Eosinophils consist of a bilobed nucleus and three types of eosinophil granules (lipid bodies, eosinophils, small and primary). They contain protein structures with the help of which foreign cells are neutralized. Eosinophils are quite large cells: their diameter reaches 20 microns.
Eosinophils got their name due to the fact that when stained according to Romanovsky, they are easily stained with eosin (an acidic dye), while other types of dyes have no effect on them. Eosin itself was invented in 1873 by the German scientist G. Caro and, due to its bright pink color, was named after the ancient Greek goddess of the dawn Eos (in the German version the name sounds like “eosin”).
Blood test for eosinophils
To determine the level of eosinophils, a general blood test is used, which is familiar to all of us since childhood. Eosinophils by themselves do not give an accurate idea of the nature of pathological changes in the body, however, in combination with other values of the leukocyte formula, they allow a specialist to judge the nature of the pathology. In the analysis form, eosinophils are designated as EO. Their content is indicated as a percentage of the total number of leukocytes. A formula is also used to calculate the absolute number of eosinophils in peripheral blood and it looks like this: number of leukocytes * 10 to the 9th power. For a general analysis, blood is most often taken from a finger prick, but venous blood is also suitable.
Figure 1. Causes of eosinophilia (increased number of eosinophils in the blood). Image: kavusta/Depositphotos
Indications for analysis
A complete blood test with a count of eosinophils is prescribed for most people who visit the clinic. The range of indications is very wide, but in modern clinical practice, the initial eosinophil count is most often used as a biomarker to assess the effectiveness of drugs prescribed to patients with bronchial asthma. In this regard, the absolute number of eosinophils is of greatest value to the physician.
Eosinophils belong to microphages. This means that they can only absorb small foreign particles.
The study is relevant when confirming a preliminary diagnosis, checking the effectiveness of the prescribed therapeutic course, assessing the state of a person’s health during medical examinations or medical examinations. The doctor also prescribes a general blood test in the postoperative period. In addition, counting eosinophils is important when the development of infectious, oncological and autoimmune diseases is suspected.
Norms of eosinophils in the blood
When deciphering the analysis, the patient’s age is taken into account, since these factors affect the content of eosinophils in the blood.
Table 1. Norm of eosinophils by age
| Children under 5 years old | Children 5 – 14 years old | Adults |
| 0,5 – 7% | 1 – 5% | 0,5 – 5% |
It should also be taken into account that in women in the first days of menstruation there is a slight excess of the norm in the content of eosinophils, while after ovulation their number may be slightly below the norm.
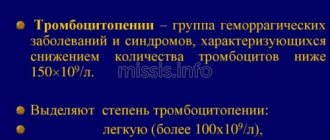
In absolute terms, the norm for adults is 0.15-0.450X10.0⁹ per liter of blood plasma. Exceeding the normal percentage of leukocytes is called eosinophilia. There are three stages of eosinophilia:
1. Light (no more than 10% of the total number of leukocytes).
2. Average (up to 15%).
3. Heavy (over 15%).
Causes of an increased number of eosinophils in the blood
An increase in the level of eosinophils indicates that the body is resisting the inflammatory process, and tissues and cells are experiencing oxygen deficiency. Possible reasons for the increase in the number of eosinophils:
- Allergy. This is one of the most common reasons. Hypersensitivity reactions always increase the production of eosinophils in the bone marrow. In turn, eosinophils reduce the production of allergy mediators.
Allergies are a common cause of elevated eosinophil levels. Photo: Dmyrto_Z / Depositphotos
- Asthma. In bronchial asthma, there is a moderate increase in the number of eosinophils in the blood, and in the allergic form they can also be found in sputum and bronchoalveolar fluid.
- Helminthic infestations. When infected with helminths, the number of eosinophils in the blood increases for two reasons: first, they release eosinophil cationic protein and reactive oxygen species to kill parasites. Secondly, the metabolic products of parasites provoke hypersensitivity reactions, and here the mechanism for increasing the production of eosinophils is the same as in allergies.
- Lung diseases. Despite the fact that the mechanism of increased eosinophil production in lung diseases has not yet been fully studied, experts note the relationship between these phenomena. Eosinophilia is observed in Churg-Strauss syndrome (in this case it reaches a frightening figure of 50%), allergic bronchopulmonary aspergillosis (an increase in the level of eosinophils is observed only in the acute phase and rarely exceeds 15%), as well as in eosinophilic pneumonia (up to 20%).
- Blood diseases. First of all, we are talking about hematological pathologies of a malignant nature (eosinophilic leukemia, myeloid leukemia). Eosinophilia is also characteristic of mastocytosis, but in leukemia its severity is much higher (up to 70%).
- Gastrointestinal diseases. An increased number of eosinophils in a general blood test is observed in gastritis, esophagitis and enterocolitis. All these diseases are accompanied by inflammatory processes, which causes accelerated formation of eosinophils.
- Oncological diseases. When confirming the diagnosis, the leukocyte count is not a priority indicator, but an increase in the number of eosinophils in malignant diseases is indeed observed. After therapeutic interventions such as radiotherapy, the increase in the number of eosinophils also increases significantly.
- Weakened immunity. In immunodeficiency conditions (Wiskott-Aldrich syndrome and Jobe syndrome), the level of eosinophils can reach 60%, which is associated with increased production of immunoglobulin E.
- Endocrine diseases. In diseases such as primary adrenal insufficiency (Addison's disease), congenital adrenal dysfunction, Schmidt's syndrome and panhypopituitarism, eosinophil levels increase to moderate levels and normalize after treatment with glucocorticoids.
- The recovery period after surgery. This is especially true when transplanting donor organs to a patient and removing the spleen.
Eosinophilia in a child: differential diagnosis
A 7-year-old boy was admitted to the hospital with fever, lymphadenopathy, hepatosplenomegaly, and eosinophilia. Two months before the development of fever and confusion, the child was healthy. He was admitted to another hospital where he developed seizures. Meningoencephalitis was diagnosed, intravenous antibiotics were prescribed, and he was treated with finytoin and carbamazepine. After improvement, he was discharged with continuation of two medications; Phenytoin was discontinued after one month. Two weeks before admission to the hospital, fever reappeared, especially in the early morning hours; the temperature reached 38.90C, with anorexia. Eleven days before admission, the physician discovered generalized lymphadenopathy and hepatosplenomegaly. The results of laboratory tests are presented in Tables 1 and 2. Tests for heterophilic agglutinins and antibodies to Borrelia buurgoferi and cytomegalovirus were negative. Radiographs of the chest and abdomen were normal except for splenomegaly.
| Table 1 Hematological laboratory data | ||||
| 11 days before admission | On admission | On the 4th day of hospitalization | on the 5th day of hospitalization | |
| Hematocrit % | 37 | 32,6 | 31,7 | 31,4 |
| Reticulocytes % | 2,6 | |||
| ESR | 10 | |||
| Leukocytes (per mm3) | 11 400 | 5 600 | 15 600 | 22 400 |
| Neutrophils | 32 | 4 | 5 | 5 |
| Band forms | 7 | 5 | 2 | |
| Lymphocytes | 21 | 39 | 65 | 66 |
| Metamyelocytes | 1 | |||
| Atypical lymphocytes | 5 | 3 | 11 | |
| Monocytes | 6 | 6 | 3 | 7 |
| Eosinophils | 27 | 46 | 22 | 10 |
| Basophils | 1 | — | — | — |
| Platelets ((per mm3) | 294 000 | 264 000 | 289 000 | 327 000 |
| Prothrombin time (sec) | 13,3* | |||
| Partial thromboplastin time (sec) | 33,7 | |||
| * Reference value 11 seconds | ||||
| Table 2. Blood chemistry data | |||
| 11 days before admission | On admission | on day 5 of hospitalization | |
| Glucose (mg/dl) | 140 | ||
| Uric acid (mg/dl) | 2,1 | ||
| Phosphorus (mg/dl) | 8,9 | ||
| Protein (g/dl) Albumin Globulin | 6,6 2,9 2,7 | ||
| Sodium (mmol/liter) | 133 | ||
| Potassium (mmol/liter) | 4,1 | ||
| Chlorides (mmol/liter) | 100 | ||
| CO2 (mmol/liter) | 26,9 | ||
| Lactate dehydrogenase (U/liter) | 429 | 493 | 487 |
| Aspartate aminotransferase (U/liter) | 49 | ||
| To convert the glucose value to mmol/L, multiply by 0.05552. To convert uric acid values to micromoles per liter, multiply by 59.48. To convert phosphorus values to millimoles per liter, multiply by 0.3229 | |||
Three days before admission, rashes appeared on the boy’s arms, elbows, and popliteal area. Carbamazepine was discontinued. The temperature remained, giving daily peaks, increasing to 400C. On the day of admission, the patient vomited twice and was admitted to the hospital. The boy's medical history was unremarkable. His parents and 13-year-old brother were healthy. The patient received all necessary vaccinations. The family had a cat. There was no history of chills, sweats, headache, diplopia, photophobia, neck symptoms, dysuria, diarrhea, myalgia, arthralgia, bleeding or bruising, scratches, bites, insect stings, eating raw foods, or traveling outside of New England for a period of time. the previous year. The temperature was 38.9º C, pulse rate 110 and respiratory rate 20. Blood pressure = 95/50 mm Hg. On examination, the patient is pale and apathetic. There was a tender, almost confluent maculopapular rash on the forearms without pruritis, with petechiae on the lower legs and ankles. Foci of discrete, firm, nontender cervical and submaxillary lymph nodes, the largest of which were 3 cm in diameter, were identified bilaterally; A small number of supraclavicular lymph nodes and bilateral axillary and inguinal lymph nodes approximately 1 cm in diameter were palpable. The head is normal, the neck is supple. A grade 2 systolic murmur was heard along the left sternal border. The edge of the liver was 6 cm below the right lower rib. No tension was detected over the spine or costovertebral angles. The arms and legs, including the joints, were normal, including the genitals. Neurological examination is normal. The urine is normal, as are the levels of urea, creatinine, bilirubin, calcium, magnesium, creatine crinase, and alkaline phosphatase. The carbamazepine concentration was less than 5 mg per millimeter. The results of other laboratory tests are presented in Tables 1 and 2. Chest radiography is normal except for a diffuse interstitial pulmonary pattern. Abdominal radiography revealed a splenic length of 13 cm and hepatomegaly. Intestinal gases were not expressed and the bones were in order. No intra-abdominal calcifications were detected. Tests for heterophile agglutinins and cytomegalovirus antibodies were negative, and microscopic examination of thick and thin blood smears did not reveal either malaria or babesiosis. Preventive measures were taken against neutropenia. Blood and urine samples were sent for culture and intravenous fluids and ticarcillin-clavunate sodium were prescribed. The temperature rose to 41.10 C; acetomifene and ibuprofen were given as needed, as was cooling swaddling. On the second day of hospital stay, the temperature was 40.8°C, and the next day 40°C. Subsequently, the fever went away without additional use of antipyretics. No convulsions were noted. On the fourth day of hospital stay, the studies were repeated (Table 1). On the fifth day, the patient felt relatively well and there was a slight decrease in the size of the lymph nodes, liver and spleen with blanching of the rash. The values of uric acid, bilirubin, aspartate and alanine aminotransferases were normal. The results of other laboratory tests are presented in Tables 1 and 2. Bacteriological cultures were negative. Antibiotic treatment was discontinued.
Differential diagnosis
Dr. Jed B. Gorlin: The differential diagnosis in this case is quite extensive. I will approach it from the causes of eosinophilia in children (Table 3). Peripheral eosinophilia is relatively uncommon in New England, where it is most often associated with allergic diathesis.
| Table 3. Causes of eosinophilia in children |
| Allergies Asthma, atopic eczema, urticaria, hay fever, drug reactions |
| Skin disorders Pemphigus, toxic epidermal necrolysis |
| Tumors Hodgkin's disease, myeloproliferative syndromes, acute lymphocytic leukemia (variant) |
| Hereditary disorders Idiopathic conditions |
| Various violations Chronic hepatitis, regional enteritis, rheumatoid arthritis, periarteritis nodosis, peritoneal dialysis, Addison's disease |
| Parasitic infections Ascariasis, trichinosis, infectious echinococcus, hookworm infection, strongyloides infection, filariasis infection, toxocariasis, Pneumocystis carinii infection, malaria, amoebiasis |
| *Adapted from Anderson et al. with the permission of the publisher |
Before considering these diagnostic possibilities, I will need to provide an overview of the current understanding of eosinophil biology. Boyce et al. recently reconsidered this problem, classifying the eosinophil as a sibling of the basophil, since their progenitors share common granules and contain histamine. The normal number of eosinophils in the blood ranges from 0 to 450 per microliter, although there is diurnal variation with the highest number in the morning. These cells have large acidophilic cytoplasmic granules and a bilobular nucleus and are limited to tissue fluid, probably due to selective need. There are approximately 200 tissue eosinophils for every 1 eosinophil in the blood. Cytokines produced by T cells, especially interleukins 3 and 5 and granulocyte-macrophage colony-stimulating factor, have eosinophilopoietic activity. Interleukin 5 activity appears to be most specific for eosinophils. A transgenic mouse that produces human interleukin 5 has significant eosinophilia but remains healthy. This information may have clinical implications, as the leading cause of eosinophilia at the Mayo Clinic was the use of granulocyte-macrophage colony-stimulating factor in cancer treatment, and eosinophilia was an adverse effect in a recent study using interleukin 3 Interleukin-3, interleukin-5, and granulocyte-macrophage colony-stimulating factor appear to prolong eosinophil circulation and probably their life cycle by antagonizing apoptosis. Corticosteroids, which are effective in many eosinophilic diseases, may also induce apoptosis or inhibit the production of cytokines by eosinophils. Some of these cytokines may increase the ability of eosinophils to recruit additional eosinophils (Table 4).
| Table 4 . Biological features of eosinophilia |
| Characteristic Bilobular nucleus Large acidophilic granules |
| Eosinophilic cytokines Granulocyte-macrophage colonies stimulating factor Interleukins 3 and 5* |
| Cytokines produced by eosinophils Interleukins 1, 3, 4, 5, 6 and 8 Tumor-necrotizing factor a Transforming growth factor a and b Major inhibitory protein 1a Granulocyte-macrophage colony stimulating factor |
| Composition of granulocytes Small lysosomal granules Phagocyto oxidase proteins that produce superoxide |
| Large lysosomal granules Eosinophil peroxidase Major basic protein Eosinophil cationic protein Neurotoxin produced by eosinophils |
| Adapted from Boyce with the permission of the publisher |
Like other granulocytes, eosinophils appear to have protective properties such as superoxide production and unique effector mechanisms that include cytotoxic effects directed against parasites and the activity of specific cytotoxic granule proteins. The beads are filled with cationic proteins, including eosinophil peroxidase, large basic protein, eosinophil cationic protein, and eosinophil-produced neurotoxin, so named because it causes central nervous system dysfunction when administered intracerebrally in animals (“Gordon phenomenon”). Can we take a look at the pictures?
Dr. Susan A. Connoly: A single posteroanteral radiograph of the chest and abdomen shows diffuse interstitial accentuation bilaterally and marked hepatosplenomegaly.
Dr. Gorlin: Eosinophilia can be associated with allergic reactions to many drugs. Adverse skin reactions that develop in 2 to 3 percent of hospitalized patients include Stevens-Johnson syndrome, toxic epidermal necrolysis, hypersensitivity syndromes, small vessel vasculitis, serum sickness, and angioedema. Hypersensitivity symptoms, which may include arthralgias, eosinophilia, fever, liver dysfunction, lymphadenopathy, and rash, are most consistent with this case. The clearest association of hypersensitivity syndromes is with anticonvulsant drugs—especially phenytoin and carbamazepine (which the patient was taking)—occurring in 1 in 5,000 people taking these drugs. The syndromes develop approximately two to six weeks after starting these drugs and usually present with fever, rash, and lymphadenopathy. Hepatitis and hematologic abnormalities, especially eosinophilia and atypical lymphocytosis reminiscent of infectious mononucleosis, are quite common. Symptoms often disappear when the drugs are stopped, although the reaction may progress to lymphoma. Cure is usually complete, and corticosteroid therapy has been reported to hasten resolution of the rash and recovery of liver enzymes. Although many of these signs and symptoms are consistent with those in this case (including a six-week delay in the onset of symptoms), progression of symptoms over several weeks after both drugs were discontinued and mild hepatitis as evidenced by elevated enzyme levels, in contrast to significantly clinically pronounced hepatomegaly casts doubt on this diagnosis. The most well-known forms of acquired eosinophilia are those resulting from contaminated tryptophan and toxic oil. Eosinophilia-myalgia syndrome caused by contaminated tryptophan was often fatal in part due to cardiac involvement and eosinophilic infiltration. Toxic oil syndrome, which occurred in northeastern Spain in 1981, was characterized by fever and respiratory distress accompanied by peripheral eosinophilia and myalgia in some people who consumed cooking oil containing aniline-denatured stolen oil. Our patient was clearly not taking any other medications than those listed in the medical history, but he and his parents should be carefully questioned about taking vitamins or other medications, since many patients insist that they did not take medications but confirm taking pills “as a additives." The most common cause of eosinophilia worldwide is parasitic infection, particularly by helminths that have invaded tissue. Eosinophilia is not common in malaria, giardiasis or amoebiasis but it can be observed in cases of intestinal coccidia infection. In a recent summary of cases of eosinophilia, Weller divided parasitic helminths into those that cause moderate eosinophilia (1 - 5000 eosinophils per microliter) and those that cause severe eosinophilia (more than 10,000). Although the list of parasitic infections is extensive, I will limit my presentation to those that may occur in a New England family with a cat at home. Stool examinations for worm eggs and parasites (according to the O + P x 3 rule) were not mentioned in the case presentation. I must caution because this approach involves testing three stool samples, rather than testing the same stool three times, as is often the case in practice. Infestation of Strongyloides stercoralis by a nematode, which causes significant eosinophilia and which may harbor the cat, deserves consideration. The disease is endemic in the tropics and subtropics, including the southeastern United States, but this child had not left New England during the previous year. Taking into account the manifestations from the central nervous system, neurocysticercosis (tapeworm infection after eating undercooked pork) should also be taken into account, despite the parents’ assurances that the baby did not eat raw foods. From this the following questions should arise. Was there eosinophilia during the first seizures? Was a CT scan of the skull or magnetic resonance examination performed? Fever with convulsions is not uncommon in young children; Indeed, febrile seizures are an innocuous condition that occurs in children under 5 years of age. What is the cellular composition of the cerebrospinal fluid and were there eosinophils in the cerebrospinal fluid? Most patients with cysticercosis of the central nervous system have an increased number of eosinophils in the cerebrospinal fluid. Finally, visceral larva migrans associated with toxocariasis should be considered. Toxocara canis is found in dogs and is the equivalent of T. cati in cats. Although more common among young children probably due to their propensity for pica, visceral larva migrans can also occur in older children. Its characteristic manifestations include fever, leukocytosis, persistent eosinophilia, hypergammaglobulinemia and hepatomegaly. Other manifestations include illness, anemia, cough (and in rare cases pneumonia), myocarditis, encephalitis, and even hemorrhagic rashes and seizures. The diagnosis can be difficult and may be made on the basis of presumptive evidence such as hypereosinophilia and hypergammaglobulinemia associated with elevated titers of anti-A and anti-B isohemaglutinins. Microscopic identification of larvae in a liver biopsy section is considered diagnostic, but a negative result does not exclude the diagnosis. A more definitive diagnosis can be made by demonstrating the presence of anti-Toxocar antibodies in liver biopsy sections, although the test must be performed at the Centers for Disease Control and Prevention. The very high titer of globulins in this patient is concerning and, given the possibility of a blood transfusion, I would determine his blood type. If they have a blood type other than AB, I would then ask if they have tested for anti-A or anti-B isohemagglutinin. Allergic reactions that commonly cause peripheral eosinophilia include atopic diseases such as asthma and hay fever and secondary allergic manifestations such as drug hypersensitivity reactions. Although patients with atopic diseases may have an absolute eosinophil count higher than 1000 per microliter, it is considered that in such patients with an eosinophil count above this level, systemic disease should be considered, especially in a child with additional worrisome features such as lymphadenopathy and hepatosplenomegaly. Eosinophilic syndromes include hypereosinophil syndrome, a diagnosis of exclusion when eosinophil counts above 1500 per microliter persist for more than six months and underlying parasitic, allergic, and other causes have been excluded. Skin disorders associated with eosinophilia include atopic dermatitis, urticaria, bullous pemphigoid, scabies, and erythema toxicum neonatorum, none of which are relevant to this case. Pulmonary eosinophilias include Loffler's syndrome, filarial eosinophilia, asthma, allergic bronchopulmonary aspergillosis, and Churg-Strauss vasculitis. Absence of pulmonary symptoms, despite interstitial highlighting visible on the image. does not correspond to any of these diseases. Moreover, Wuchereria bancrofti, the organism that causes tropical pulmonary eosinophilia, is endemic in the tropics including Latin America, tropical Africa, southern Asia and some islands in the South Pacific.
I would like to comment on some of the diagnoses presented in Table 3. The child does not have any of the pathognomonic features of Addison's disease—and indeed his normal blood pressure, electrolyte levels, and lack of pigmentation suggest an alternative diagnosis. Chronic hepatitis is also unlikely given normal or near-normal hepatocellular enzyme levels. Eosinophilia may be a nonspecific reaction to various malignant tumors. When associated with solid tumors, this may reflect a host mechanism against helminths. Specific tumor-derived factors that are chemotactic or eosinophilopoietic have been identified. Slungaard et al. identified one such factor in a patient with lung carcinoma and eosinophilia. A factor was cloned that is chemotactic against eosinophils, which they named “eotaxin,” and the gene responsible for the production of interferron gamma and interleukin-4 was demonstrated. Tumor cells that secrete interleukin-4 and recruit eosinophils when transplanted into mice have been shown to activate the eotaxin gene. Eosinophilic tumor infiltration has been reported to be a good prognostic indicator for several tumor types, including intestinal carcinoma and Hodgkin's disease. Interleukin-4, secreted at the site of tumor invasion, has been shown to manifest as eosinophilic infiltration of the tumor. Moreover, there is evidence that activated eosinophils may have antitumor effects. Eosinophilia is most often associated with tumors of the hematopoietic system. At the risk of oversimplification, it should be stated that a common manifestation in hematopoietic malignancies is a translocation manifested in the juxta-position of an oncogene, often a cytokine receptor and a specific functionally active gene in the involved cell, such as an immunoglobulin gene or a T-cell receptor in a lymphoid cell. This translocation may be the sole product or cause of dysregulation of genes located near the breakpoint, or both. Champlin and Gale summarized that breakpoints are associated with common forms of acute leukemia. Translocations involving the TEL gene have been reported in cases of myelodysplastic syndrome, including those progressing to chronic myelomonocytic leukemia associated with eosinophilia. Although the characteristic translocation in myelodysplastic syndrome, t(5;12)(q33;p13), links the platelet-derived growth factor receptor to the TEL gene, other translocations involving the TEL gene have the same effect. Eosinophilia is often associated with Hodgkin's disease, especially in the nodular sclerosing and mixed cell subtypes that are most often encountered in pediatric practice. Using in situ hybridization, some researchers have identified increased levels of interleukin-5 messenger DNA in Reed-Sternberg cells. Although the history of fever and lymphadenopathy in this patient is suggestive of Hodgkin's disease, the presence of both neutropenia and eosinophilia, as well as the normal erythrocyte sedimentation rate and distribution of lymphadenopathy, are unusual for this disease. If Hodgkin's disease tends to spread to adjacent lymph node groups, then cervical lymphadenopathy and hepatosplenomegaly without widespread mediastinal disease would be unusual. Moreover, hepatomegaly is not a typical feature of Hodgkin's disease and the disease itself is unusual in children as young as seven years of age. Other types of lymphoma that have been associated with eosinophysia include lymphoblastic lymphoma, as with myeloid hyperplasia, or myeloid leukemia (a biphenotypic malignancy) associated with a translocation between chromosomes 8 and 13. Patients with such disorders usually have isolated lymphadenopathy and sometimes splenomegaly or systemic (B) symptoms , but not hepatomegaly. The youngest patient in the latest case series was 18 years old. Regarding the age of the patient in question, the most predominant type of cancer for him would be leukemia. Acute myelomonocytic leukemia (M4) is associated with inversions of chromosome 16 and an increase in the number of eosinophils in the bone marrow, which usually exceeds those in the peripheral blood. Other types of leukemia, such as acute lymphoblastic leukemia with a translocation between chromosomes 5 and 14, are associated with severe eosinophilia in both adults and children. The presence of fever and lymphadenopathy is quite common, and patients with severe eosinophilia often have cardiovascular problems. In at least one case there was tissue invasion by eosinophils with cardiac manifestations consistent with Loffler endocarditis. In this case, a 21-year-old man with Loffler's endocarditis had deep vein thrombosis, indicating a thrombotic diathesis in this form of leukemia. Although eosinophilia itself does not necessarily pose a risk to the patient, tissue invasion can manifest as damage, and in the case mentioned above, myocardial invasion may have contributed to the rapid loss of myocardial function during induction therapy. Grimaldi and Meeker reported a translocation between chromosomes 5 and 14 that manifested itself in the juxta position of the interleukin-3 gene and the immunoglobulin heavy chain gene in a patient with severe lymphatic leukemia of the B-cell lineage and severe eosinophilia. Meeker et al. further showed that both this patient and a second patient had an activated interleukin-3 gene, manifested by excessive production of interleukin-3, which correlated with disease activity. Finally, the case discussed closely resembles a case report in which chorea, eosinophilia, and lupus anticoagulant developed in a 5-year-old girl with acute lymphocytic leukemia. She had fever, sore throat, and myalgia; Subsequently, “non-rhythmic involuntary twitching movements of her limbs, twitching of the face and speech with swallowing of sounds” appeared. Eosinophils accounted for 59% of the cells in the peripheral blood differential, and laboratory studies revealed a coagulopathy with a prothrombin time of 14 seconds (reference value 13), which was not corrected by the addition of transfused plasma; partial thromboplastin time was normal. Lupus coagulants are usually associated with prolonged prothrombin time. Although the patient did not have bleeding or clotting problems, the combination of prolonged prothrombin time and lupus anticoagulant was associated with a bleeding diathesis, in contrast to the typical lupus anticoagulant, which is associated with thrombotic diathesis. Whether the patient described by Troxell et al had lupus anticoagulant can not be said with certainty based on the article. Were this patient's central nervous system symptoms and dysgammaglobulinemia indirect effects of eosinophilia? Could eosinophilic neurotoxin in granules specifically contribute to central nervous system symptoms? Are lupus anticoagulants the result of aberrant immunoglobin production associated with a translocation of the heavy chain immunoglobulin gene? That such questions can be asked at all shows that techniques developed for basic research can be applied to clinically relevant questions. In summary, although toxocariasis (visceral larva migrans) and hypersensitivity to one of the anticonvulsant drugs taken by the boy remain diagnostic possibilities, I believe that this is an unusual presentation of acute lymphocytic leukemia as a result of a specific chromosomal translocation manifested by eosinophilia and symptoms in this boy .
Dr Robert E. Scully: Dr. Ebb, what was your impression before the diagnostic procedures were performed? Dr. David H. Ebb: We thought about the possibility of a hematopoietic malignancy due to the presence of generalized lymphadenopathy, organomegaly and neutropenia. We did a bone marrow biopsy.
Clinical diagnosis Acute leukemia
DR.JED B. GORLIN'S DIAGNOSIS Acute lymphocytic leukemia associated with a specific translocation, manifested by eosinophilia
PATHOLOGICAL DISCUSSION Dr. Judith A. Ferry: Examination of peripheral blood smears revealed marked leukocytosis, but only 5% of the white cells were neutrophils, more than half were lymphocytes, and eosinophils were abundant. Some had a somewhat dilated oval or irregular nucleus and scanty to moderate amounts of pale blue cytoplasm. Cytometric study showed that the majority of the cells in the lymphocytic light-scatter gate (89%) were CD3+ T cells; these cells also expressed CD5 and CD7, consistent with normal T cells. There was an inversion of the CD4:CD8 ratio, with 52% CD8+ (cytotoxic or suppressor) T cells and only 37% CD4+ (helper) T cells. The rest of the mononuclear cells were B cells that secreted polytypic immunoglobulin. These morphological types and immunophenotype were most consistent with a reactive process. Bone marrow examination revealed approximately 80 percent cellularity, which is normal or slightly increased for a seven-year-old child. Erythroid series showed almost complete maturation and mature granulocytes were infrequent. Cells of the neutrophil line were represented in reduced quantities; the majority of myeloid forms were eosinophils and their precursors. The number of megakaryocytes was slightly increased. In addition, there was a single, well-formed granuloma containing multinuclear giant cells. We did not detect parasites or any other microorganisms using conventional staining methods or special staining for mycobacteria and fungi. We found no evidence of lymphoma or leukemia. We interpreted these changes as characteristic of a reactive process, probably a hypersensitivity reaction. However, we were unable to determine the specific cause of these changes.
Dr Ebb: After the bone marrow examination, the boy's most threatening manifestations of the disease continued to improve. The rash disappeared, and severe organomegaly and generalized lymphadenopathy rapidly decreased. Subsequent chest films showed resolution of the interstitial infiltrates. Thus, there were no clinical or laboratory findings to support the diagnosis of leukemia, lymphoma, or infection. We found several case reports in the literature concerning children and adults treated with carbamazepine that had an almost identical constellation of findings. All of these patients presented within one week to three months of starting anticoncussive therapy and most improved within two to six weeks of stopping treatment. Given the possibility of T. canis infestation, serological tests for toxocariasis were performed, which were negative. We conclude that this child developed a carbamazepine hypersensitivity syndrome akin to pseudolymphoma syndrome after phenytoin therapy, which has been more extensively documented. Pseudolymphoma syndrome was characterized by fever, erythematous rash, severe lymphadenopathy, and, less commonly, organomegaly. Only about 200 cases of pseudolymphoma have been reported as a complication of phenytoin therapy, and fewer than 24 cases have occurred following administration of carbamazepine.
Dr. Satya N. Cavarasana: What was the cause of the patient's fever and seizures?
Dr. Ebb: We assume that this was a primary neurological disorder, although we do not know the full extent of the treatment performed at the other hospital. We found no evidence of an infectious cause. We performed a large number of viral serological tests, which were negative.
Dr. Mark S. Pasternack: We often see children who have been febrile for some time before their presentation and it is very difficult to make an accurate diagnosis in retrospect. In this case, the working diagnosis was febrile seizures, and the patient's course of illness was consistent with this diagnosis.
ANATOMICAL DIAGNOSIS Hypersensitivity reaction to carbamazepine.
Causes of a low number of eosinophils in the blood
A decrease in the number of eosinophils below 0.02*109/l is called eosinopenia. There are several possible reasons:
- Taking glucocorticoids and steroids. These are hormonal drugs that help reduce the number of leukocytes (including eosinophils) in the blood due to their destruction. At the same time, eosinopenia is not a strong enough reason to discontinue a course of glucocorticoids, since in itself it does not pose a threat to health, while the therapeutic effect of these drugs for allergic reactions or autoimmune diseases fully justifies their use.
- Nervous tension and stress. During times of severe mental stress, depression and emotional turmoil, the level of cortisol, which is called the stress hormone, increases in the blood. It is cortisol that destroys eosinophils.
- Allergic reactions. The level of eosinophils in allergies is a rather paradoxical issue. With moderate hypersensitivity reactions, eosinophilia is observed, but with severe allergies, the level of eosinophils, on the contrary, decreases.
- Infectious diseases. Eosinopenia is characteristic of diseases of a viral and bacterial nature, which include coronavirus infection. A decrease in the number of eosinophils is also observed in purulent-septic processes (abscesses and phlegmon).
- Endocrine diseases. As we already know, an increase in the level of cortisol in the blood entails a decrease in the number of eosinophils. Cortisol is produced in the adrenal glands, so adrenal diseases (for example, Cushing's syndrome) cause eosinopenia.
- Bone marrow diseases. Since eosinophils are formed in the bone marrow, any associated pathologies and injuries cause eosinopenia.
- A decrease in the level of eosinophils in the blood can also be observed in the first days after a heart attack, with appendicitis, sepsis, acromegaly, lupus erythematosus, burns and injuries.
Figure 2. Eosinopenia (low eosinophil count). Dr Graham Beards / Wikipedia (CC BY-SA 3.0)
Decreased eosinophil levels
If the analysis showed a reduction in eosinophils to a level below 1%, we are talking about problems with the production of new cells. The condition itself goes away if it is caused by a massive movement of leukocytes to the site of infection, however, a prolonged lack of defenders may indicate the body’s inability to replenish their supply. Diseases and environmental factors lead to this:
- stress, lack of sleep, physical fatigue - their constant impact weakens the body;
- injuries, including from burns and operations, radiation during tumor therapy;
- shock from excessive concentration of toxins released by microorganisms, poisoning with heavy metal salts;
- taking corticosteroids;
- serious bacterial infections such as typhoid fever;
- inflammation of the peritoneum, appendicitis, blood poisoning;
- bone marrow damage;
- anemia due to lack of vitamin B12.
For infections, once eosinophils return to normal, one can judge the effectiveness of the chosen drug. Eosinophils may be reduced in a woman during pregnancy and the first two weeks after childbirth; the latter turn out to be serious stress for the body. Eosinopenia in such cases is considered normal, just like its development after surgery or from taking certain medications.
Consequences of deviation from the norm
A change in the normal level of eosinophils in the blood is not a criterion by which one can get an idea of possible pathological changes in the body. Simply put, the level of eosinophils in the blood itself means little - you need to pay attention to the disease that caused its change. Therefore, the consequences can be very diverse - from completely insignificant (as in the case of physical activity) to deadly (for example, in the case of oncology).
Eosinophilia itself, in rare cases, can lead to damage to tissues in which the greatest accumulation of eosinophils is observed. The mechanism of such damage has not been fully studied to date, but it has been established that eosinophils exhibit the most severe damaging effect in conditions such as eosinophilic fibroplastic endocarditis and idiopathic hypereosinophilic syndrome. The nature of the damage directly depends on the duration of eosinophilia and the severity of eosinophilic tissue infiltration.
What are eosinophils and what do they do in the body?
Eosinophils are blood cells that belong to the group of leukocytes. Leukocytes in the blood are a diverse group of cells that differ in their structure and functions. The main function of these cells is to protect the body.
Eosinophils are part of the immune system. They are responsible for protecting the human body from foreign agents: bacteria, viruses, allergens.
Eosinophils easily penetrate the vascular bed. This allows them to easily move and reach the desired place when a foreign agent enters the body. These cells are able to absorb and destroy it. True, they are able to do this only with relatively small particles.
Eosinophils have a high cytotoxic effect - their main purpose is to fight parasites. It is involved in the formation of antiparasitic immunity.
This type of leukocyte is able to absorb histamines, which play an important role in the formation of an allergic reaction. This allows not only to provoke the activation of the immune system, but also to suppress it due to excessive production of substances that can cause harm to the body.
How to reduce the number of eosinophils in the blood
Eosinophilia is not an independent nosological entity, but only a consequence of a particular disease. Therefore, it cannot be treated in isolation - first of all, it is important to eliminate the cause of its occurrence, that is, the disease that caused the change in the leukocyte formula.
Possible treatment options:
- Desensitizing therapy. For allergies, antihistamines are used to reduce hypersensitivity reactions. Some of them may cause mild drowsiness (for example, chloropyramine), but newer generation drugs such as cetirizine, levocetirizine, desloratadine and rupatadine do not have this side effect and have a mild anti-inflammatory effect.
- Antibacterial therapy - for infectious diseases, antibiotics are prescribed (amoxicillin, ceftriaxone, azithromycin, erythromycin, etc.). The choice of antibacterial drug depends on the pathogen and its sensitivity to a specific group of antibiotics.
- Anti-inflammatory therapy. An increase in the level of leukocytes (including eosinophils) is observed during inflammatory processes. When they are severe, glucocorticosteroids (prednisolone) are used.
- Chemotherapy. This treatment method is aimed at eliminating malignant tumors. For this purpose, cytostatics and antimetabolites are used.
- Hormonal therapy. For multisystem diseases accompanied by immunodeficiency (for example, Jobe's syndrome), the use of steroid drugs and interferon gamma is indicated. Treatment is supplemented with antibiotics, calcineurin inhibitors, H1-histamine blockers, and antifungal drugs.
- Antihelminthic therapy. To combat helminthic infestations, drugs such as albendazole, levamisole, bephenia hydroxynaphthoate, piperazine, tetrachlorethylene, and mebendazole are prescribed. The choice of medication depends on the type of parasite and the stage of infestation. Additionally, antibiotics, enterosorbents, enzymes, probiotics, and glucocorticoids are prescribed.
Additionally, the following measures can be taken:
- Normalize your lifestyle. It is important to avoid frequent drinking of alcohol and give up cigarettes (or at least significantly limit the number of them).
- Avoid chronic intoxication. In people working in hazardous industries or living in environmentally unfavorable regions, the number of eosinophils in the blood increases as a result of constant chemical intoxication.
- Maintain a healthy diet. You should not overuse spicy, smoked, canned and fatty foods. To increase the level of eosinophils, you should limit the amount of meat, poultry and fish in your diet (consume mainly low-fat varieties). The menu should include yogurt, cheeses, vegetables, fruits, beans, bran and whole grain bread.
Giving up bad habits will help normalize the level of eosinophils. Photo: vgstockstudio / freepik.com
How to increase the number of eosinophils in the blood
A decrease in the level of eosinophils in the blood is a sign of weakened immunity. As in the case of eosinophilia, the primary pathology should be identified and eliminated, as well as lifestyle adjustments: minimize bad habits, ensure an adequate level of physical activity, and also take care of a normal daily routine (it is important to sleep at least 8 hours a day) .
The normalization of the leukocyte formula is facilitated by the consumption of vitamins B12, C, D. They can be obtained from food (meat, fish, cottage cheese, rose hips, currants, garlic), or from pharmacy multivitamins. It is advisable to exclude foods with a high allergenic potential: milk, soy, wheat, eggs, seafood, peanuts.
When treating diseases that result in eosinopenia, the same groups of drugs are often used as in the case of eosinophilia. For example, antibiotics are prescribed for infectious diseases, as well as diffuse and localized purulent-inflammatory processes (cellulitis and abscess). As mentioned earlier, allergies can provoke not only an increase, but also a decrease in the number of eosinophils in the blood, so antihistamines can also be used in the treatment of eosinopenia.
Importance of eosinophils for diagnosis
The level of eosinophils is one of the first steps in assessing the condition of the body, and its norm is the same for both men and women. Being one of the important participants in the immune system, these cells migrate to the allergen or invader, and in return the body tries to increase the production of new eosinophils. An elevated blood level indicates allergies, helminthiases and associated lesions of the gastrointestinal tract and lungs, and less often is a sign of serious immunodeficiencies or tumors. Eosinopenia often becomes noticeable as a result of the body’s too active efforts to eradicate the problem and the insufficient rate of replenishment of the ranks of leukocytes.
One way to detect an allergy or related process is to test for eosinophilic cationic protein. Blood for it is taken from a vein, and in general the method is considered more accurate than searching for representatives of leukocytes or immunoglobulin E. This protein itself helps eosinophils attack pathogens or stimulate the immune system, therefore, during illness, its content increases along with the cells themselves. Sometimes a nasal swab is taken from the patient for eosinophils: this also helps to identify the nature of the disease - for example, rhinitis.