Prolactin has many names - lactation hormone, Luteotropic hormone (LTH), luteotropin, mammotropin, lactotropic or lactogenic hormone, Lactotropin, mammotropic hormone, Prolactin (PRL)
Prolactin can influence ovulation, delaying menstruation during lactation. This mechanism allows a woman to calmly feed her child without worrying about the onset of a new pregnancy. Due to the analgesic effect of prolactin, biting the nipple does not cause severe pain in the mother.
Three immunoreactive forms of the hormone are determined: monomeric (low molecular weight, monoPRL), dimeric and macroprolactin¹. MonPRL, which has greater biological activity, is most often detected in the blood. This article will discuss the indications for the analysis and its features, as well as the reasons for the deviation of the results from the norm, including in men.
Figure 1. Functions of prolactin in the female body. Source: Wikipedia and Russian Association of Endocrinologists
Blood test for prolactin
Prolactin is produced primarily in the adenohypophysis. This is the anterior lobe of the endocrine gland, which is located at the base of the brain. Prolactin synthesis also occurs in the cells of the placenta and decidua (the uterine mucosa modified due to pregnancy), immune organs, and structures of the central nervous system. The hypothalamus² is responsible for the regulation of these processes.
A certain level of PRL is detected not only in the blood, but also in the amniotic fluid surrounding the fetus, mucous secretions, and mother’s milk. A small amount of the substance is found in the cerebrospinal fluid - cerebrospinal fluid. A rarer source is hormone-producing tumors.
Prolactin in a blood test for hormones (Prolactin) is a significant indicator that can help with the diagnosis of female infertility³, tumors, and endocrine diseases. On the laboratory form it is indicated by the Russian name or abbreviation - PRL, PRL, LTH. The doctor may also prescribe determination of different fractions of the substance to clarify the suspected diagnosis.
Determining PRL in serum has its own difficulties, since there is a temporary change in concentration under physiological conditions (stress, physical activity, constitutional features) in the same person. Therefore, laboratories provide reference values in the form of digital ranges. The most common unit of measurement is mU/L (milli-international unit per liter of test material), but ng/ml (nanograms per milliliter) is also used. Converting ng/ml to honey/l is very easy - multiply the resulting value by 21.
Indications for analysis
A doctor prescribes a blood test if a pathological process is suspected. It makes no sense to just study prolactin levels. Referral can be given to both men and women as part of a comprehensive diagnostic search.
A prolactin test is often prescribed to overweight people who cannot lose weight even if they follow a diet and regularly go to the gym. An increase in PRL levels is accompanied by an increase in hunger. As a result, the body begins to store additional energy, which is normally needed by nursing mothers⁸.
Indications for women
Women are prescribed a prolactin test in the following cases:
- finding out the cause of infertility³;
- Irregular menstrual cycle or complete cessation/absence of menstruation (amenorrhea);
- diagnosis of breast diseases;
- the appearance of milky discharge from the nipples that is not related to breastfeeding or the postpartum period (galactorrhea);
- frequent miscarriages;
- imbalance between female and male sex hormones;
- miscarriage;
- pathological course of pregnancy in history, especially with premature delivery;
- suspicion of neoplasms (tumors) of the pituitary gland, ovaries;
- deterioration in the functioning of the thyroid gland with a subsequent decrease in hormone levels (hypothyroidism).
Symptoms of concomitant diseases help to suspect a problem. Patients note the cessation of menstruation, the appearance of male-pattern hair (around the nipples, on the shoulders or chin), and excessive sweating. However, diseases in the initial stages are often hidden, and then there will be no complaints².
Why should men take prolactin tests?
Under normal conditions, the male pituitary gland also produces small amounts of lactotropic hormone. It is necessary for the proper development of the genital organs, maintaining water-salt balance and the ability to reproduce the species - reproductive function. Prolactin also affects immunity, metabolic processes (metabolism), body weight, libido².
Patients may be recommended to study PRL levels for the following indications:
- erection problems - dysfunction up to impotence;
- decreased libido;
- high probability of developing a tumor in the pituitary gland;
- decreased sperm count;
- enlargement of the mammary glands (gynecomastia) of the female type;
- infertility.
Couples who cannot conceive a child for a long time usually undergo a joint examination, since the man’s health is no less important. A blood test for hormones allows you to suspect a possible source of disorders at an early stage, when the likelihood of successful treatment is highest.
A prolactin test is recommended for couples who are unable to conceive a child. Photo: gpointstudio / Depositphotos
What does high prolactin levels in the body mean?
Low prolactin levels are usually not a cause for concern in either women or men. High levels are normal during pregnancy and after childbirth.
Hyperprolactinemia, a high level of prolactin that occurs in men and non-pregnant women, occurs in 10% of the population.
Hyperprolactinemia can be caused by:
- anorexia;
- some diseases of the liver, kidneys;
- hypothyroidism;
- pituitary tumors;
- certain medications - risperidone and haloperidol, used in psychiatry, metoclopramide, used to treat nausea caused by cancer drugs;
- some common stressors - low blood sugar, intense exercise, and even mild forms of mental illness;
- some herbs - red clover or meadow clover, fenugreek, fennel.
Preparing for analysis
Testing can be done at any phase of the menstrual cycle, but results will vary due to normal fluctuations in prolactin concentrations throughout the month. Usually the attending physician himself chooses the required period if he suggests some kind of diagnosis. When searching for the causes of infertility, the patient is sent to donate blood on days 2-5 of the cycle, if necessary, including other hormones in the list of tests³.
Men don't need to worry about calendar intricacies. It is enough just to follow the recommended rules before performing the analysis.
Patients (both men and women) should begin preparing for the study in advance - the informativeness of the data obtained depends on this. For 2-3 days before analysis, it is necessary to exclude the influence of such factors:
- sex;
- severe psycho-emotional overload;
- alcohol;
- exhausting physical activity;
- bath, sauna;
- solarium;
- binge eating;
- unbalanced consumption of sweet, fatty, protein foods;
- additional stimulation of the mammary glands and nipples - during self-examination, sexual stimulation, wearing tight bras;
- lack of sleep;
- calorie deficit diet;
- psychoactive substances.
Blood is drawn from a vein in the usual way in the morning from 8 to 11-12 hours. The patient comes on an empty stomach - the last meal can be taken the night before, and dinner should be light. A few hours before submitting the material, give up cigarettes and other types of smoking (vaping, hookah).
A test for prolactin will be uninformative if you donate blood in the acute period of inflammatory diseases - colds (ARVI), sinusitis, pneumonia. There is also no point in conducting analysis in the first weeks after surgery and trauma, especially in the chest area. Some pharmaceutical drugs (antidepressants, hormones) affect the level of prolactin in the blood serum. Usually 3-5 days before testing, their use is suspended. However, you cannot stop the prescribed therapy yourself - consult your doctor.
Elevated prolactin levels - symptoms, causes, consequences
The limits of the norm are quite wide for women who are not pregnant or breastfeeding. From time to time, prolactin may rise above the upper level, and this does not necessarily indicate serious problems in the body. The level of the hormone can fluctuate due to emotional stress, taking certain medications, and other external physiological factors.
But a persistent and significant excess of the norm outside of pregnancy and breastfeeding is a cause for concern. You can suspect him based on the following signs:
- cycle disturbances up to the cessation of menstruation;
- vision problems (decreased visual acuity);
- discharge from the mammary glands;
- engorgement of the mammary glands, their enlargement;
- headache;
- decreased sexual desire;
- weight gain with normal physical activity and diet.
These signs do not give grounds to assert the presence of hyperprolactinemia. But if you find them in yourself, be sure to go to a gynecologist-endocrinologist.
Norms of prolactin in the blood
Laboratories use different equipment and test systems, so normal ranges may vary. This also applies to differences in units of measurement. The gender of the patient matters. The amount of hormones in the blood serum of women is subject to regular fluctuations throughout the menstrual cycle. Normal values change with age or pregnancy².
In children
The pituitary gland begins to produce PRL during fetal development.
Then its concentration drops in the first 1-1.5 months of life². Hormone production is enhanced in the presence of thyrotropin-releasing hormone and estrogen⁵. Table 1. Normal prolactin levels (ng/ml) in children of different age groups⁶
| Age, years | Floor | |
| M | AND | |
| 1-5 | 3,9-20,1 | 2,7-19,5 |
| 6-10 | 2,6-16,1 | 2,7-22,3 |
| 11-13 | 2,3-22,3 | 2,0-31,6 |
| 14-17 | 4,7-16,7 | 3,7-23,3 |
Before adolescence, the concentration of prolactin in girls and boys is almost the same. As young people develop, the ratio of sex hormones and prolactin changes towards adult levels⁵.
Among women
Table 2. Normal prolactin levels in healthy women⁶
| Biological state | Contents of the PRL | |||
| minimum | maximum | |||
| mIU/l | ng/ml | mIU/l | ng/ml | |
| Non-pregnant | 240 | 4,79 | 300-500 | 23,3 |
| 1st trimester | 500 | 23,5 | 2000 | 94 |
| 2nd trimester | 2000 | 94 | 6000 | 282 |
| 3rd trimester | 4000 | 188 | 10000 | 470 |
| Menopause | 107 | — | 290 | — |
Prolactin levels vary throughout the day. Diurnal fluctuations are subject to biological (circadian) rhythm². The maximum content in serum is reached 60-90 minutes after going to bed, and decreases during daylight hours⁷.
In men
In the body of men, prolactin enhances the effects of other pituitary hormones - luteinizing hormone (LH) and follicle-stimulating hormone (FSH). This stimulates Leydig cells, endocrine cells in the testicular area. Prolactin has a direct effect on testicular and seminal vesicle mass by regulating sperm activity².
In a healthy man, normal prolactin levels range from 80-265 mIU/L or 4.01-15.2 ng/ml⁷. Some laboratories indicate 500-540 mIU/L or 20-27 ng/ml as the upper limit.
Prolactin and the ability to have children
In some cases, high prolactin levels can lead to infertility. Prolactinoma tumors affect the pituitary gland, and it reduces the production of hormones. This condition is known as hypopituitarism. In men, it causes decreased libido and hair loss. In women, this can lead to infertility.
Hyperprolactinemia complicates pregnancy and disrupts the normal production of the hormones estrogen and progesterone. This causes the ovaries to either release eggs irregularly or stop producing eggs completely.
Medicines and other treatments for prolactinoma restore fertility in most women.
Causes of elevated prolactin
Hyperprolactinemia (high prolactin in the blood) can be physiological or pathological. In making the final diagnosis, the patient’s complaints, symptoms, anamnesis, and general examination data are of great importance. If necessary, the doctor prescribes additional examinations - MRI (magnetic resonance imaging), ultrasound of the thyroid gland, biochemical blood test⁴.
Figure 2. Risk factors for developing hyperprolactinemia. Source: Russian Association of Endocrinologists
Physiological reasons
In healthy people, temporary hyperprolactinemia can be detected, which occurs against the background of the following factors⁴:
- sexual intercourse within the previous 3-5 days;
- intense physical activity;
- deep sleep phase;
- lactation – period of breastfeeding;
- stressful situations;
- pregnancy;
- sleep disturbance;
- hypoglycemia (low blood glucose) at the time of the test;
- severe pain of another origin;
- obesity;
- nipple stimulation the day before.
The listed conditions are not an indication for reducing prolactin levels with medications. It returns to normal on its own after a few days. To exclude hidden (asymptomatic) diseases, the analysis is repeated after 5-7 days.
Pathological causes
Persistently elevated PRL may mean a disruption in the functioning of the hypothalamic-pituitary system due to the following reasons⁴:
- trauma to the chest, mammary gland;
- false pregnancy is a psychophysical disorder in which a healthy woman has signs of pregnancy in the absence of pregnancy;
- herpes zoster (herpes zoster);
- epilepsy;
- polycystic ovary syndrome;
- injuries or surgery on the brain in the place where the pituitary gland and hypothalamus are located;
- radiation exposure;
- acromegaly is a disease in which the bones of the skull and limbs become pathologically enlarged due to excessive synthesis of growth hormone (somatotropin);
- Rathke's pouch cyst (craniopharyngioma) is a benign brain tumor;
- cirrhosis of the liver;
- “empty sella” syndrome;
- hormone-producing tumors of the adrenal glands, ovaries;
- chronic kidney damage;
- hypothyroidism (primary) – the thyroid gland does not perform its functions to the required extent, which is accompanied by a decrease in the level of thyroid-stimulating hormones;
- other brain tumors: germinoma, prolactinoma, meningioma, metastases in the hypothalamic-pituitary system;
- micro- and macroadenomas of the pituitary gland;
- systemic (autoimmune) diseases – lupus, polyarthritis, thyroiditis;
- condition after abortion, miscarriage;
- deficiency of vitamin B6 (pyridoxine);
- chronic prostatitis;
- vascular malformations in the cerebral hemispheres.
Rarely, there are patients with an idiopathic form of hyperprolactinemia, the causes of which are unknown. In this case, persistent hyperfunction of pituitary cells is observed with a normal MRI picture. Patients predominantly complain of frequent headaches, blurred vision, and autonomic disorders (sweating, fluctuations in blood pressure, gastrointestinal disorders)⁴.
Taking pharmacological drugs
Hyperprolactinemia may be a side effect of long-term use of the following medications⁴:
- verapamil;
- furosemide;
- hormonal contraceptives with estrogens;
- some antidepressants: paroxetine, fluoxetine, amitriptyline, anafranil, doxepin, imipramine, moclobemide;
- reserpine;
- anticonvulsants: benserazide, methyldopa, levodopa;
- morphine;
- H2-histamine receptor antagonists: famotidine, ranitidine, cimetidine;
- metoclopramide;
- domperidone;
- neuroleptics;
- antihypertensive drugs.
Dopamine naturally inhibits the production of prolactin². All drugs that affect this neurotransmitter can lead to hyperprolactinemia. Most often this occurs with long-term treatment with neuroleptics, antidepressants, and antipsychotics⁴.
Taking certain medications can significantly affect prolactin levels. This must be taken into account before submitting the analysis. Photo: Matic.Sandra / Depositphotos
Patients with drug dependence syndrome - amphetamines, opiates, cocaine² are also at risk. If the doctor suspects pharmacological hyperprolactinemia, the blood test is repeated at least 72 hours after discontinuation of the substances⁴.
How to reduce the concentration of the hormone prolactin in women?
Elevated prolactin levels are far from harmless. It negatively affects the endometrium, the mucous layer of the uterus to which the embryo is attached. The endometrium becomes less sensitive and its thickness decreases. As a result, the egg, even if it has been fertilized, will not be able to attach to the wall of the uterus, that is, pregnancy will not occur.
- In addition to non-occurrence of pregnancy, an increase in prolactin concentration is accompanied by the following phenomena:
- Irregular menstrual cycle. The interval between “critical days” can increase significantly.
- Sexual desire is reduced or absent.
- Colostrum is released from the breast.
- There is more hair on the face, nipples, and lower abdomen.
If a woman plans to become pregnant, and the analysis shows increased production of prolactin, the specialist will select treatment taking into account the degree of hyperprolactinemia:
- With moderate hyperprolactinemia (not higher than 1000 mU/l), hormone therapy is most often not needed. However, the doctor may recommend vitamin and mineral complexes that normalize the hormonal balance in general. For example, the drug Pregnoton includes extract of Vitex sacred, which eliminates hormonal imbalance and gently regulates the cycle. The effectiveness of the drug for hyperprolactinemia has been proven in clinical studies (more information about the product can be found here).
- High-grade hyperprolactinemia (more than 1000 mU/l) can be caused by neoplasms in the pituitary gland. In such a situation, it is possible to remove the tumor through surgery or radiation. Therapy often involves taking hormonal medications.
Many women prefer to rely on traditional medicine, which promises to reduce prolactin concentrations without pills. Traditional methods can be effective only if they are used as an addition to drug therapy. Therefore, it is better to influence the pathology in a comprehensive manner.
In addition, with increased prolactin production, a woman should follow the following recommendations:
- Avoid stressful situations.
- Eliminate foods with flavor enhancers and preservatives from your diet. But it’s worth adding eggs, fruits, legumes, fish and meat to the menu.
- Normalize your daily routine. Pay special attention to getting enough sleep.
- Stop smoking, alcohol, coffee and black tea. If starting your morning with coffee or strong black tea has been a long-standing ritual without which you won’t feel invigorated, try an alternative - chicory or green tea.
As for traditional medicine for normalizing hormonal levels, perhaps the most effective of them is sacred vitex (common twig, tree of Abraham, tree of purity). Its positive effect on prolactin levels is also recognized by traditional medicine. In particular, Vitex extract is part of the Pregnoton complex, which is used to reduce prolactin.
Causes of low prolactin
Reasons for detecting low BPD include the following conditions⁹:
- Sheehan's syndrome - pituitary infarction that occurs against the background of massive bleeding during childbirth;
- bleeding associated with uterine fibroids;
- irregular meals with long breaks between meals, fasting;
- compression of the pituitary gland due to anomalies of surrounding tissues ("empty sella" syndrome), nearby tumors, injuries, underdevelopment of the bone structures of the skull;
- a history of significant blood loss not related to childbirth;
- radiation damage to the central nervous system;
- smoking;
- true post-term pregnancy (more than 41 weeks);
- long-term therapy with antipsychotic, hormonal, opioid drugs;
- hyperglycemia – a persistent increase in the concentration of glucose in the blood serum;
- alcohol dependence syndrome;
- tuberculosis.
Hypoprolactinemia (low PRL in the blood) most often occurs in women with a history of massive bleeding⁹. Accompanied by impaired libido and the ability to procreate (fertility)².
How to reduce or increase prolactin
If elevated levels are not associated with a tumor or other serious disease, you can start with nutritional correction. It is recommended to add the following foods fortified with folic acid to your diet:
- nuts;
- offal 1-2 times a week;
- sea fish (fatty);
- lean meat;
- fresh vegetables, herbs;
- chicken eggs;
- flax seeds or their oil.
Foods fortified with folic acid (vitamin B9) help increase prolactin levels in the blood.
Photo: yarunivphoto / Depositphotos A diet high in gluten also increases prolactin levels in the blood. For minor hypoprolactinemia, the following products help:
- bakery products;
- fresh baked goods;
- quinoa;
- fenugreek;
- whole grain oats.
Hyperprolactinemia associated with a tumor process is tried to be treated conservatively with the help of dopamine agonists. Drug therapy can last from several months to 2 years⁴. If the patient is intolerant or resistant to drugs, surgery is recommended through the nasal cavity (transsphenoidal surgery)². Radiation therapy is used only in extreme cases⁴.
What else should I try?
Ways to reduce prolactin levels:
- change your diet;
- try to keep stress under control;
- limit intense exercise;
- Wear comfortable clothes that do not cause chest discomfort or stimulate the nipples;
- Take vitamin B6 and vitamin E – vitamin B6 is involved in the production of dopamine and higher levels can lower prolactin levels, and vitamin E prevents prolactin levels from rising;
- avoid anabolic steroids;
- take zinc supplements.
If you find an error, please select a piece of text and press Ctrl+Enter
Sources
- Bulatov A.A., Makarovskaya E.E., Marova E.I., Melnichenko G.A. Hyperprolactinemia with a predominance of high molecular weight immunoreactive prolactin: differences in the regulation of the level of high molecular weight and monomeric forms in the blood. Problems of Endocrinology. 1995;41(6):19-23
- Melnichenko G.A., Marova E.I., Dzeranova L.K., Vaks V.V. Hyperprolactinemia in women and men: A manual for doctors. M. 2008.
- Clinical recommendations of the Ministry of Health of the Russian Federation. Female infertility. Year of approval (revision frequency): 2021.
- Federal clinical recommendations of the Ministry of Health of the Russian Federation on hyperprolactinemia: clinical picture, diagnosis, differential diagnosis and treatment methods. 2021.
- Hyperprolactinemia syndrome in children and adolescents: causes, diagnosis, treatment. / V.V. Smirnov, F.I. Morozkina, M.D. Utev // Attending Physician. – 2014. – No. 12.
- Ph.D. Nebyltsova O.V., Klimova Zh.A., Nosenko G.A., Boyko I.V., Ph.D. Klishnya M.A., Chernyshova L.A., Knyazeva L.P., Malikova S.V., Danilova I.E., Abasheva S.N., Degtyarenko O.A., Prishchepa L.A. Laboratory handbook. 2011
- Obstetrics: national guide / ed. G. M. Savelyeva, G. T. Sukhikh, V. N. Serov, V. E. Radzinsky. — 2nd ed., revised. and additional - M.: GEOTAR-Media, 2021. - 1088 p. — (Series “National Guidelines”). — ISBN 978-5-9704-4551-8
- Crowley WR, Ramoz G, Torto R, Keefe KA, Wang JJ, Kalra SP. Neuroendocrine actions and regulation of hypothalamic neuropeptide Y during lactation. Peptides. 2007;28(2):447-452. doi:10.1016/j.peptides.2006.09.025
- Nad Yu.G. Hypoprolactinemia syndrome - a right to exist? // Eurasian Union of Scientists. 2015. No. 9-4 (18).
Prolactin is one of the hormones of the anterior pituitary gland. According to its chemical structure, it is a peptide hormone consisting of 199 ^ amino acid residues. Prolactin is secreted in lactotropic cells of the anterior pituitary gland, which constitute from 11 to 29% of the total cellular composition of the adenohypophysis. There is also extrapituitary secretion of prolactin, the significance of which, however, has not been definitively established [1].
Like human growth hormone, pituitary secretion of prolactin is under direct hypothalamic control and is not regulated by feedback. The hypothalamic-pituitary system has both an inhibitory and stimulating effect on prolactin secretion through neuroendocrine, autocrine and paracrine mechanisms [2]. The secretion of prolactin is constantly inhibited by the hypothalamic hormone dopamine. Dopamine is produced in neurons of the paraventricular and gray tuberous nuclei, as well as in neurons of the infundibulum nucleus and arcuate nucleus of the hypothalamus.
The inhibitory effect of dopamine is realized through stimulation of dopamine receptors localized on lactotropic cells. There are 2 types of dopamine receptors: Dj and D2. D1 receptors stimulate adenylate cyclase, and D2 receptors inhibit it. Dopamine and its agonists stimulate D2 receptors, which leads to inhibition of adenylate cyclase, a decrease in the amount of intracellular cAMP and a decrease in prolactin secretion. It is on this stimulation of D2 receptors that the effect of the therapeutic action of dopamine agonists (L-dopa, apomorphine, dopamine, bromocreptine, cabergoline) in the treatment of hyperprolactinemia is based. Estrogens, dopamine antagonists (phenothiazines, metoclopramide), serotonergic agonists (5-hydroxytryptophan), adrenergic inhibitors, sympatholytics (reserpine, α-methyldopa), opiates, acetylcholine, oxytocin, serotonin, have a prolactin-stimulating effect. melanostimulating hormone, TSHR (thyrotropin-releasing hormone), neurotensin, and hypoglycemia [3].
Prolactin, like other hormones, has a circadian rhythm of secretion. The maximum concentration of prolactin in human blood plasma is observed during sleep, the minimum level is in the morning, during awakening [4].
There are a number of physiological conditions accompanied by an increase in prolactin levels. Such conditions include, first of all, pregnancy and breastfeeding. In men, a physiological rise in prolactin levels can be observed during sleep, during intake of protein foods, physical activity, and in response to stress.
Pathological hyperprolactinemia is an increase in prolactin levels against the background of a particular disease or taking medications. Pathological hyperprolactinemia develops as a result of anatomical or functional disorders of the hypothalamic-pituitary system. In accordance with its origin, pathological hyperprolactinemia can be conditionally divided into hyperprolactinemia of tumor origin (prolactinoma) and non-tumor origin. In some cases, when it is not possible to establish the cause of pathological hyperprolactinemia, they talk about the idiopathic form of hyperprolactinemia, in which the function of pituitary cells increases, but their number does not change [2].
The level of prolactin can suggest the nature of hyperprolactinemia. An increase in prolactin levels by 1.5-3 times usually indicates non-tumor hyperprolactinemia. Hyperprolactinemia with an increase in prolactin levels from 2000 to 4500 mIU/l is observed, as a rule, with pituitary microadenomas; an increase in prolactin over 4500 mIU/l is typical for pituitary macroadenomas [5].
Prolactin has an effect on almost all organs and systems, so the clinical picture of hyperprolactinemia is extremely polymorphic.
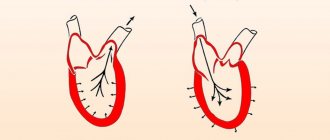
| Figure 1. Regulation of prolactin secretion |
Table 1. Etiological factors of hyperprolactinemia
| Pathological hyperprolactinemia | Primary diseases of the hypothalamus and pituitary gland
Microadenoma (diameter up to 10 mm) Macroadenoma (diameter more than 10 mm) Rupture or transection of the pituitary stalk Empty sella syndrome Neurogenic stimulation Chest trauma or surgery Herpes zoster Excess TSHR (thyrotropin-releasing hormone) Primary hypothyroidism Idiopathic hyperprolactinemia Metabolic causes
Chronic renal failure and systemic hemodialysis Ectopic secretion of prolactin Neoplasms |
| Drug-induced hyperprolactinemia | Antihypertensive drugs (reserpine, methyldopa, verapamil) Dopamine receptor blockers
Estrogens Drugs (morphine, heroin, cocaine) Antiulcer drugs (cimetidine) |
| Kalinchenko S.Yu. A step forward in the treatment of hyperprolactinemia. Selected lectures. M., 2010.[2] | |
One of the main manifestations of hyperprolactinemia is impaired sexual and reproductive function, caused by a decrease in the secretion of gonadotropins against the background of hyperprolactinemia. In men, these disorders are expressed in decreased sexual desire and erectile dysfunction (ED) (50-85%), infertility due to oligozoospermia and ejaculation disorders (3-15%), gynecomastia (6-23%). With sexual dysfunction in men, hyperprolactinemia is detected in 0.4-11% of cases, and in some studies reaches 20%, therefore, studying the level of prolactin in the blood is an important step in diagnosing the causes of sexual dysfunction in men and ED in particular, as the most frequent manifestations of sexual dysfunction. In most cases, ED is only a symptom of the disease, so treatment should be comprehensive and aimed at eliminating the underlying problem. In the case of hyperprolactinemia, even a slight increase in prolactin levels can lead to erectile dysfunction. Therefore, in many cases, ED may be a marker of hyperprolactinemia [7]. At the same time, the diagnosis of hyperprolactinemia in men is complicated by the fact that characteristic complaints (decreased libido, ED and infertility) are not always associated with the presence of serious endocrinopathy. According to Buvat J., Lemaire A. (1997), hyperprolactinemia was detected in 3.18% of men with ED [8]. A high incidence of hyperprolactinemia (19.3%) among men with sexual disorders was reported by N. Grafeille (1997).
| Figure 2. Erectile function scores according to the IIEF scale in the main group of patients with ED (n = 1148) and the group of patients with hyperprolactinemia (n = 69) |
Other clinical manifestations of hyperprolactinemia are psychoemotional disorders, such as irritability, anxiety, depression, memory and mood deterioration, and sleep disturbances.
Neurological symptoms occur in patients with tumors of the hypothalamic-pituitary region and are caused directly by tumor growth. These symptoms include: headache, dizziness, visual disturbances (limited visual fields, double vision, decreased visual acuity).
Patients with prolactinemia may experience certain symptoms of endocrine disorders caused by loss of other pituitary functions (symptoms of pituitary insufficiency), such as symptoms of hypothyroidism (with decreased TSH secretion), symptoms of adrenal insufficiency (with decreased ACTH secretion), symptoms diabetes insipidus (with a decrease in the secretion of antidiuretic hormone), symptoms of hypogonadism (associated with a decrease in the secretion of LH, FSH). Some endocrine symptoms are caused directly by an increase in prolactin levels. These include galactorrhea, obesity, and insulin resistance.
TREATMENT OF HYPERPROLACTINEMIA
For all forms of hyperprolactinemia, incl. and tumor genesis, the main method of treatment is medication. Drug treatment is carried out using dopamine agonists, among which cabergoline (a third generation dopamine agonist) is currently the drug of choice. First generation dopamine agonists include lysergic acid derivatives (bromocriptine, methysergide), aminoergoline derivatives (lisuride, tergulide, mesulergine), clavine derivatives (pergolide, metergoline). Bromocriptine is the most common first generation dopamine analogue, which for a long time remained the “gold standard” in the treatment of hyperprolactinemia, effective in reducing prolactin levels and restoring reproductive and sexual function. In most patients, treatment with bromocriptine leads to a number of side effects, such as drowsiness, dizziness, headache, orthostatic decrease in blood pressure, nausea, vomiting, which is the reason for refusal of treatment in 12% of patients.
The imperfection of dopamine analogues of the first generation became the basis for the creation of new dopamine agonists of the second generation (quinagolide) and third generation (cabergoline), which today are the drugs of choice in the treatment of any form of hyperprolactinemia, more selective for D receptors and characterized by greater efficiency and better portability.
When treating erectile dysfunction in patients with hyperprolactinemia, normalization of prolactin levels comes to the fore. For this purpose, dopamine agonists are used, which are used in the first stage of treatment as monotherapy. In most cases, monotherapy with dopamine agonists restores erectile function. If monotherapy with dopamine agonists is ineffective, which is most often due to hypogonadism concomitant with hyperprolactinemia, therapy aimed at normalizing testosterone levels, as well as therapy with phosphodiesterase type 5 inhibitors (PDE-5), is prescribed. So according to Carani S. et al. (1996), treatment with bromocriptine restored erectile function before the level of testosterone in the blood increased (a decrease in libido may be a consequence of both dishormonal disorders and, possibly, the direct effect of prolactin on the brain) [9].
MATERIALS AND METHODS OF RESEARCH
We examined a large sample of patients with ED of various etiologies (n=1148). Hyperprolactinemia was detected among patients of the general group in 69 (9%) observations. In a retrospective study of 69 adult men with hyperprolactinemia, the dominant clinical symptoms were predominantly endocrine in nature. Decreased or absent libido was detected in 58 (84%), gynecomastia - 12 (17.4%), galactorrhea - 2 (2.9%), rare beard growth was noted in 4 (5.8%) patients. Focal cerebral symptoms were present in 23 (33.3%), headache in 15 (21.7%), limited visual fields in 4 (5.8%), diplopia in 2 (2.9%) patients. Testicular volume was normal (> or = 15 cm3) in all patients except five who had signs of late pubertal development. A decrease in visual acuity was noted in 32 (46.4%) patients. Increased fatigue among patients with hyperprolactinemia was detected in 29 (42%) patients, sleep disturbances in 31 (44.9%). Serum prolactin levels ranged from 360 to 8000 mU/L (mean 1200 mU/L, normal range
Data from sexological testing (IIEF scale) demonstrated the prevalence of more severe ED symptoms among patients with hyperprolactinemia compared to all patients in the general group (Figure 2).
When examined, 20 (28.9%) patients with hyperprolactinemia had low testosterone levels (
RESULTS AND ITS DISCUSSION
In our study, hyperprolactinemia was detected in 9% of cases, clinically manifested by a wide range of neurovegetative disorders against the background of pronounced manifestations of ED. These pathological symptoms were successfully relieved by a 1-2 month course of pathogenetic therapy with drugs that reduce the level of prolactin in the blood plasma.
Thus, testing the concentration of prolactin in the blood is an important step in diagnosing the causes of ED and should be performed in all patients with complaints of decreased erection quality.
Key words: erectile dysfunction, hyperprolactinemia, treatment, dopamine agonists, bromocriptine, quinagolide, cabergoline.
Keywords: erectile dysfunction, hyperprolactinemia, treatment, dopamine agonists, Bromocriptine, quinagolide, cabergoline.
LITERATURE
- Dedov I.I., Melnichenko G.A., Romantsova T.I. Hyperprolactinemia syndrome. M. 2004.
- Kalinchenko S.Yu. A step forward in the treatment of hyperprolactinemia. Selected lectures. M. 2010.
- Dzeranova L.K. Hyperprolactinemia syndrome in women and men: clinical picture, diagnosis, treatment: Dis. ... Dr. med. Sci. M. 2007.
- Dedov I.I., Dedov V.I. Biorhythms of hormones. M. 1992.
- Casanueva FF, Molitch ME, Schlechte JA, Abs R., Bonert V., Bronstein MD, Brue T., Cappabianca P., Colao A., Fahlbusch R., Fideleff H., Hadani M., Kelly P., Kleinberg D ., Laws E., Marek J., Scanlon M., Sobrinho LG, Wass JA, Giustina A. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas // Clin Endocrinol (Oxf). 2006. Vol. 65. No. 2. P. 265-73.
- Bhasin S., Enzlin P., Coviello A., Basson R. Sexual dysfunction in men and women with endocrine disorders // Lancet. 2007. Vol. 369. No. 9561. P. 597611.
- Johri AM, Heaton JP, Morales A. Severe erectile dysfunction is a marker for hyperprolactinemia // Int J Impot Res. 2001. Vol. 13. No. 3. P. 176-82.
- Buvat J., Lemaire A. Endocrine screening in 1,022 men with erectile dysfunction: clinical significance and cost-effective strategy / J Urol. 1997. Vol. 158. No. 5. P. 1764-1767.
- Carani C., Granata AR, Fustini MF, Marrama P. Prolactin and testosterone: their role in male sexual function // Int J Androl. 1996. Vol. 19. No. 1. P. 48-54.
| Attached file | Size |
| 730.96 kb |
‹ Endovideosurgery in pediatric urology, reconstructive plastic surgery in children Up Stages and prospects for the development of oncological urology in the Research Institute of Urology ›