The trigeminal nerve is a ganglion that gives rise to three “branches” that exit directly from the brain stem. Three “branches” reach directly to the human face, supplying it with nerves and connecting it with the central nervous system.
The trigeminal nerve exits the skull through three different foramina. The first “branch” comes out through symmetrical points that are located slightly above the person’s eyebrows (the so-called ocular process). The second, emerging, passes along both sides of the nose (just below the eye area and close to the cheeks) and is therefore called the maxillary, the third “branch” exits in the lower jaw (mandibular) in the direction from the corners of the mouth to its center.
With inflammation of various processes of the trigeminal nerve, pain is observed, localized in various places of the face. When the first “branch” is inflamed, pain occurs above or below the brow ridge, in the forehead and in the front part of the temporal region of the head. When the second and third “branches” of the trigeminal nerve become inflamed, pain occurs in the upper and lower jaws, respectively, which, in turn, causes severe toothache.
Next, we will talk about the types of neuralgia, causes and methods of treatment. But if you are experiencing unbearable pain right now, make an appointment with us. When making an appointment, tell the administrator that you need emergency assistance, and they will find an appointment for you as soon as possible. An appointment with a dentist can be made by calling 8 or using the online appointment form.
Types of trigeminal neuralgia
Trigeminal neuralgia is divided into two types. The first, the so-called true trigeminal neuralgia, is a holistic disease caused in most cases by compression of the nerve or disruption of the blood supply. The second type - secondary trigeminal neuralgia - is a symptom of a general disease of the body. It could be a tumor or a serious infection.
In most cases, doctors diagnose inflammation of one of the processes of the trigeminal nerve, but in some situations inflammation of two or three processes occurs at once. Inflammation can affect either one side of the face or both, and in different combinations.
Diagnostics
Based only on a survey, a doctor can distinguish tertiary neuralgia from Sjostad syndrome (with this syndrome, longer attacks), post-herpical pain, and typical migraines. To understand the full picture, it is important to carry out a comprehensive diagnosis:
- Tomography. For accurate diagnosis and correct treatment, the most complete data on the state of the brain and the selection of a detailed scheme (the scheme is important for accurate positioning) when performing magnetic resonance imaging of the ternary nerve are extremely important. The most accurate data can be obtained from MRI with contrast.
- Tomography (scanning) scan of the trigeminal nerve. Makes it possible to create layer-by-layer images, identify neurovascular conflict, signs of destruction of the myelin sheath of nerves. The scan allows the doctor to get a complete picture of what the nerve being examined looks like and what is happening where it exits the brain stem.
- It is extremely important that tomography allows not only to identify that there is a neurovascular conflict, but also to understand its cause. This may be a conflict of the cerebellar arteries, a neuroma (neoplasm) of the nerve. In many cases, the trigeminal nerve scan is performed with a simultaneous scan of the facial nerve.
- X-ray of the jaws (if you suspect that the main problem is dental).
- Angiography. Important for verification (confirmation) of the vascular origin of compression with an impressive size of the aneurysm and vascular loop or aneurysm.
Also, in most cases, blood and urine tests are prescribed (the role of these studies is especially valuable in pathologies that arise as a result of infectious diseases).
Causes of inflammation of the trigeminal nerve
Doctors believe that the main cause of inflammation of the trigeminal nerve is compression of it either inside the skull or outside it. Inside the skull, the trigeminal nerve can be compressed as a result of the formation of tumors, in most cases resulting from some kind of head injury.
Also a fairly common cause of inflammation of the trigeminal nerve is internal venous or arterial displacement.
Other causes of trigeminal neuralgia include:
- the presence of a chronic inflammatory process, viral or bacterial infection in the body;
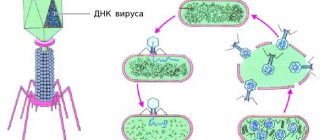
- herpes infection (herpes);
- a brain tumor;
- scarring in the brain stem;
- failure of anesthesia during treatment or tooth extraction.
Most often, inflammation of the trigeminal nerve affects women at pre-retirement and retirement age (usually from fifty to seventy years). If trigeminal neuralgia is diagnosed in a young man or girl, then most likely its cause is a change in the arteries of a sclerotic nature or a strong dilatation of blood vessels.
Consequences and complications
It is important to start treating neuralgia in a timely manner. Untimely treatment is fraught with the following complications:
- Continuous pain (both headaches and facial pain).
- Paralysis of the facial nerve and, as a result, facial asymmetry.
- Weakening of hearing and vision.
- Weakening of facial muscles, appearance of wrinkles.
- Behavioral disorder. Constant fears. The person constantly thinks that he may have another attack. Therefore, he tries to move minimally when chewing (or chews, moving food behind one cheek), and smile a little.
How does inflammation of the trigeminal nerve manifest?
The main symptom of inflammation of the trigeminal nerve is severe pain that occurs in the facial part. The pain really has a powerful force and shooting character, so it is very difficult for the patient to calmly endure painful attacks. The pain intensifies when performing the slightest actions with the facial muscles and jaws - yawning, chewing, laughing, and performing daily oral hygiene. At the same time, the sensitivity of the skin on the inflamed side of the face decreases.
The next painful attack is accompanied by a rapid dilation of the patient’s pupils and the same rapid contraction of facial muscles. Increased tear production may begin.
Pain with trigeminal neuralgia is severe, but not constant. The pain occurs for a few seconds and is interrupted for a while. But if the intervals between painful attacks are short, then it seems that the pain is constant. Trigeminal neuralgia is dangerous because the interval between attacks can be several weeks, and sometimes even several months. But after this period, the pain will certainly return. A long break does not mean that the disease has passed, so if you have already noticed symptoms of neuralgia once, you should immediately consult a doctor.
Procedures
An alternative for patients who are contraindicated for complex operations, but drug and physiotherapeutic treatment does not provide an effect, may be the following procedures during an exacerbation:
- Injection of glycerin with a hollow needle through the cheek . The procedure allows you to influence the fibers responsible for pain, but careful monitoring of the procedure is problematic. Only 80% of patients experience real relief.
- Balloon compression . It is carried out through the skin using a catheter. A big plus of the procedure is the ability to provide immediate pain relief. Disadvantage: Requires general anesthesia.
- Stereotactic rhizotomy under the influence of electrical impulses . The pain relief effect is high, but in addition to eliminating the symptoms of neuralgia, unfortunately, nerve cells also die. Like balloon compression, the procedure requires general anesthesia.
- Development of hypochondria, depression.
Why do teeth hurt when the trigeminal nerve is inflamed?
How is inflammation of the trigeminal nerve related to teeth? The connection here is the most direct. Firstly, severe pain during attacks “radiates” to the upper or lower jaw (depending on which nerve extension is inflamed), and sometimes to both jaws. This causes severe and unbearable toothache.
Secondly, those nerves that are found in the upper and lower teeth and gums are directly connected to the trigeminal nerve. The second branch of the trigeminal nerve innervates the upper teeth and gums, and the third, respectively, the lower jaw and gums.
The trigeminal nerve can also be damaged during a number of dental manipulations. Unsuccessful tooth extraction or improper filling, surgical intervention in the jaw structure that ended unsuccessfully, and injuries can cause trigeminal neuralgia.
It is very important to distinguish inflammation of the trigeminal nerve from other diseases of the oral cavity, in particular pulpitis - inflammation of the internal dental tissues. A characteristic sign of inflammation of the trigeminal nerve is that, despite severe pain, the sensitivity of the teeth does not increase when they come into contact with cold and hot foods, and hypothermia or heating does not provoke the onset of a new pain attack. Acute tooth sensitivity is a symptom of pulpitis.
When the trigeminal nerve is damaged in the jaw area, acute toothache, pain in the chin, ears and sometimes in the lower lip occurs. The pain may become increasingly intense, and often the patient continues to feel a dull ache after the attack.
General information
Pain in the facial area is considered the most difficult in medicine, as it is associated with pathologies of the nervous system, ENT organs, dental system or eyes. However, trigeminal neuralgia is often the cause of such pain.
The problem is at the top of the ranking of neurological diseases due to a large number of factors: excruciating paroxysmal pain, social and work maladjustment (it is extremely difficult for a person to work productively, he is under constant stress), long-term treatment. Symptoms can be identified, but only a specialist can prescribe the exact cause of the disease and truly effective treatment. In the 5th city hospital of Minsk, all conditions have been created for high-quality neurological and neurosurgical care: from diagnosis to treatment.
Treatment of inflammation of the trigeminal nerve
The first stage of treatment for inflammation of the trigeminal nerve is medication. It is aimed at reducing the strength and frequency of pain in the patient. Most often, doctors prescribe anticonvulsants to a patient suffering from trigeminal neuralgia. Sedatives are also used.
Physiotherapeutic procedures, as well as resorption therapy to relieve the inflammatory process, have a good therapeutic effect. Next, the doctor may recommend the use of laser treatment, in which the laser is directed cutaneously to the area where the processes of the trigeminal nerve exit the skull.
Our clinic is located in the same building as the multidisciplinary clinic “Diamed on Shchelkovskaya”, where special conditions for receiving physiotherapeutic procedures are organized for dental patients. The clinic’s physiotherapy room is equipped with modern equipment, including a laser physiotherapy device, with which you will feel relief after the first procedure. The pain will go away and you can return to normal eating. Make an appointment with a dentist by calling 8 or using the online appointment form. The doctor will make an accurate diagnosis and refer you for treatment.
If you are in severe pain, but for some reason you have not yet made an appointment with us, then it can be relieved with folk remedies. Take one tablespoon of yarrow, pour a glass of boiling water, let it brew for one hour and strain. The tincture should be taken one tablespoon before meals three to four times a day.
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Trigeminal nerve, symptoms of trigeminal nerve damage, pathology
Damage to one of the sensory branches of the trigeminal nerve results in a disturbance of all types of sensitivity on the face of a peripheral type in the zone of innervation of this branch. In this case, symptoms : pain, decreased reflexes, extinction of reflexes. When the optic nerve is damaged, the conjunctival reflex, corneal reflex, and superciliary reflex are affected. When the motor part of the mandibular nerve is damaged, the mandibular reflex suffers. When the trigeminal nerve ganglion is damaged, all types of sensitivity in the area of 3 of its branches are lost, herpetic eruptions (herpes, herpetic blisters), and trophic disorders are often observed. A lesion of one of the sensitive nuclei in the pons results in a dissociated type of sensitivity disorder - superficial or deep. When the nucleus and oral parts of the spinal tract are damaged, a violation of superficial types of sensitivity in the mouth and nose occurs. If the caudal region is affected, sensitivity is impaired in the area of the outer part of the face. When the optic thalamus and the posterior third of the posterior limb of the internal capsule are affected, contralateral hypersthesia is observed on the face, trunk (body), and limbs (arms, legs) according to the hemitype. When the motor nucleus and its fibers are damaged, peripheral paresis occurs, which is characterized by symptoms such as insufficient muscle tension when chewing, muscle atrophy, retraction in the temple area, angle of the lower jaw, deviation of the lower jaw towards the affected side when opening the mouth. If bilateral peripheral paresis occurs, the lower jaw droops, as a result of which a man or woman cannot chew, cannot close his teeth, or close his mouth. Central paresis of the masticatory muscles on one side does not occur, since the corticonuclear fibers approach the motor nucleus of the trigeminal nerve from both hemispheres of the brain. With bilateral lesions, chewing becomes slightly more difficult (difficulty chewing), and the mandibular reflex is significantly enhanced. Small children have difficulty sucking.
Trigeminal nerve, anatomy, innervation, where the trigeminal nerve is located
The trigeminal nerve, nervus trigeminus, the 5th pair of human cranial nerves is a mixed nerve that contains sensory, motor and autonomic fibers. The functions of the trigeminal nerve are varied.
The sensory fibers of the trigeminal nerve originate from the cells of the trigeminal ganglion, which is called the ganglium trigeminale. It is located in the recess of the pyramid of the temporal bone. The dendrites of these cells form 3 branches and 3 trunks.
1 branch of the trigeminal nerve, the first branch (nervus ophthalmicus) - the ophthalmic nerve passes in the lateral wall of the cavernous sinus, later through the superior orbital fissure into the orbit. Then it breaks up into branches, innervates such structures as the outer part of the conjunctiva, the skin of the outer corner of the eye, the upper eyelid, the lacrimal gland, the skin of the scalp to the temporal and parietal regions, the skin of the forehead, the skin of the root of the nose, the cornea, the frontal sinus, the main sinuses , nasal mucosa, nasal skin, posterior cells of the ethmoid bone.
2nd branch of the trigeminal nerve, second branch (nervus maxillaris) - the maxillary nerve passes (exit) through the round foramen and the pterygopalatine fossa. It further breaks down into branches and innervates the following sections: the skin of the temporal region (temporal region, temple), the skin of the zygomatic region (cheekbone), the mucous membrane of the posterior ethmoid cells and the main sinus, the vault of the pharynx (pharynx), the nasal cavity (nose), the soft palate, hard palate, mucous membrane of the tonsils (tonsils), skin of the infraorbital region (infraorbital region), wings of the nose, upper lip, gums of the upper jaw, upper teeth.
3rd branch of the trigeminal nerve, third branch (nervus mandibularis) - the mandibular nerve leaves the skull through the foramen ovale (exit point, exit point), innervates the following areas: mucous membrane of the cheek, mucous membrane of the lower gum (lower gum), skin of the corner of the mouth (angle mouth), skin of the external auditory canal, anterior part of the auricle, temple, all lower teeth, skin and mucous membrane of the lower lip.
The motor fibers of the trigeminal nerve originate from the motor nucleus nucleus motorius nervi trigemini. The core is located in the bridge tire. Fibers extending from the nucleus leave the cranial cavity through the foramen ovale. They innervate the masticatory muscles and the anterior belly of the digastric muscle. The axons of the trigeminal ganglion cells form a root and go to the bridge, where they divide into 2 branches.
The descending branch forms the descending spinal tract of the trigeminal nerve, which is responsible for conducting temperature and pain sensitivity. It ends in the nucleus spinalis nervi trigemini. The descending spinal tract and its nuclei are analogous in their function and structure to the posterior horns of the spinal cord. The nuclei and path are divided into 5 segments, as a result of which the innervation of the facial skin in the Zelder zones is located in a ring.
Treatment methods
Depending on what caused the inflammation, a course of treatment is prescribed. For bacterial lesions, the emphasis is on antibacterial therapy through systemic administration of drugs.
However, regardless of the reasons, the doctor prescribes painkillers to relieve pain and reduce inflammation. It could be:
- ibuprofen;
- paracetamol;
- analgin;
- ketorol;
- diclofenac.
All of the listed drugs can be prescribed either in the form of tablets for oral administration, or prescribed in the form of solutions for intramuscular administration.
When conservative methods are not possible, the help of a surgeon may be needed. This primarily concerns abscesses due to the eruption of wisdom teeth, pulpitis or other dental diseases. In this case, the abscess will be opened, pus will be removed, the wound will be treated with antiseptic, and the tooth will be removed, if necessary. If a pinched nerve occurs as a result of pathologies in the structure of the skull, the surgeon will perform an operation to correct the situation and free the nerve bundles.
As a complex therapy, massage, heating or exposure to a magnetic field and electric current can be prescribed. You cannot massage or warm the inflamed area yourself, because this can lead to complications associated with rupture of the purulent capsule, blood poisoning and paralysis of the facial nerve.
Separately, you may need to consult a neurologist who will determine the cause of the inflammation if other specialists have not found obvious foci of infection and abscesses.
Traditional methods of treatment are permissible only as an addition to the main therapy. For example, rinsing with chamomile decoction will relieve inflammation and reduce swelling. But you can resort to such procedures only with the permission of the attending physician.