Doctor:
Anufriev Ivan Igorevich
Keratoconus is a disease from the field of ophthalmology, characterized by the development of a progressive degenerative process of a non-inflammatory nature. The pathological process is accompanied by thinning of the cornea of the eye, acquiring a cone-shaped shape.
As a result of deformation and dystrophy of the cornea, vision gradually deteriorates. The development of pathology is caused by various biochemical processes. During diagnosis, patients experience a decrease in the synthesis of collagen, protein, and enzymes, and a disruption in the activity of antioxidants occurs. The consequence of these changes is a decrease in the elasticity of the corneal layer, its stretching and acquisition of a cone-shaped shape.
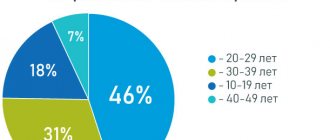
According to statistics, keratoconus develops in only 1 patient out of a thousand, which makes this disease one of the rarest among eye pathologies. It affects men and women equally, but in 9 out of 10 cases the disease is diagnosed in childhood. In this case, the peak progression of keratoconus occurs between the ages of 20 and 30 years.
If untimely or improper treatment is used, the disease progresses and leads to impaired functioning of the affected eye, decreased visual acuity and clarity. However, complete blindness rarely develops, and the patient’s condition can be improved by selecting contact lenses.
To date, keratoconus is a poorly understood disease. But even under this condition, the danger of the disease is low, because doctors have managed to develop a lot of ways to combat this pathology.
Reasons for development
Despite the development of instrumental diagnostic methods, doctors are unable to accurately identify the causes of the disease. But ophthalmologists agree, highlighting the most likely factors predisposing to the development of keratoconus:
- eye injuries received during life, corneal damage; endocrine system disorders;
- polluted environment;
- genetic predisposition (if one of the parents has a history of keratoconus, the risk of developing the disease in the child is 80%);
- various chronic diseases, genetic abnormalities and other diseases (for example, asthma, hay fever, Down syndrome, eczema, inflammation of the conjunctiva and cornea, chronic adrenal insufficiency).
Patient reviews
If you have questions, you can ask our specialists using the feedback form on the website or by multi-channel phone 8(800)777-38-81 daily from 9:00 to 21:00 Moscow time (call for mobile and landline telephone numbers in the Russian Federation toll-free).
In addition to the indicated telephone numbers, you can make an appointment at the clinic using the online registration form.
Possible complications
Deformation of the corneal layer prevents the anatomical function of light refraction. Due to this disorder, the patient's visual acuity is reduced, similar to myopia. Incorrect refraction of light rays when passing through a curved cornea is also reflected in the distortion of visible objects and the refraction of straight lines in the field of view.
The progression of keratoconus complicates the independent choice of glasses and lenses for vision correction. The most severe complication caused by the progression of the pathology is considered to be corneal rupture. This happens when there is a pronounced thinning of the corneal layer, as a result, the functions of the eye are disrupted, and the patient feels acute pain or severe discomfort.
How dangerous is the disease?
The nature of keratoconus is non-inflammatory, but the disease is considered quite dangerous, since in the absence of proper and timely treatment it carries severe complications. In the final stages, thinning of the cornea of the eye is observed, which can lead to its rupture. This process is characterized by acute pain and leads to complete loss of vision without the possibility of recovery.
Classification of keratoconus
In medical practice, there are several classifications of the disease. The most common is the Amsler classification, which includes 4 degrees of development of keratoconus:
- characterized by acquired astigmatism of degree 1-0.5, which is easily corrected by wearing standard contact lenses;
- the degree of astigmatism corresponds to 0.4-1, which can also be successfully corrected;
- thinning of the corneal layer and its stretching are recorded, astigmatism is 0.12-0.02, the selection of special lenses is required;
- the fourth stage is the most severe; as it develops, the cornea takes the shape of a cone and becomes cloudy, vision drops to 0.02-0.01, which is difficult to treat and correct with special lenses.
Treatment of keratoconus requires qualified and timely assistance; self-medication only aggravates the situation. Early contact with a qualified specialist allows you to minimize the rate of progression of the pathology and avoid surgical intervention.
Cost of initial appointment
The cost of treatment for keratoconus at JSC Meditsina (Moscow) is presented in the table below. Please note that prices are listed by category to make it easier to find the service you need. From the table below, you will find out the price of appointments, each test, examination, and other medical procedures for both adults and children. The cost of the initial appointment differs from subsequent ones. If you have any questions, you can call our help desk and find out the prices for treatment.
Keratoconus and pregnancy
In 2011, doctors for the first time conducted a study aimed at studying the course and development of the disease during pregnancy, in which 4 patients took part. Results of the study:
- even due to hormonal changes and a tendency to edema, pregnancy did not affect the accelerated progression of the disease;
- Keratoconus does not affect the course of pregnancy, fetal development or the woman’s condition. The disease is not a contraindication to natural childbirth.
Clinical picture
The common and most common clinical signs of keratoconus include:
- progressive decrease in vision;
- increased fatigue of the visual organs;
- itching and burning sensation on the mucous membranes of the eyeball;
- tearfulness, especially in bright light;
- deformation and clouding of the corneal layer when examined by an ophthalmologist;
- double vision;
- decreased concentration;
- distortion of objects in the field of view;
- the need to frequently change glasses and contact lenses;
- decreased performance associated with impaired vision;
- in rare cases, complete blindness.
Relationship between astigmatism and keratoconus
As can be seen from the above classification of the disease, the early stages of disease progression are accompanied by astigmatism, which is expressed in the corresponding symptoms:
- blurriness and unclearness of the picture that the patient sees;
- discomfort in the eyes, pain, itching and burning, especially in the evening; inability to focus on small objects; headaches, in most cases concentrated in the frontal lobe;
- increased eye fatigue, especially when reading;
- inability to see distant or close objects in detail.
If these clinical signs are initially recognized as astigmatism, the disease subsequently develops and the patient’s condition worsens. The present symptoms allow the ophthalmologist to suspect the presence of keratoconus, especially if the condition rapidly worsens.
How the disease develops
Initially, keratoconus typically affects only one eye. Over time, in the absence of adequate treatment, the pathological process affects both eyes. In this case, the degree of damage to the left and right eyes may differ (one eye sees better than the other), which is associated with alternating damage (initially one, after a while the other).
The early stage of the disease is characterized by a slight decrease in vision, especially blurred vision in the evening, when in poorly lit rooms. As the disease progresses, photophobia may occur, and clouding of the cornea leads to blurred vision and double vision.
Many patients develop monocular polyopia - when looking at two objects, they are perceived as one. Diagnosis of monocular polyopia includes:
- the ophthalmologist places in front of the patient a sheet of black paper with one white spot on it;
- in this case, the patient sees several randomly located spots on a black background;
- voicing the correct answer by the doctor and showing the picture over time does not change the results; in the future, if the disease develops, in the same picture the patient sees even more white spots, randomly located; in the later stages of the progression of the pathology, these spots pulsate in time with the heartbeat.
A special sign of disease progression is that the patient wears perfectly fitted glasses; after 10-15 days they will no longer fit him. In the case of standard lenses, as the disease progresses, wearing them becomes impossible. This is due to deformation of the corneal layer, as a result of which the lens cannot fit completely. Each of these signs indicates with 100% probability the occurrence and worsening of keratoconus.
Other symptoms
Among other clinical signs, the most common are unpleasant and painful sensations in the eyes, increased fatigue, and tearfulness. Such symptoms are manifested by deterioration of vision, as a result of which the patient has to squint and often instinctively rub his eyes.
The same reasons cause the occurrence of headaches, which are associated with a decrease in attention, performance, and ability to concentrate on something. In patients with keratoconus, rapid deterioration of vision is often replaced by long-term stagnation in the development of the disease.
Each of the symptoms described, with the exception of the last, is dangerous for humans. People who need to concentrate on dangerous work or while driving are especially at risk.
Clinic of acute keratoconus
Acute keratoconus is a special type of disease that develops in case of neglect of doctor’s recommendations or errors in treatment. Its occurrence is characterized by clinical signs:
- hyperemia of the mucous membranes of the eye;
- severe swelling of the corneal layer;
- sudden clouding of the cornea or sudden blindness;
- rapid deterioration of visual acuity;
- the occurrence of intense pain.
This condition is dangerous; it is accompanied by rapid deformation and other pathological changes in the corneal layer. Adjustment of treatment and unquestioning adherence to the doctor’s recommendations helps stabilize the patient after 1-2 weeks and improves the functions of the visual organ. If acute keratoconus occurs in the later stages of the pathological process, this is fraught with a violation of the integrity of the corneal layer or blindness.
Symptoms in children
In most cases, the pathological process develops from childhood. You can recognize the disease by looking closely at the child’s behavior:
- school performance deteriorates, the child is distracted and inattentive;
- when reading, the child brings the book closer to his eyes than usual;
- the child begins to squint;
- eyes water and turn red for no apparent reason;
- children systematically complain of headaches;
- in later stages, children report blurriness of the image.
If a child has previously been seen by an ophthalmologist and, according to the doctor’s indications, wears glasses, they quickly become unusable, as evidenced by the corresponding complaints. Changing glasses is accompanied by a short-term improvement and no complaints. But after a couple of weeks, the blurriness of the image and other complaints return again. The lack of timely and correct treatment threatens swelling of the corneal layer and complete blindness.
Diagnostics
Making a diagnosis in the early stages of keratoconus development is extremely important, but at the same time difficult, even with the current development of medicine. This disease is identified by an ophthalmologist based on patient complaints, clinical signs and anamnestic data. However, the final diagnosis is made through additional hardware and physical examinations.
The most reliable and informative diagnostic methods are:
- Skiascopy is a method of initial diagnosis of keratoconus. This test involves the use of a light beam, which is directed by a doctor to the iris, reflected from its surface and forms light stripes on the corneal layer, which should be located at a certain angle. When the cornea is deformed, the angle of curvature of these stripes deviates from the norm, which indicates the development of keratoconus.
- Refractometry is an auxiliary diagnostic method that confirms the fact of deformation of the corneal layer by detecting altered astigmatism and myopia. This diagnostic method is based on the use of a beam of light, which, in keratoconus, changes refractive power and focusing after passing through the cornea.
- Keratometry – makes it possible to make a preliminary diagnosis. The study consists of studying the corneal layer for its curvature. It is carried out using a special device or a computer keratometer. The latter option is more accurate, as it allows you to extremely accurately calculate the curvature of the cornea, comparing current indicators with generally accepted standards.
- Mapped pachymetry - with a high degree of probability allows you to identify pathology in the early stages of development or even at the first alarming signs. During the study, a special device is used to determine the area of deformation at the very beginning of its formation.
- Optical computer topography is a method similar to the previous one, but more accurate, since it involves the use of expert equipment that reads data on the structure of the cornea, analyzes it, highlighting the main signs of deformation of the corneal layer.
- Diaphanoscopy - the study takes into account the characteristics of the shadow on the corneal layer: with keratoconus, it takes a wedge-shaped shape.
- Optical coherence tomography – used during clinical trials.
- Examination of the cornea by biomicroscopy, confocal and endothelial microscopy. These methods are intended for early detection of the disease, as they help determine pathological changes at the cellular level.
One of the methods for detecting keratoconus is the slit lamp, but with its help it is possible to detect the disease only in the later stages of the disease. If, during examination using a slit lamp, the doctor sees a Fleischner ring (a brown-yellow edging formed from iron salts) on the surface layer of the cornea, we can talk about the development of keratoconus. There are 2 other signs that appear on slit lamp examination:
- Vogt's lines - easily eliminated by pressing formations in the superficial layer of the cornea;
- Munsen's sign is a structural change in the edge of the lower eyelid that is visible when the patient looks down.
Of particular importance in making a diagnosis is the differentiation of keratoconus with a number of pathologies:
- myopia;
- astigmatism;
- keratoglobus;
- herpetic lesion of the cornea, etc.
It is important to understand that you should contact an ophthalmologist as early as possible, when the first alarming symptoms appear. This allows treatment to begin earlier, preventing severe progression of the disease and the need for surgical treatment.
Pathogenesis
The cornea is the front part of the eyeball. Normally it has a characteristic convex-concave, spherical shape. Its concave side faces the pupil, the convex side faces outward. The main function is to refract light rays.
The size and shape of the cornea are formed before the age of 4. Until this moment it grows. By the age of four, it is fully formed and then practically does not change.
The cornea can become thinner and “bulge” forward due to pathological structural changes: its shape becomes conical and pointed. In this case, the factor influencing its shape is intraocular pressure. There is no inflammation during this period. This condition is an ophthalmic disease and is known as keratoconus.
Traditional treatment
Helping patients diagnosed with keratoconus involves medical or surgical treatment. Preference for one method or another is given depending on what stage of progression the disease is at, the patient’s condition, the characteristics of the pathology and a number of other factors.
Common treatments for keratoconus include:
- wearing hard contact lenses;
- the use of special glasses and lenses of a special shape, as well as alternate wearing of these attributes to correct vision;
- preventing the progression of the disease with the help of special drugs in combination with ultraviolet irradiation;
- performing collagen crosslinking of the cornea;
- introduction of segmental ring-shaped implants;
- keratoplasty (full or partial).
Each medication is selected only by a doctor individually for each patient; self-medication is strictly contraindicated. At the initial stages of pathology progression, subject to conservative therapy, treatment can be carried out at home. But even in this scenario, the patient must regularly visit the attending physician, who monitors the condition of the visual organs and, if necessary, adjusts the therapy.
Features of treatment in the early stages
The early stages of keratoconus development are symptomatically similar to astigmatism and are treated primarily with conservative methods. The drugs prescribed by the ophthalmologist are aimed at preventing deformation of the corneal layer, relieving unpleasant symptoms and correcting vision clarity.
Each patient diagnosed with keratoconus is recommended to wear special glasses or lenses that completely eliminate vision defects. Lenses and glasses are selected by an ophthalmologist for each patient individually, taking into account the nature of pathological changes. At the same time, each patient is warned that glasses may soon need to be replaced due to deteriorating vision. If there is a sharp deterioration in visual acuity, treatment is adjusted and more intensive methods are used.
Wearing lenses
Taking into account the peculiarities of the pathological process, the ophthalmologist selects special lenses for the patient. They allow you to artificially restore clarity and acuity of vision, and correct the deformation of the corneal layer.
Depending on the nature of the pathology, the following types of lenses are used:
- Soft - rarely used, mainly in the early stages of the disease, until serious deformation of the cornea has occurred.
- Hard ones are the most common option. Lenses help restore the anatomical shape of the corneal layer and correct vision.
- Double-layer - a constructive solution that combines hard and soft elements. They are used to identify areas of thinning of the corneal layer or in cases where wearing a standard hard lens is poorly tolerated by the patient.
- Hybrid contact lenses have soft edges but a hard center. The main advantage is the ability to wear hybrid lenses if you are completely intolerant of hard lenses. However, this option threatens corneal swelling, neovascularization, and the development of conjunctivitis.
- Scleral - have a special structure; when worn, areas of the sclera of the eyeball are additionally covered. This feature allows you to correct the deformation of the corneal layer and ensures reliable fastening of the lens.
Uses of riboflavin
One of the methods of conservative treatment of keratoconus, which involves the use of riboflavin-based drops. After instillation of the drug, the organs of vision are exposed to ultraviolet radiation, the procedure takes up to half an hour.
Performing such procedures makes it possible to strengthen the structure of the corneal layer, significantly reducing the rate of development of the deformation process or stopping it altogether. The use of riboflavin and UV radiation, provided that treatment is started in a timely manner, allows one to avoid complex surgical interventions.
Crosslinking
This treatment method involves treating the corneal layer with a special composition, which becomes hard when exposed to UV rays. Treatment stops the progression of the disease by strengthening the cornea.
The procedure has a number of advantages:
- the result of its implementation lasts for at least 7 years, the progression of the pathology stops; the clarity and acuity of vision increases;
- Cross-linking postpones the need for surgical interventions.
Segmental ring-shaped implants
A minimally invasive operation, partly related to surgical methods for treating keratoconus. The procedure is performed in three stages:
- Using high-precision equipment, the doctor makes a miniature incision on the periphery of the corneal layer;
- arcs made of polymethyl methacrylate are implanted into the “holes” formed after the incision, on both sides of the pupil;
- the incisions made are closed.
Arcs implanted into the corneal layer help gradually level the cornea and give it an anatomically correct shape. The operation is painless and safe and is performed under local anesthesia. If over time there is no positive effect, the arcs are removed from the corneal layer without harm to the organ of vision.
Keratoplasty
Surgical intervention is performed if conservative therapy does not bring the desired results. This operation involves surgical removal of the corneal layer with its subsequent transplantation. The material for transplantation is the donor cornea.
After surgery, complete regeneration of eye tissue requires up to 6 weeks. However, a full restoration of visual acuity and clarity should be expected no earlier than after 9-12 months. Partial keratoplasty can be used to treat pediatric patients, but this operation is much more complex and requires appropriate expert-class equipment.
Crosslinking
Currently, they are trying to treat the disease using corneal collagen cross-linking. This is a new method to stop the progression of keratoconus. This treatment is used to increase the rigidity of the cornea, which allows it to resist further deformation. The principles of treatment in this case are to strengthen the bonds between collagen microfibrils in the cornea, as well as between and within the molecules that form these microfibrils. This can be achieved using riboflavin (vitamin B2), which plays the role of a photosensitizer. Dosed ultraviolet irradiation in this disease in the long-wave range (UV-A) promotes the formation of free radicals in the cornea and, consequently, chemical cross-links.
The treatment is simple and gentle for the patient. Local anesthetic drops are instilled into the eye before removing the corneal epithelium in the central part. A riboflavin solution is applied to saturate the stroma for half an hour before ultraviolet irradiation, which is also carried out for 30 minutes using a precisely calibrated instrument. Postoperative care is the same as for excimer laser photorefractive keratotomy, requiring the use of a therapeutic contact lens, as well as topical treatment for the next three days to increase comfort and accelerate epithelialization.