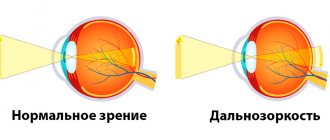
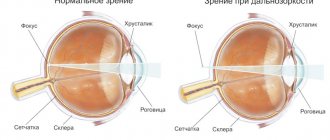
Myopia, better known as myopia or simply myopia, is one of the most ancient, widespread and global problems of ophthalmology. Along with farsightedness and astigmatism, myopia is a refractive error, i.e. refraction of light by the lens. With myopia, refraction is excessive, as a result of which the focal point of the optical system of the eye is not on the sensitive surface of the retina, as is normal, but in front of it.
The average distance from the cornea of the eye (the outer protective transparent layer) to the optical zone of the retina is approximately 23.5 mm. With myopia, this distance is increased by 1-7 mm, and in some cases even more, and each extra millimeter turns into three diopters of the well-known “minus”, i.e. myopia.
By the way, the designation of myopia with a “minus” sign, and farsightedness with a “plus” sign came to ophthalmology from optics: it is the minus that marks the corrective concave lenses necessary for myopia.
Causes of myopia
First of all, it is necessary to distinguish two large and significantly different categories of myopia: congenital and acquired. As follows from the terminology, in the first case, myopia is caused by abnormal development of the eye in the prenatal stage, in the second, it is caused by unfavorable conditions and/or influences after birth.
The main prerequisites for the development of acquired myopia include:
- genetic predisposition (the likelihood is especially high if both parents are myopic);
- physical inactivity (physical passivity, inactivity);
- chronic overload of the visual system (for example, any profession that requires constant intense looking at small details or increased concentration of visual attention);
- neglect of the principles of safe writing and reading (distance, lighting, duration);
- the presence of another ophthalmological problem, for example, strabismus or astigmatism (in this case, myopia may develop as a secondary consequence of the underlying pathology).
According to large-scale statistical studies, the most significant risk factor is heredity with myopia. However, one should not ignore the other prerequisites, attributing everything to “bad genes” and abdicating responsibility for one’s own health: any of the listed factors, and especially an unfavorable combination of them, can lead to the development of myopia at any age.
Myopia symptoms
The main manifestations of myopia are:
- inability to clearly distinguish distant objects;
- the optical effect of “blurring” their boundaries;
- poorly differentiated perception of distant images as a chaotic overlay of muddy colored spots, without distinguishing significant details;
- more or less intact “near vision”.
Sometimes the focal point is shifted so much that a nearsighted person has to bring the object in question (or bring his eyes closer to it) to a distance of literally a few centimeters, removing corrective glasses with dramatically thick lenses.
When myopia and astigmatism are combined, additional symptoms are possible: double vision of the object being contemplated, various distortions of the shape of objects (due to the fact that objectively straight contours can be projected onto the retina as curvilinear).
Degrees of myopia
In ophthalmology, various typological classifications of myopia are used, based on certain criteria. One of the simplest and most obvious is the classification based on the severity of the refractive error:
- mild degree of myopia (no more than -3.0 diopters);
- medium degree (from -3.25 to 6.0 diopters);
- high degree (over -6.25 diopters).
Returning to the above optical-geometric dependencies, it is easy to notice that myopia of the first, weak degree of severity is due to an increase in the anatomically normal distance from the cornea to the retina by only one millimeter.
Moderate and high myopia, caused by a significant anomaly in the structure of the eye, is fraught not only with visual impairment. As a rule, it is accompanied by serious pathology of the retina, circulatory system, lens (degenerative changes, thinning, stretching of the membranes, etc.).
Visual acuity can be extremely insufficient and amount to only 1-2% of the average standard. With such vision, a person, at best, can distinguish fingers on an outstretched arm, and is able to read only at a distance of 5-10 cm from the text. In addition, the purely cosmetic effect of myopia has a negative psychological impact: with myopia of, for example, -20 diopters, in order to ensure at least a minimal quality of life, it is necessary to wear corrective glasses with very thick glasses, which optically reduce the patient’s eyes from the point of view of an outside observer.
Contact lenses for low myopia
Contact lenses are rarely prescribed for vision correction in early myopia. Typically, permanent correction is not required at this stage. Glasses are much more convenient to take off and put on if necessary, which is why most doctors prescribe them. For mild myopia, contact lenses with negative diopters are prescribed. “Minus” optical products help reduce the power of the refractive apparatus and concentrate the focus in the center of the retina. It is very important that the diopters of the lenses fully correspond to the refraction of the eye. You should not purchase ophthalmic products yourself. Before purchasing them, you should consult an ophthalmologist. In the recipe he will indicate the necessary parameters. If this is not done, then the lenses can freely “sit” on the cornea and move during the day. People who have a mild degree of myopia do not always quickly get used to the presence of a foreign body in the eye. That’s why ophthalmologists often prescribe biocompatible models for them.
False myopia
True myopia is caused by abnormal optical-geometric proportions in the structure of the eye, false myopia is caused by a spasm of accommodation, i.e. the inability of the ciliary muscle to relax and bring the lens to the optically required shape (for proper refractive support for distance vision, the lens must take on a flatter appearance). Such chronic overstrain of the ciliary muscle, which usually occurs during long hours of daily work with close objects and small parts (the muscle is toned, the lens takes on a more convex shape), is usually cured with medications in combination with mandatory gymnastics for the eye muscles. Spasm of accommodation can be corrected with glasses or contact lenses (similar to true myopia), but this approach is completely wrong.
Differences between myopia and farsightedness
Given the above, it is easy to imagine the anatomical differences between two well-known refractive errors: nearsightedness (myopia) and farsightedness (hyperopia). In the first case, the focal point of the clearest image is in front of the retina, in the second - behind it, which causes blurred near vision (farsightedness).
In other words, in a farsighted eye, the distance between the cornea and the retina is not greater (as in myopia), but less than necessary. However, there is a second, not so common cause of hypermetropia: too weak, insufficient refractive characteristics of the cornea itself.
Features of diagnosing myopia in preschool children
Congenital myopia in preschool children is extremely rare; in most cases it is acquired. In early childhood, it is difficult to suspect the disease, since the child is not able to understand that his vision is deteriorating and does not complain about its decline, and parents do not attach importance to the child’s changing behavior due to visual impairment. It is important to undergo regular examinations at an ophthalmological center; this is the only way to identify the disease and timely treat myopia in children with a weak degree, and not wait for progressive development.
Diagnosis of myopia
Despite the apparent obviousness, evidence of myopia and establishment of a clinical diagnosis requires a thorough examination, including to distinguish between true and false myopia, simple and complicated by astigmatism, etc.
The following diagnostic methods are usually used:
- visometry (accurate measurement of existing visual acuity by replacing interchangeable lenses of varying strengths);
- perimetry (assessment of visual fields);
- skiascopy (determining the nature and strength of refraction by the displacement of the shadow from the ophthalmoscopic mirror);
- refractometry (requires pupil dilation, used to determine the true parameters of light refraction in the eye);
- tonometry (measuring the pressure of intraocular media to exclude glaucoma);
- visual examination of the fundus using a Goldmann lens (numerous deviations and pathological changes are possible, for example, myopic cone, protrusion of the sclera, hemorrhages, retinal dystrophy, etc.);
- Ultrasound examination of the eye with precise measurement of its basic geometric parameters.
Varieties
It is important not only the degree of the disease, but also the determination of its type. Based on the nature of its occurrence, myopia is divided into:
- to a landline. The identified pathology does not worsen over time;
- progressive. Vision is steadily declining. Every year it decreases by about one diopter;
- malignant. It is not so much a refractive error as a severe type of disease that quickly leads to disability. A person loses the ability to perform usual professional and everyday activities.
Diagnostics
Mild myopia may initially not manifest itself in any way and may not affect the quality of life. To determine the pathology and take timely corrective measures, you need to visit an ophthalmologist annually. The level of acute vision is checked using Sivtsev or Golovin tables. For young children, a specially designed Orlova table is sometimes used. Surveys are carried out using:
ophthalmoscopy. Allows you to evaluate the retina, optic nerve head, and fundus vessels. With the advent of retinophot, you can not only examine, but also get a high-quality image;- skiascopy. “Shadow test” occurs by illuminating the pupil with a beam of light reflected from the mirror. The position of the spatial optical phenomenon depends on the refraction of the eye being examined;
- refractometry. A non-invasive objective diagnostic method that allows you to determine abnormal changes in the refractive power of the eye, leading to various diseases;
- ophthalmometry. Determines the radius of curvature of the cornea, which is involved in ensuring visual acuity along with other elements of the optical system of the eye. It is carried out by three methods: manual, mechanical and using a computer;
- keratotopography. Allows you to study in detail the condition of the cornea of the eye. The result of the scan is a color map of its surface;
- Ultrasound of the eye, or ophthalmoechography. Allows a detailed study of the structures of the ocular apparatus. The technique is considered highly informative because it provides a detailed image of the orbit on a computer monitor.
Conservative (drug) treatment of myopia
For any patient suffering from myopia, a therapeutic and prophylactic drug course is mandatory, usually prescribed at intervals of 6-12 months. Such tactics are aimed primarily at preventing (or slowing down) further worsening of myopia and generally include:
- vitamin C and B vitamins;
- mydriatic drugs that eliminate accommodation spasms (for example, irifrin or mezaton);
- calcium compounds (eg, intravenous injections of calcium chloride);
- drugs to normalize the condition and functioning of eye tissues (for example, cortexin, renylalamine, intramuscular injections of aloe extract);
- cerebral circulation optimizers (piracetam, pentoxifylline, etc.).
A significant role in the overall therapeutic scheme is given to various methods of reflexology and physiotherapy (magnetic, laser, electrotherapy, massage of the collar area, etc.).
Spectacle and contact correction of myopia
The advisability of wearing corrective glasses or contact lenses is determined not only by the patient’s preferences (for example, aesthetic), but also by numerous clinical nuances, indications and contraindications. Only a qualified ophthalmologist can assess the situation in full, taking into account the anamnesis, the nature of the pathology and the prognosis in a particular case, and it is extremely unwise to ignore his recommendations.
The choice between classic glasses and contact lenses is also purely individual. Some patients perceive contact lenses as a solution to all problems and a long-awaited deliverance from “hated glasses” - and wear them constantly without any noticeable difficulties. For others, on the contrary, glasses are a familiar, integral and very important element of the image, and contact lenses cause allergic reactions, various irritations (irritations), and inflammatory processes (keratitis). Both correction methods, glasses and lenses, have their advantages and disadvantages.
It is important to emphasize that in both cases, as a rule, an underestimated, incomplete correction is prescribed - in order to prevent the ciliary muscle from becoming completely lazy and to force it to perform, as far as possible, the functions assigned to it.
An innovative invention in recent years are the so-called orthokeratological lenses, or night wear lenses. As the name suggests, such lenses, made from complex composite synthetic materials, are worn by the patient only while sleeping and are seemingly ordinary corrective contact lenses. The difference, however, is in the unique properties of the lens material: they can be removed in the morning, and the cornea will retain its optically correct shape for up to 24 hours. Orthokeratological lenses do not cause any allergies or corneal hypoxia; they can be prescribed to patients over the age of 6 years with 1-2 degrees of myopia. The approach based on correcting the geometric shape of the cornea is similar to orthokeratological vision correction with laser vision correction, however, lenses, as stated above, are only a palliative, temporary solution to the problem.
Methods, including hardware, aimed at training the ciliary muscle and stimulating neurons of the visual pathways are very important. Such methods, in particular, are absolutely necessary to prevent the development of amblyopia (“lazy vision syndrome,” the gradual exclusion of the poorly seeing eye from visual processes). For this purpose, various accommodation simulators, color pulse devices, and ophthalmic lasers are used.
Disease “Myopia of both eyes”
Some people with myopia experience worsening twilight vision. In this case, myopia occurs in both eyes. A person has to constantly strain his eyes, which leads to muscular asthenopia - visual fatigue.
In this case, these symptoms are supplemented by the occurrence of pain in the eyes, the appearance of “ache” in the eye sockets, and severe headaches. Progressive myopia requires frequent replacement of glasses and contact lenses, since the previous ones no longer correspond to the degree of the disease and no longer correct vision.
Surgical treatment of myopia
Ophthalmic surgery is advisable in cases of rapidly and steadily progressing myopia, resistant to other treatment methods. The so-called scleroplasty is produced when the protective protein shell grows at a rate of more than 1 mm/year. For severe myopia, removal of the lens with implantation of an artificial intraocular lens is prescribed, which performs the same functions, but with the correct refractive parameters. There are other methods of surgical correction, but in recent years, correction using an excimer laser has become a priority method.
Gymnastics for the eyes
The initial stage of myopia can be easily eliminated by performing special therapeutic exercises for the eyes. The exercises should be performed only in a sitting position and preferably in the specified order.
Close your eyes tightly for five seconds, then open them for five seconds. Repeat the exercise 8-10 times.
Blink both eyes for two minutes: try to blink quickly, but without causing discomfort.
Close your eyelids. Use your fingertips to gently massage them, making circular movements.
Close three fingers tightly and press lightly on the upper eyelids with three, release after two seconds and remove your fingers from the eyelids. Repeat 4-5 times.
Use your index fingers to press the skin of your eyebrows, then slowly close your eyes. Hold the skin of the brow ridges firmly: this trains the muscles well. Repeat 10 times.
Laser vision correction
The surgical technology of photorefractive keratectomy (PRK) was the first method of laser correction of myopic vision. A layer of epithelium was removed from the cornea with a scalpel, then the necessary volumes of tissue were evaporated with a laser beam to give the cornea a more correct geometry. The technique involved continued wearing of contact lenses and was associated with a certain risk of complications - in particular, postoperative corneal astigmatism.
The laser epithelial keratomileusis technique (more often called by the English abbreviation LASEK) differs in that the epithelium is not completely removed; After ultra-precise laser action and giving the cornea an anatomically correct shape, the epithelial layer returns to its place. This technique results in faster healing and reduces pain or discomfort.
The modern methodological modification of LASIK (laser in situ keratomileusis) is that the epithelial layer remains in place - it is only incised with a microkeratome and folded back into a flap. After laser ablation (evaporation), the flap takes exactly the same position. No stitches are required, the incision is quickly sealed naturally, and pain is minimized. Wearing contact lenses is also not necessary. However, there are some contraindications to the use of LASIK, for example, an unacceptably thin cornea.
Finally, today’s newest and record-breaking fast method of laser vision correction is Femto- or IntraLASIK. The ablation effect is carried out within a vanishingly short time: the prefix “femto-” means 10-15 seconds. This technique is certainly the least traumatic and the least risky in terms of possible complications or side effects.
It should be noted here that the rate of complications is quite low with any method of laser vision correction.
The most well-known and studied side effects include:
- psychovisual discomfort caused by the “unusuality” of normal vision;
- excessive or insufficient correction, due, for example, to an error in precision calculations;
- corneal astigmatism;
- dryness of the outer membranes of the eye (observed in approximately 20% of cases);
- inflammatory processes as a consequence of an infection or exacerbation of a chronic infection (keratitis, conjunctivitis).
Complications of myopia
As in any other field of medicine, in the treatment of myopia, the earliest possible start of therapy, thorough and comprehensive diagnosis, and correctly calculated correction are of key importance. As you drag out or endlessly postpone a visit to an ophthalmologist, choose your own corrective glasses, etc. – the prognosis is rapidly deteriorating, the likelihood of rapid and irreversible worsening of myopia and the development of such severe complications as amblyopia, scleral protrusion, dystrophic or hemorrhagic damage to the retina, and in the most severe cases – retinal detachment and, as a result, blindness, increases.
Prevention of myopia
Preventive measures that can dramatically reduce the likelihood of developing myopia are quite simple and really effective, especially in childhood and adolescence. And, like most other simple and effective prevention principles, these measures are often ignored.
Let's list them again:
- when reading, the text should be located at arm's length (the same applies to a computer monitor, which can be placed even further without any discomfort), and the TV should be at a distance of at least three meters;
- it is strictly forbidden to read while lying down or in a moving vehicle;
- lighting should be optimal, combine general and local light sources and not cause eye strain (as, for example, when reading in the beam of a flashlight or at dusk);
- If an ophthalmologist prescribes corrective glasses or lenses, this prescription cannot be neglected, no matter how important the excuses may seem.
In conclusion, it should be emphasized: the development of myopia is much easier to prevent in childhood and adolescence than to cure at the stage of severe severity in adults.
Symptoms: how to recognize myopia?
Myopia can appear at any age. Obviously, it is easier to correct the negative consequences of the disease at first. Therefore, adults need to carefully monitor the child’s behavior and be able to promptly recognize the first symptoms of pathology. Children may not realize they have vision problems because they do not understand what is normal. It is recommended to have a preventive examination with an ophthalmologist at least once a year. If the following symptoms occur, you should consult a doctor immediately:
- When looking at distant objects, the child squints.
- The child is often bothered by headaches, which in most cases occur after work associated with visual strain - reading, doing homework, working on the computer, watching TV or playing a tablet.
- While reading, the child brings the book too close to his face, bends low towards the notebook, and comes closer to the TV to look at the picture.
- The child complains of pain and burning in the eyes, blinks frequently and constantly rubs his eyes.
- Absent-mindedness and constant change of activity. The child constantly switches his attention and cannot do one thing for a long time (most often this symptom manifests itself in schoolchildren over 8 years old).
Even if a student has only one of the above symptoms, this is a reason to seek help from a specialist. Otherwise, the disease may progress and correcting the situation will be much more difficult.