hemodez (or polydesis) - 400 ml, 5% glucose solution - 500 ml, 1% calcium chloride solution - 200 ml, Unithiol with a 5% solution of ascorbic acid, 5 ml 3 times a day. In the presence of hypoproteinemia, it is advisable to carry out infusions of protein solutions (albumin, protein), blood replacement solutions, plasma, red blood cells or whole blood, and amino acid preparations [12].
Physiotherapeutic treatment occupies one of the leading places in the treatment of acute endometritis. It not only reduces the inflammatory process in the endometrium, but also stimulates ovarian function. When normalizing the temperature reaction, it is advisable to prescribe low-intensity ultrasound, inductothermy with an HF or UHF electromagnetic field, magnetic therapy, and laser therapy.
Every fifth woman who has suffered salpingo-oophoritis is at risk of infertility. Adnexitis can cause a high risk of ectopic pregnancy and pathological course of pregnancy and childbirth. The fallopian tubes are the first to be affected, and the inflammatory process can involve all layers of the mucous membrane of one or both tubes, but more often only the mucous membrane of the tube is affected, and catarrhal inflammation of the mucous membrane of the tube occurs - endosalpingitis. Inflammatory exudate, accumulating in the tube, often flows through the ampullary opening into the abdominal cavity, adhesions form around the tube and the abdominal opening of the tube closes. A saccular tumor develops in the form of a hydrosalpinx with transparent serous contents or in the form of a pyosalpinx with purulent contents. Subsequently, the serous exudate of the hydrosalpinx resolves as a result of treatment, and the purulent pyosalpinx can perforate into the abdominal cavity. The purulent process can capture and melt increasingly large areas of the pelvis, spreading to all internal genitalia and nearby organs [9, 10, 13].
Inflammation of the ovaries (oophoritis) as a primary disease is rare; infection occurs in the area of the ruptured follicle, since the rest of the ovarian tissue is well protected by the covering germinal epithelium. In the acute stage, swelling and small cell infiltration are observed. Sometimes, in the cavity of the follicle of the corpus luteum or small follicular cysts, ulcers and microabscesses form, which, merging, form an ovarian abscess or pyovarium. In practice, it is impossible to diagnose an isolated inflammatory process in the ovary, and this is not necessary. Currently, only 25–30% of patients with acute adnexitis have a pronounced picture of inflammation; the remaining patients experience a transition to a chronic form, when therapy is stopped after a rapid subsidence of the clinic.
Acute salpingoophoritis is also treated with antibiotics (preferably third generation fluoroquinolones - Ciprofloxacin, Tarivid, Abaktal), since it is often accompanied by pelvioperitonitis - inflammation of the pelvic peritoneum.
Inflammation of the pelvic peritoneum most often occurs secondary to the penetration of infection into the abdominal cavity from an infected uterus (with endometritis, infected abortion, ascending gonorrhea), from the fallopian tubes, ovaries, from the intestines, with appendicitis, especially with its pelvic location. In this case, an inflammatory reaction of the peritoneum is observed with the formation of serous, serous-purulent or purulent effusion. The condition of patients with pelvioperitonitis remains either satisfactory or moderate. The temperature rises, the pulse quickens, but the function of the cardiovascular system is slightly impaired. With pelvioperitonitis, or local peritonitis, the intestine remains unbloated, palpation of the upper half of the abdominal organs is painless, and symptoms of peritoneal irritation are determined only above the pubis and in the iliac regions. However, patients note severe pain in the lower abdomen, there may be retention of stool and gas, and sometimes vomiting. The level of leukocytes is increased, the formula shifts to the left, the ESR is accelerated. Gradually increasing intoxication worsens the condition of patients [14, 15].
Treatment of salpingoophoritis with or without pelvioperitonitis begins with a mandatory examination of the patient for flora and sensitivity to antibiotics. The most important thing is to determine the etiology of inflammation. Today, benzylpenicillin is widely used for the treatment of specific gonorrheal process, although drugs such as Rocephin, Cephobid, Fortum are preferable.
The “gold standard” in the treatment of salpingoophoritis from antibacterial therapy is the prescription of Claforan (cefotaxime) at a dose of 1.0–2.0 g 2–4 times a day intramuscularly or one dose of 2.0 g intravenous in combination with gentamicin 80 mg 3 times/day (gentamicin can be administered once at a dose of 160 mg IM). It is imperative to combine these drugs with the administration of Metrogyl IV 100 ml 1-3 times a day. A course of antibiotic treatment should be carried out for at least 5–7 days, prescribing cephalosporins of the second and third generations (Mandol, Zinacef, Rocephin, Cephobid, Fortum and others at a dose of 2–4 g/day) [14].
In case of acute inflammation of the uterine appendages, complicated by pelvioperitonitis, oral administration of antibiotics is possible only after the main course, and only if the need arises. As a rule, there is no such need, and the persistence of previous clinical symptoms may indicate the progression of inflammation and a possible suppurative process.
Detoxification therapy is mainly carried out with crystalloid and detoxification solutions in an amount of 2–2.5 liters with the inclusion of solutions of hemodez, Reopoliglyukin, Ringer-Locke, polyionic solutions - acessol, etc. Antioxidant therapy is carried out with a solution of Unithiol 5.0 ml with a 5% solution of ascorbic acid 3 times/day i.v. [14].
In order to normalize the rheological and coagulation properties of blood and improve microcirculation, acetylsalicylic acid (Aspirin) 0.25 g/day is used for 7–10 days, as well as intravenous administration of Reopoliglucin 200 ml (2–3 times per course). Subsequently, a whole complex of resorption therapy and physiotherapeutic treatment is used (calcium gluconate, autohemotherapy, sodium thiosulfate, Humisol, Plazmol, Aloe, FiBS) [3, 15]. Among the physiotherapeutic procedures for acute processes, ultrasound is appropriate, providing analgesic, desensitizing, fibrolytic effects, enhancing metabolic processes and tissue trophism, inductothermy, UHF therapy, magnetic therapy, laser therapy, and later - sanatorium-resort treatment.
Among 20–25% of inpatients with inflammatory diseases of the uterine appendages, 5–9% develop purulent complications requiring surgical interventions [9, 13].
The following provisions regarding the formation of purulent tubo-ovarian abscesses can be highlighted:
- chronic salpingitis in patients with tubo-ovarian abscesses is observed in 100% of cases and precedes them;
- the spread of infection occurs predominantly through the intracanalicular route from endometritis (with IUD, abortion, intrauterine interventions) to purulent salpingitis and oophoritis;
- frequent combination of cystic transformations in the ovaries with chronic salpingitis;
- there is a mandatory combination of ovarian abscesses with exacerbation of purulent salpingitis;
- Ovarian abscesses (pyovarium) are formed mainly from cystic formations, often microabscesses merge with each other.
Morphological forms of purulent tubo-ovarian formations:
- pyosalpinx - predominant lesion of the fallopian tube;
- pyovarium - predominant damage to the ovary;
- tubo-ovarian tumor.
All other combinations are complications of these processes and can occur:
- without perforation;
- with perforation of ulcers;
- with pelvioperitonitis;
- with peritonitis (limited, diffuse, serous, purulent);
- with pelvic abscess;
- with parametritis (posterior, anterior, lateral);
- with secondary lesions of adjacent organs (sigmoiditis, secondary appendicitis, omentitis, interintestinal abscesses with the formation of fistulas).
Clinically differentiating each of these localizations is almost impossible and impractical, since the treatment is fundamentally the same; antibacterial therapy takes a leading place both in the use of the most active antibiotics and in the duration of their use. The basis of purulent processes is the irreversible nature of the inflammatory process. Irreversibility is due to morphological changes, their depth and severity, often accompanying severe renal dysfunction [3, 9].
Conservative treatment of irreversible changes in the uterine appendages is unpromising, since if it is carried out, it creates the preconditions for the occurrence of new relapses and aggravation of impaired metabolic processes in patients, increases the risk of upcoming surgery in terms of damage to adjacent organs and the inability to perform the required volume of surgery [9].
Purulent tubo-ovarian formations represent a difficult diagnostic and clinical process. Nevertheless, a number of characteristic syndromes can be identified:
- intoxication;
- painful;
- infectious;
- early renal;
- hemodynamic disorders;
- inflammation of adjacent organs;
- metabolic disorders.
Clinically, intoxication syndrome manifests itself in intoxication encephalopathy, headaches, heaviness in the head and severity of the general condition. Dyspeptic disorders (dry mouth, nausea, vomiting), tachycardia, and sometimes hypertension (or hypotension in the onset of septic shock, which is one of its early symptoms along with cyanosis and facial hyperemia against the background of severe pallor) are noted [4].
Pain syndrome is present in almost all patients and is of an increasing nature, accompanied by a deterioration in general condition and well-being, there is pain during a special examination, displacement behind the cervix and symptoms of irritation of the peritoneum around the palpable formation. Pulsating increasing pain, persistent fever with a body temperature above 38°C, tenesmus, loose stools, lack of clear contours of the tumor, lack of effect from treatment - all this indicates the threat of perforation or its presence, which is an absolute indication for urgent surgical treatment. The infectious syndrome is present in all patients, manifested in the majority by high body temperature (38°C and above), tachycardia corresponds to fever, as well as an increase in leukocytosis, ESR and leukocyte index of intoxication increase, the number of lymphocytes decreases, the shift of white blood to the left and the number of molecules of average mass, reflecting increasing intoxication. Often there is a change in kidney function due to impaired urine passage. Metabolic disorders manifest themselves in dysproteinemia, acidosis, electrolyte imbalance, etc.
The treatment strategy for this group of patients is based on organ-preserving principles of surgery, but with radical removal of the main source of infection. Therefore, for each specific patient, the volume of the operation and the time of its implementation should be optimal. Clarifying the diagnosis sometimes takes several days - especially in cases where there is a borderline variant between suppuration and an acute inflammatory process or in differential diagnosis from an oncological process. Antibacterial therapy is required at each stage of treatment [1, 2].
Preoperative therapy and preparation for surgery include:
- antibiotics (use Cefobid 2.0 g/day, Fortum 2.0–4.0 g/day, Reflin 2.0 g/day, Augmentin 1.2 g IV drip 1 time/day, Clindamycin 2.0– 4.0 g/day, etc.). They must be combined with gentamicin 80 mg IM 3 times a day and Metrogyl infusion 100 ml IV 3 times;
- detoxification therapy with infusion correction of volemic and metabolic disorders;
- mandatory assessment of the effectiveness of treatment based on the dynamics of body temperature, peritoneal symptoms, general condition and blood counts.
The surgical stage also includes ongoing antibacterial therapy. It is especially valuable to administer one daily dose of antibiotics on the operating table immediately after the end of the operation. This concentration is necessary as a barrier to further spread of infection, since penetration into the area of inflammation is no longer prevented by dense purulent capsules of tubo-ovarian abscesses. Betalactam antibiotics (Cephobid, Rocephin, Fortum, Claforan, Tienam, Augmentin) pass these barriers well.
Postoperative therapy includes the continuation of antibacterial therapy with the same antibiotics in combination with antiprotozoal, antimycotic drugs and uroseptics in the future (according to sensitivity). The course of treatment is based on the clinical picture and laboratory data, but should not be less than 7–10 days. Antibiotics are discontinued based on their toxic properties, so gentamicin is often discontinued first, after 5–7 days, or replaced with amikacin.
Infusion therapy should be aimed at combating hypovolemia, intoxication and metabolic disorders. Normalization of gastrointestinal motility is very important (intestinal stimulation, HBOT, hemosorption or plasmapheresis, enzymes, epidural blockade, gastric lavage, etc.). Hepatotropic, restorative, antianemic therapy is combined with immunostimulating therapy (UVR, laser blood irradiation, immunocorrectors) [2, 9, 11].
All patients who have undergone surgery for purulent tubo-ovarian abscesses require post-hospital rehabilitation in order to prevent relapses and restore specific body functions.
Literature
- Abramchenko V.V., Kostyuchek D.F., Perfileva G.N. Purulent-septic infection in obstetric and gynecological practice. St. Petersburg, 1994. 137 p.
- Bashmakova M. A., Korkhov V. V. Antibiotics in obstetrics and perinatology. M., 1996. No. 9. P. 6.
- Bondarev N. E. Optimization of diagnosis and treatment of mixed sexually transmitted diseases in gynecological practice: abstract. dis. ...cand. honey. Sci. St. Petersburg, 1997. 20 p.
- Ventsela R.P. Nosocomial infections // M., 1990. 656 p.
- Gurtovoy B. L., Serov V. N., Makatsaria A. D. Purulent-septic diseases in obstetrics. M., 1981. 256 p.
- Keith L. G., Berger G. S., Edelman D. A. Reproductive health: Vol. 2 // Rare infections. M., 1988. 416 p.
- Krasnopolsky V.I., Kulakov V.I. Surgical treatment of inflammatory diseases of the uterine appendages. M., 1984. 234 p.
- Korkhov V.V., Safronova M.M. Modern approaches to the treatment of inflammatory diseases of the vulva and vagina. M., 1995. No. 12. P. 7–8.
- Kumerle X. P., Brendel K. Clinical pharmacology during pregnancy / ed. X. P. Kumerle, K. Brendel: trans. from English T. 2. M., 1987. 352 p.
- Serov V.N., Strizhakov A.N., Markin S.A. Practical obstetrics: a guide for doctors. M., 1989. 512 p.
- Serov V.N., Zharov E.V., Makatsaria A.D. Obstetric peritonitis: diagnosis, clinic, treatment. M., 1997. 250 p.
- Strizhakov A. N., Podzolkova N. M. Purulent inflammatory diseases of the uterine appendages. M., 1996. 245 p.
- Khadzhieva E. D. Peritonitis after cesarean section: a textbook. St. Petersburg, 1997. 28 p.
- Sahm DE The role of automation and molecular technology in antimicrobial susceptibility testing // Clin. Microb. And Inf. 1997; 3: 2(37–56).
- Snuth CB, Noble V., Bensch R. et al. Bacterial flora of the vagina during the mensternal cycle // Ann. Intern. Med. 1982; p. 948–951.
- Tenover FC Norel and emerging mechanisms of antimicrobial resistance in nosocomial pathogens // Am. J. Med. 1991; 91, p. 76–81.
V. N. Kuzmin, Doctor of Medical Sciences, Professor MGMSU, Moscow
Causes of inflammation of the appendages
There are two possibilities for the development of infection: ascending and descending spread. The first method is preferred by anaerobic bacteria, colon bacilli, streptococci, staphylococci and chlamydia. The vagina is not free of bacteria and is home to many germs. This is the potential start of an upward pathway for bacteria.
Then they pass through the mouth of the cervical canal and provoke inflammation of the mucous membrane of the uterine cavity. It is only a matter of time before they enter the fallopian tube and cause inflammation of the appendages.
Bacteria can also enter the upper region of the reproductive system, penetrating the absorptive spaces of the cervical canal and reaching the appendages through the lymph.
Normally, bacteria have a complex penetration process, which was described above. For this there must be special conditions. Firstly, there must be a nutrient medium for pathogenic bacteria (blood, secretions). Secondly, a gateway for infection is needed, for example, a damaged mucous membrane.
There are a number of factors predisposing to the occurrence of infection through an ascending route:
- period of bleeding from the uterine cavity - menstruation;
- miscarriage;
- childbirth, postpartum period;
- performing cleaning (curettage);
- performing hysteroscopy;
- hysterosalpingography;
- installation of an intrauterine device.
Descending infection develops differently: bacteria enter the appendages through the blood. In this case, the source of origin of microbes is located in a completely different organ. Another possibility is infection, for example, from an inflamed appendix sticking to the appendages.
Diagnostics
With this disease, the symptoms are quite vague. The acute form of ovarian inflammation is similar in its symptoms to the manifestations of an acute abdomen in various diseases: ectopic pregnancy, appendicitis, ovarian cyst, peritonitis.
As a result, making a correct diagnosis is often difficult. For the highest reliability, the results of the following analyzes are used:
- ultrasound diagnostics.
- bacteriological examination.
- hysterosalpingoscopy (detection of gross anatomical changes in the fallopian tubes that can occur during chronic inflammation of the ovaries).
- Laparoscopy is the most informative diagnostic method.
- gynecological history data (this includes information about the presence of previous inflammation of the uterus and appendages, STIs, complicated childbirth, abortion, diagnostic intrauterine procedures).
- laboratory tests (increased levels of leukocytes in urine and blood tests, smears of the urethra and vagina).
- gynecological examination (pain and enlargement of the ovaries, impaired mobility of the uterine appendages).
Inflammation of the appendages - symptoms
Symptoms of adnexitis depend on the type of disease. Most often they appear immediately after obstetric and gynecological procedures or uterine bleeding. The condition of acute adnexitis is characterized by high fever and malaise.
The most annoying symptom is pain in the lower abdomen. It is acute in nature, and its severity can be so significant that some patients cannot touch the sore spot. Sometimes symptoms from other organs occur.
During inflammation of the pelvic organs, an abscess develops, occupying the Douglas cavity. Swelling and swelling can put pressure on the rectum, causing diarrhea, constipation, and even intestinal obstruction. The mucous membrane of the uterine cavity, affected by the inflammatory process, gives other symptoms - blood or pus coming out of the cervical canal.
If the inflammatory process is not sufficiently treated, subacute or chronic adnexitis may develop. Then the symptoms will be less turbulent. Pain in the lower abdomen occurs to a lesser extent - in chronic conditions it is nagging, pain more often appears during physical activity and sexual intercourse. Body temperature is less high.
Tumor of the left ovary
In recent years, women have increasingly encountered such a pathological process as a tumor of the left ovary.
A few decades ago, a tumor of the left ovary was diagnosed mainly in women of the older age group (50-60 years old); nowadays, such a tumor is often diagnosed at a young age, and it is not uncommon for tumors to form in girls during puberty. A tumor of the left ovary is a rather insidious disease, practically asymptomatic, accompanied by hormonal imbalances, has a detrimental effect on reproductive function, and often leads to its complete loss. And untimely treatment or lack thereof can lead to death.
Complications after inflammation of the appendages
Inflammation of the appendages can lead to many complications associated with suppuration and the subsequent transition of the disease process to the peritoneum, covering the pelvis and abdomen. There is a risk of developing a condition of peritonitis (local or diffuse).
The inflamed structures, together with neighboring organs, form a so-called inflammatory tumor, which should be operated on after acute symptoms have resolved.
Other complications of adnexitis:
- fallopian tube abscess;
- ovarian abscess;
- ovarian-fallopian abscess;
- Douglas cavity abscess;
- rupture of abscesses and formation of fistulas;
- inflammation of the uterus;
- fallopian tube cyst;
- fallopian tube hematoma;
- adhesions in the pelvis;
- infertility due to inflammation of the fallopian tubes, which makes transporting the egg impossible, as adhesions form, which obstruct the tube.
A complication of adnexitis during pregnancy is ectopic pregnancy in the fallopian tubes - a fertilized egg cannot enter the uterine cavity due to post-inflammatory changes in the mucous membrane of the fallopian tube and implantation of the embryo in an unsuitable place.
Prevention
Properly organized professional prevention of ovarian inflammation is extremely important for women, especially during the active reproductive period. Due to a chronic pathological process in the area of the pelvic organs, adhesions often occur, forming tubular infertility, resulting from the distance of the tubes and the inability to become pregnant in the future.
Prevention of complications is early initiation of treatment. It is quite difficult to completely protect yourself from inflammatory processes. Ophoritis can occur even against the background of general health, with slight hypothermia and decreased immunity. It is recommended to monitor the quality of personal hygiene and underwear. Air flows and shifting pelvic organs. Stagnant blood flow can contribute to the development of infectious and inflammatory processes. Several times a year, visit a gynecologist and examine the genital organs.
It is very important to avoid casual sex and abortion, which often result in inflammation of the ovaries. Even with minor irregularities in the menstrual cycle, which can help restore the pathological process and prevent complications dangerous to health.
How to detect inflammation of the ovaries and fallopian tubes?
Pain in the lower abdomen on the right, left side (or bilateral) requires a gynecological examination. To diagnose adnexitis, it is necessary to perform a smear from the vagina and cervix with an antibiogram to check which pathogen caused the symptoms and find out which antibiotic should be prescribed.
When diagnosing inflammation of the uterine appendages, blood tests are also prescribed to evaluate the number of leukocytes and C-reactive protein. During inflammation of the appendages, the ovaries (or appendages) become enlarged, so abdominal ultrasound is a useful diagnostic method.
Acute form
In the acute form, the clinic manifests itself clearly and there are many symptoms. In this case, there are practically no difficulties in diagnosis. Acute onset with high fever (up to 400), chills, intense pain of different localization, with copious discharge of various, mainly purulent, nature. The pain is localized depending on the damage to the ovaries. Inflammation of the ovaries in women can be bilateral or on one side. If both ovaries are involved in the process, the pain is disturbing in the groin area, strong, acute, accompanied by general symptoms of intoxication: fever, maybe chills, general malaise, headaches, weakness.
With unilateral damage, pain appears from the side of inflammation and can radiate to the lower back or rectum. This may interfere with the process of defecation. Depending on which side the pathological process develops, it is necessary to differentiate with appendicitis (on the right) or with renal colic. Inflammation of the ovaries can affect the urinary organs, and then the process of urination itself is disrupted. If the uterus is involved in the inflammatory process, the pain is intense in the lower abdomen, without clear localization and irradiation. That is, in terms of symptoms, it resembles an acute surgical pathology and requires urgent hospitalization in a hospital.
Treatment of adnexitis - antibiotics, surgery
The healing process depends on the type of inflammation of the appendages, the patient’s condition and the complications listed above. The basis of treatment for an acute condition is urgent hospitalization and intensive antibacterial therapy. An antibiotic for adnexitis must have a wide spectrum of action. Initially, the drugs are administered intravenously, then administered orally. The gynecologist will also prescribe a diet and apply cold compresses to the abdomen.
Surgery for inflammation of the appendages is used in case of failure of conservative treatment, deterioration of the patient’s condition, or the appearance of symptoms of peritonitis. Antibiotics are also used for chronic and sub-spatial conditions. Only complications of the resulting inflammation of the appendages are operated on. The most dangerous of them is peritonitis, caused, for example, by rupture of an ovarian abscess.
In life-threatening conditions, surgeons use an open surgical method, which consists of a wide incision in the abdominal tissue and cleansing the abdominal cavity of pus. For less serious complications, such as a fallopian tube cyst, laparoscopy may be used.
Treatment of inflammation of the appendages with home remedies is ineffective, and any attempts to use natural methods, including herbs, can only do harm and delay a visit to the gynecologist.
A tumor of the left ovary can be:
- germ cell tumor (embryonic cell tumor);
- epithelial (tumor formation occurs in the ovarian epithelium);
- hormonally active (stromal tumor that produces hormones forms in the tissues that form the basis of the ovary).
The majority of tumors of the left ovary of any group are initially benign. Treatment of a benign tumor can be carried out either medicinally or surgically. In turn, both methods lead to a complete cure, often even with preservation of reproductive function. But even under conditions of a histologically benign tumor structure, the course of the disease can be malignant (rapid tumor growth, metastasis).
A malignant ovarian tumor can be primary or secondary. A primary malignant tumor of the ovary affects the ovary directly, but the most common malignant tumor is still secondary. Secondary malignant ovarian tumors develop in serous and mucinous cystadenomas.
Metastatic malignant tumor of the ovaries (Krukenberg) is also common. Metastasis to the ovaries occurs by lymphogenous, implantation or hematogenous route from the primary site (for example: mammary gland, uterus, intestines).
Treatment of the chronic form
Treatment of the disease in a chronic form is reduced to pain relief, restoration of reproductive function and the formation of beneficial microflora of the woman’s genital organs, which has an anti-inflammatory and antimicrobial effect.
The doctor prescribes anti-inflammatory drugs, immunomodulators, physiotherapy - mud therapy, mineral baths, gynecological massage, acupuncture. Treatment of chronic ovarian inflammation takes a long time and sometimes requires surgical intervention.
Diagnosis
Recognizing oophoritis is a complex process, because Its manifestations are similar to many diseases. To establish the transition of inflammation to the ovaries, the gynecologist:
- Interviews the patient - interested in past illnesses, birth history, presence of abortions, symptoms, duration of course.
- Conducts an examination - palpation, manipulation with a mirror.
- Refers for laboratory testing - analysis of vaginal secretions, blood, urine, urethral smear, bacterial culture.
- Uses instrumental methods - hysterosalpingography, ultrasound OMT, fallopian tubes (USGSS).
- He resorts to additional methods - tuberculin diagnostics, PCR analysis, ELISA, laparoscopy.
Pathogenesis
Typically, oophoritis (usually salpingoophoritis) develops as an ascending infection from the vagina or uterus due to infection during sexual intercourse or complicated abortions and childbirth. In response to the introduction of the pathogen, an inflammatory reaction of the body occurs.
When the ovaries are involved in the process, their epithelium and adjacent peritoneum are first infected ( periophoritis ). Then inflammation covers the cortical layer of the ovary (actually oophoritis). In the ovary, microcirculation is disrupted, tissue damage occurs, and swelling occurs due to inflammatory effusion. Multiple follicular cysts of varying diameters form inside the enlarged ovary, as in polycystic ovary syndrome. Unlike polycystic disease, in this case there is no thickening of the stroma.
Proliferation is the final phase of inflammation and the number of connective tissue cells in the lesion increases and the number of T and B lymphocytes increases. Connective tissue cells can differentiate into fibroblasts, which produce rough fibrous tissue that replaces normal ovarian tissue. As a result of this, it loses its function.
Sometimes ulcers form in the cavity of the follicle or small cysts, which, merging, form an ovarian abscess , which is considered as a complication of oophoritis. Infectious factors are a prerequisite for the development of autoimmune oophoritis with its characteristic decrease in hormonal function.
The chronic inflammatory process is the breeding ground for the human papillomavirus, cancer and precancerous processes, since local immunity decreases.
List of sources
- Abramchenko V.V., Bashmakova M.A., Korkhov V.V. Antibiotics in obstetrics and gynecology. – St. Petersburg: Spetslit, 2000.– 220 p.
- Rational pharmacotherapy in obstetrics and gynecology // Guide for practitioners, edited by V.I. Kulakova, V.N. Serova, M., “Litterra”, 2005, pp. 724–727.
- Serov V.N., Tikhomirov A.L. Modern principles of treatment of inflammatory diseases of the female genital organs. Toolkit. M., 2002.
- Prilepskaya V.N. Features of infectious processes of the lower genital tract. Possibilities of therapy with drugs for local use // Gynecology. 2000; 2 (2): pp. 57–59.
- Abramchenko V.V., Kostyuchek D.F., Perfileva G.N. Purulent-septic infection in obstetric and gynecological practice. St. Petersburg, 1994. 137 p.
Chronic oophoritis and pregnancy
If chronic oophoritis is diagnosed, is it possible to get pregnant in this case?
The likelihood of conception remains until ovarian function is completely lost. However, there is a risk of ectopic pregnancy. In addition, pregnancy against the background of the disease can provoke a tumor process of the uterus and ovarian cystosis.
You should plan pregnancy only after completing the course of treatment.
To make an appointment or get advice, call the 24-hour number
+7
or fill out the form