Causes of the disease
Most often, optic neuritis develops with multiple sclerosis and is its first manifestation. The basis of the inflammatory process in this case is demyelination, or destruction of the myelin sheath of the nerve. Damage to the optic nerve is also provoked by other autoimmune pathologies: systemic lupus erythematosus, Sjogren's syndrome.
Diseases associated with serum immunoglobulin G to myelin-oligodendrocyte glycoprotein (MOG-IgG), in particular acute disseminated encephalomyelitis, also lead to demyelination and, as a consequence, optic neuritis.
Axons and neurons of the optic nerve are destroyed not only as a result of demyelinating processes, but also against the background of other diseases. These include:
- inflammation of the eyeball and/or orbit;
- inflammatory diseases of the brain;
- infectious processes in the nasopharynx;
- sarcoidosis, granulomatosis;
- acute cerebrovascular accident;
- endocrine pathologies – thyrotoxicosis, diabetes mellitus;
- specific infections - tuberculosis, syphilis, influenza.
Optic neuritis can be a consequence of eye injury, traumatic brain injury, toxic damage - in most cases it is poisoning with methyl alcohol, lead, and sometimes helminthic infestations. May be provoked by complicated pregnancy.
Indications
Treatment indications include:
- the presence of one or more symptomatic manifestations;
- head injuries or mechanical damage to the eye;
- regularly occurring headaches;
- dizziness, partial loss of vision;
- blurred vision;
- emerging eye fatigue.
If you have indications, you should contact a specialized center that will provide assistance. Don’t waste time, call our clinic and make an appointment with an ophthalmologist.
Symptoms of optic neuritis
Symptoms vary depending on the type of disease: intrabulbar (papillitis) or retrobulbar neuritis.
Papillitis (intraocular, retrobulbar neuritis)
It is characterized by an acute onset with a rapid deterioration in visual acuity - from 1-2 hours to 1-2 days. In some cases, mild headache and pain when moving the eyes occur. With partial damage, visual acuity may be preserved, but scotomas appear - areas of partial or complete loss of the visual field, which can be central or paracentral, round or arch-like. There may be a narrowing of the boundaries of the visual field, a decrease in dark adaptation and color perception. Most often, symptoms of visual impairment disappear after 7-10 days; after 2-3 weeks (sometimes up to 5 weeks), vision is restored. Without treatment or with severe neuritis, optic nerve atrophy with complete loss of vision is possible.
Retrobulbar neuritis
It occurs in acute or chronic form. The acute form is more often characteristic of unilateral lesions, the chronic form - for bilateral ones.
General symptoms:
- pain when moving the eyeballs and pressing on the eye;
- color vision disorders - decreased sensitivity of the eye to colors, shades quickly fade;
- a drop in visual acuity to the point of complete inability to distinguish objects;
- appearance of scotomas.
Depending on the form of retrobulbar neuritis, symptoms may vary. Axial neuritis is characterized by a combination of central scotoma with partial loss of visual fields and the appearance of peripheral defects in the visual field. In the peripheral form, the field of vision narrows along the entire perimeter - it is concentric in nature. The transversal form is characterized by a significant decrease in vision, up to blindness, scotomas merging with peripheral loss of visual fields.
Read also
Red eye
*Red eye syndrome* is a group of diseases that are accompanied by redness or hyperemia of the eye.
Redness of the eyes (hyperemia) occurs due to dilation of the vessels of the conjunctiva of the sclera and can… Read more
Contact lenses/contact correction
Vision is one of the senses through which we learn about the world around us. Good vision is essential for a high quality of life. The most important characteristic in diagnosis is the acuity...
More details
Myopia
Vision plays a huge role for a person. Through the eye we experience the entire amazing and diverse world. A person receives 80-90% of information from the surrounding world through vision. Therefore, a huge tragedy...
More details
Blindness
Vision is a unique gift that nature has given us. We can truly appreciate it only when we lose. With a number of diseases, vision loss may decrease, sometimes almost to the point of complete blindness. Often…
More details
Facial hemispasm
Facial hemispasm is a forced contraction of the facial muscles of one half of the face. Most often, the orbicularis oculi muscle is first involved in the process, then the muscles of the lower half of the face join.…
More details
Classification and stages of disease development
Depending on the affected area:
- Intrabulbar (intraocular) neuritis, optic papillitis. This is an inflammation of the intraocular part (disc) of the optic nerve. More often develops in children.
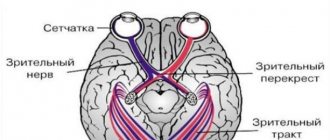
- Retrobulbar neuritis. Damage to the nerve section lying between the eyeball and the optic chiasm. Forms of retrobulbar neuritisSource: Retrobulbar optic neuritis. Kukhtik S.Yu., Popova M.Yu., Tantsurova K.S. Bulletin of the Council of Young Scientists and Specialists of the Chelyabinsk Region, 2021: axial - a bundle of axons passing in the optic nerve is involved in the pathological process;
- peripheral - inflammation covers the nerve sheaths and spreads deep into the nerve trunk with the formation of a large amount of exudate under the sheaths;
- transversal - the process affects all layers of the optic nerve.
According to the etiology of the lesion:
- infectious:
- parainfectious (post-vaccination, after acute respiratory viral infections);
- demyelinating;
- ischemic;
- toxic;
- autoimmune.
According to the severity of the flow:
- spicy;
- chronic.
According to the prevalence of the lesion:
- mononeuritis – inflammation of one nerve (the vast majority of cases);
- polyneuritis – involvement of both optic nerves in the process (less than 1% of cases).
What is cell therapy?
Cell therapy is a promising, modern and actively developing area of medicine. It allows you to get good results for various diseases of the nervous system. The main effects of cell therapy are achieved due to the possibility of replacing dead neurons (nerve cells), improving tissue trophism, forming new nerve endings and blood vessels, and enhancing the body's immune system.
Cell therapy involves treatment with stem cells, a special type of cell that has the ability to specialize into any cell of the human body. Some techniques are still at the stage of clinical trials. Other therapeutic approaches are already successfully used in many clinics around the world, including German clinics.
Benefits of cell therapy:
- Stem cells promote the appearance of new blood vessels
- Increased blood circulation in the vessels of the optic nerve and retina
- There is an improvement in the nutrition of nerve fibers
- The ability to restore tissue structures of the visual analyzer
- Stem cells release biologically active compounds, thereby preventing the formation of scars
- Increasing immunity and at the same time suppressing unwanted activity of the immune system in the pathological focus
- Restoration of normal metabolism in tissues
- Self-cell therapy is well tolerated by patients
Stem cell treatment has virtually no contraindications and can be performed on patients with various forms of atrophy at any age.
Diagnosis of the disease
As a rule, patients who have the first symptoms of optic neuritis turn to an ophthalmologist. The disease is considered an interdisciplinary pathology; an ophthalmologist or neurologist must take part in its treatment. If neuritis develops against the background of other pathologies, it is necessary to clarify the diagnosis and carry out specific therapy for the primary diseases. Source: Visualization of the optic nerve in the diagnosis and monitoring of retrobulbar neuritis. Yuryeva T.N., Burlakova E.V., Khudonogov A.A., Ayueva E.K., Sukharchuk O.V. Acta Biomedica Scientifica, 2011. p. 133-136. Then the appropriate specialists are involved in the treatment - an immunologist, an otolaryngologist, an infectious disease specialist, a phthisiatrician.
The first step in diagnosing optic neuritis is collecting anamnesis, external examination of the patient, and palpation. During the medical history, the doctor will clarify the presence of concomitant pathologies, the time of onset of the disease, what complaints the patient has (pain, decreased visual acuity, changes in color perception, the appearance of “blind” spots), how quickly the symptoms developed and how severe they are, whether one eye or both is affected.
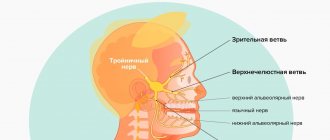
External examination and palpation may often not provide additional data. Pain, forward displacement of the eyeball, and limitation of its movements may occur with retrobulbar neuritis, but are not obligatory.
Next, the doctor proceeds to an ophthalmological examination. It includes:
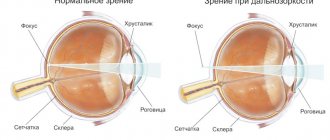
- determination of visual acuity;
- the study of color perception is carried out using Rabkin’s polychromatic tables;
- study of pupil reaction to light;
- measurement of intraocular pressure, which can be a symptom of glaucoma and other diseases that provoke the development of neuritis;
- biomicroscopy – examination of the anterior segment of the eye to exclude its pathology;
- ophthalmoscopy (examination of the fundus of the eye) after instillation of drops that dilate the pupil;
- computer examination of visual fields at 120 points;
- study of visual fields using kinetic perimetry.
To clarify the diagnosis, the following methods are used:
- electrophysiological diagnostics - study of the threshold of electrical sensitivity of the retina and visual evoked potentials;
- ultrasound examination of the eyes, MRI of the orbit of the eye and brain;
- coherence tomography of the optic nerve;
- fluorescein angiography of the retina.
Laboratory diagnostics:
- general blood analysis;
- blood for HIV, syphilis, rheumatoid factor;
- blood culture for sterility;
- PCR studies;
- histological, immunochemical analysis.
If the patient has concomitant diseases, he is prescribed consultations with specialists.
Sources of mesenchymal stem cells
The first source of mesenchymal stem cells is the bone marrow, followed by umbilical cord blood and adipose tissue. Bone marrow is the best source of MSCs, but in some cases its use has contraindications: limited growth rate, dependence of differentiation on the age of the donor, and some inherited risks of tissue sampling. As for umbilical cord blood, obtaining MSCs requires compliance with all points of a special protocol, and this is not always possible. It is also not always possible to find a source of umbilical cord blood. Mesenchymal cells derived from adipose tissue have a similar structure and phenotype to bone marrow cells. These cells proliferate better and are easier to harvest from liposuction procedures.
Treatment of optic neuritis
Treatment must be carried out in a hospital setting; it should begin as early as possible, in order to avoid the disease becoming chronic and developing complications. Source: Modern view on the problem of optic neuritis (systematic review). Krivosheeva M.S., Ioileva E.E. Saratov Scientific and Medical Journal, 2021. p. 602-605. For patients with optic neuritis, diet No. 15 is indicated - a general table, in the absence of indications for other types of therapeutic diets.
The basis of treatment is etiotropic therapy aimed at eliminating the primary disease that caused optic neuritis. Until the etiology of the disease is clarified, remedies are used to reduce the symptoms of inflammation, remove swelling, allergic manifestations, and improve metabolism. For this purpose:
- glucocorticosteroid drugs, if they are intolerant - non-steroidal anti-inflammatory drugs (prescribed in rare cases);
- antibacterial or antiviral therapy;
- antifungal agents to prevent fungal infection due to a long course of antibiotics;
- detoxification therapy – intravenous drip administration of saline solutions;
- antihistamines;
- diuretics;
- products that improve microcirculation;
- neuroprotectors;
- vitamins.
In addition to medications, physical therapy may be used to treat optic neuritis.
With papillitis, as well as the infectious-toxic etiology of the disease, the prognosis is more favorable than with other types of optic neuritis - in 75-90% of cases, with proper treatment, vision is completely restored. When the optic nerve is damaged due to autoimmune, demyelinating diseases, collagenosis, sarcoidosis, and specific infections, relapses often occur, incomplete restoration of vision, and nerve atrophy is possible. Source: Results of treatment of optic neuritis. Latypova E.A. Saratov Scientific and Medical Journal, 2021. p. 875-879.
How does stem cell therapy work in Germany?
The stem cell product contains millions of viable neuronal precursor cells that make up the optic nerve and its nerve endings. Carrying out cell therapy includes several stages:
- Specialists collect stem cells from the bone marrow by puncturing the ilium, or they are isolated from adipose tissue through an operation similar to liposuction.
- The main parameters of stem cells – quantity and viability – are assessed, as well as a check for the presence of blood infections.
- If the cellular material meets all the standards for reimplantation, it is purified. The viability of stem cells should be 98-99%.
- The required amount of the drug is injected into the sub-Tenon and suprachoroidal spaces of the eye (in certain areas of the orbit near the optic nerve). This operation is low-traumatic and takes little time.
- After 1-2 months, it is possible to repeat the session in order to consolidate the treatment results.
This method of administration ensures penetration directly into the pathology site, which guarantees the most positive effect from the procedure. The treatment is easily tolerated by patients and has no side effects. For a better result, an additional course of reflexology and electrical stimulation is prescribed, and, if necessary, drug therapy.
View program with price
Disease prevention
To prevent optic neuritis, it is recommended to give up bad habits, promptly treat infectious diseases, avoid eye and head injuries, and visit specialized doctors in the presence of chronic pathologies.
Article sources:
- Retrobulbar optic neuritis. Kukhtik S.Yu., Popova M.Yu., Tantsurova K.S. Bulletin of the Council of Young Scientists and Specialists of the Chelyabinsk Region, 2016
- Visualization of the optic nerve in the diagnosis and monitoring of retrobulbar neuritis. Yuryeva T.N., Burlakova E.V., Khudonogov A.A., Ayueva E.K., Sukharchuk O.V. Acta Biomedica Scientifica, 2011. p. 133-136
- Modern view on the problem of optic neuritis (systematic review). Krivosheeva M.S., Ioileva E.E. Saratov Scientific and Medical Journal, 2021. p. 602-605
- Results of treatment of optic neuritis. Latypova E.A. Saratov Scientific and Medical Journal, 2021. p. 875-879