What is pathology?
Blood leukemia in children is a malignant disease of leukocytes, i.e. white blood cells. The problem is that with this pathology, the bone marrow produces abnormal (mutated) cells that are unable to perform their protective functions. Instead, diseased white blood cells divide uncontrollably, preventing the body from producing red blood cells (red blood cells) and platelets (nuclear-free, flat cells responsible for blood clotting).
Based on the duration of the disease, two forms are described:
- acute (less than two years);
- chronic (over two years).
In the children's body, the first type occurs predominantly; it accounts for 97% of cases.
According to morphological type, they are distinguished:
- lymphoblastic leukemia in children (in this case, young, immature leukocytes – lymphoblasts) undergo mutations;
- non-lymphoblastic.
The second type includes a malignant lesion of the myeloid blood line (it is also called acute myeloblastic leukemia in children).
The acute form is characterized by dynamic development; as a result of this disease, anemia appears, the immune system is weakened, internal hemorrhages occur, and increased bleeding is observed. All this is accompanied by sensitivity to infections (children get sick very often).
On a note
Achievements in domestic oncohematology, primarily in children, became possible thanks to the state’s attention to this branch of medicine.
41% of the funds allocated to finance the state program “7 nosologies” (which is $1.16 billion) are allocated to the treatment of patients with hematological malignancies (malignant blood diseases, which also include childhood leukemia).
In Russia, unrelated bone marrow donation programs are just beginning - such transplants began to be performed only 10 years ago. On a national scale, there are negligible numbers of them - no more than 70–80 per year. In total, 13 clinics in the country are licensed to perform transplantation, and there are 70–75 board-certified hematologists, oncologists, and transfusiologists who can perform the procedure. One of the largest transplant departments is the Scientific and Clinical Center for Pediatric Hematology, Oncology and Immunology named after Dmitry Rogachev, which opened in 2011 in Moscow.
Why does this disease develop?
The exact causes of leukemia in children have not been established to date; only a number of dangerous factors that can lead to the disease have been identified.
First of all, it is called a genetic factor. The disease itself is not transmitted, we are talking about the tendency of cells to mutate. It has been noticed that those who have close relatives who suffered the same pathology get sick more often. It is also worth noting the connection with some congenital diseases (for example, with Down syndrome, the risk of developing a malignant process in the blood is 15 times higher than in healthy babies).
Radiation radiation, some chemical factors, as well as endogenous problems (immunodeficiency, hormonal imbalance) can cause the development and signs of leukemia in children.
Causes
The causes of oncological blood diseases have not been precisely established. It could be:
- genetic failure;
- abnormal development of blood cells;
- exposure to radiation;
- hereditary factor;
- poor environmental stop;
- consumption of carcinogens, etc.
Even a medical luminary is unlikely to be able to say exactly why a child, who does not yet have negative habits and does not eat harmful foods, develop an illness.
Main symptoms indicating pathology
Leukemia does not manifest itself in children with characteristic symptoms; this disease has only general signs that may indicate the development of any disease. Therefore, this diagnosis is often detected during an examination with suspicion of another illness.
At the same time, you can suspect the first signs of leukemia in children if you pay attention to such deviations as:
- increased fatigue (which is unusual in childhood, when, on the contrary, hyperactivity should be observed);
- shortness of breath during games;
- sleep disorders;
- poor appetite;
- pallor of the skin (often they have an earthy tint);
- high tendency to bruise;
- frequent bleeding (nose, gum);
- headache;
- unreasonably rising temperature.
The most striking symptoms of acute leukemia in children are long-term bleeding wounds after falls or cuts (this indicates poor clotting) and frequent illnesses.
Failure in the immune system
Is it possible to predict the risk of developing leukemia? Unfortunately no. “99% of leukemias are completely random events,” says Deputy General Director for Scientific Work of the Federal Research Center for Pediatric Hematology, Oncology and Immunology named after Dmitry Rogachev, Director of the Institute of Hematology, Immunology and Cell Technologies (IGICT), Doctor of Medical Sciences, Professor Alexey Maschan . — In children, the most rapidly developing system is the immune system, and a failure in its functioning in some people leads to the development of leukemia. Every year, 4 cases of acute leukemia are registered per 100 thousand children.”
Where to go Bone marrow transplantations for children and adolescents are carried out in 13 Russian medical centers. The leading ones are located in Moscow - Federal Scientific Center for Children's and Orthopedics Orthopedics named after. Dmitry Rogachev, Russian Children's Clinical Hospital, Cancer Center named after. N. N. Blokhina. In St. Petersburg - St. Petersburg State Medical University named after. Academician I.P. Pavlov, Institute of Pediatric Hematology and Transplantology named after Raisa Gorbacheva. There are centers in Yekaterinburg and Nizhny Novgorod.
Experts recommend paying attention to the following symptoms and changes in the child’s well-being:
- the unreasonable appearance of bruises, small hemorrhagic rash - not because the child hit himself, but just like that;
- pallor, increased abdominal size;
- the appearance of strange formations on the body, enlarged lymph nodes;
- changes in blood tests;
- There may be various pains - headaches, in the stomach, but this is an optional symptom.
The first person parents should contact for advice is the local pediatrician; he will decide whether the child needs a consultation with a hematologist.
“If the fears are not unfounded, the child is transferred to the regional children's clinical hospital, to hematologists. Regional hospitals decide whether they can cope with this disease on their own: whether they have the necessary equipment and personnel,” says Elena Skorobogatova, head of the bone marrow transplantation department of the Russian Children’s Clinical Hospital of the Russian Ministry of Health, Doctor of Medical Sciences . “If it can’t be dealt with locally, the region turns to one of the federal clinics where there is a bone marrow transplant department. My advice: if your child is diagnosed with acute leukemia, do not go to private clinics, use the public network. Don't waste your time and money! "
How is this pathology diagnosed?
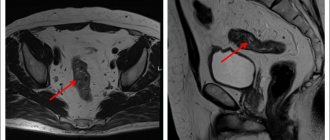
After the initial examination, the first thing the doctor will prescribe is a blood test for leukemia in children (this includes extensive research and biochemistry). Laboratory testing will show the presence of anemia, thrombocytopenia, and ESR will be increased. The most characteristic blood parameters for leukemia in children are such an anomaly as “leukemic failure”. Its essence is that between immature leukocytes and mature ones there are no obligatory transitional forms (young, segmented).
The pediatric diagnostic program must include:
- sternal puncture;
- bone marrow biopsy;
- trephine biopsy.
In addition, an examination by a pediatric neurologist or ophthalmologist is necessary. Additional are ultrasound of the lymph nodes, and, if necessary, of the liver, salivary glands and other organs (the need is determined by the doctor based on the results of the examination).
Hope for salvation
“The goal of any pediatric hematologist-oncologist is to cure all of his patients,” says Alexey Maschan, “but we cannot yet cure 10–20% of children with leukemia. Their treatment requires fundamentally new approaches, and they are no longer in the scope of conventional chemotherapy, no matter how intense it may be. Doctors have high hopes for biotechnologies and the development of a new area – immuno-oncology.”
Time for mercy. What can everyone do for the children from the cancer center?
More details
The first research in the field of creating immuno-oncological drugs began about 15 years ago in the USA and European countries. Today, immunotherapy for leukemia, including in children, is successfully used in European and American clinics when chemotherapy is ineffective. With the new treatment method, 70% of hopeless patients achieve remission. The drugs have not yet been registered, but are already available in Russia. Several of Rogachevsky’s patients are undergoing therapy under the individual access program,” sums up Alexey Maschan.
Article on the topic
Valery Savchenko: “Thanks to progress in chemotherapy, thousands of lives have been saved”
What treatment methods are used
The main method of treating leukemia in children is complex chemotherapy. It consists of a combination of several specific anticancer drugs and glucocorticoid hormones in high doses. After the course, immunotherapy (interferon or other drugs) is mandatory.
Particularly important in treatment is a step-by-step approach, which is aimed at:
- achieve stable remission;
- secure it;
- carry out maintenance therapy;
- prevent possible complications.
In complex cases, stem cell transplantation, bone marrow transplantation from a donor, and platelet and red blood cell transfusions may be necessary.
Price issue
The cost of one bone marrow transplantation operation exceeds 2 million rubles (according to the Program of State Guarantees of Free Medical Care to Citizens for 2015 and for the planning period of 2021 and 2021).
Article on the topic
Rescue from cancer: Spain is one of the best places for treatment of childhood oncology
“Since 2015, the state has been allocating 2 million 300 thousand rubles for each patient for transplantation for the entire treatment; this amount allows us to close many positions that were previously paid for by charitable foundations,” says Elena Skorobogatova. “But still, the contribution of philanthropists is significant, it amounts to 20 percent or more in the treatment of our patients. Funds resolve issues not only of providing medications and consumables, but in some cases also pay for the search for a donor, transportation costs for the delivery of donor bone marrow, and much more. Each center works with its own funds, we work with the Gift of Life foundation.
About relapses and prognosis after treatment
As a rule, a relapse of this particular disease, if it exists, manifests itself directly during the course of treatment or immediately after its completion. After remission has been achieved and its consolidation (consolidation) has been carried out, after five years relapses are an extremely rare occurrence. After seven years, we can safely talk about a complete recovery.
Modern treatment methods suggest a favorable prognosis for acute lymphoblastic leukemia in children in 60-80% of cases. The indicator is influenced by an adequate therapy program (including the capabilities of a specialized clinic) and the general condition of the body.
Acute myeloid leukemia in children
Leukemias occupy a leading place in the structure of childhood cancers and account for 30-40% of all malignant diseases, of which acute lymphoblastic leukemia (ALL) accounts for 80%, and acute myeloid leukemia (AML) for 15-17%. The frequency of acute leukemia (AL) in children under 15 years of age is 4.1+0.4 cases per 100 thousand children with a boy/girl ratio of 1.3 (aged 2 to 5 years).While significant advances in treatment have been achieved in children with ALL, the results of treatment for AML remain unsatisfactory. In this regard, the problem of diagnosis and treatment of AML in children is relevant.
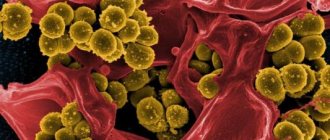
AML is a heterogeneous group of diseases. The basis for dividing it into various options is the morphological identification of leukemic cells, which, in addition to cytological data, uses cytochemical indicators.
In 1976, the French-American-British (FAB) classification was adopted, which distinguishes several variants among AML: M0 - acute undifferentiated leukemia, M1 - acute myeloid leukemia without signs of maturation, M2 - acute myeloid leukemia with signs of maturation, M3 - acute promyelocytic leukemia, M4 - acute myelomonoblastic leukemia, M5 - acute monoblastic leukemia, M6 - acute erythrocyte leukemia, M7 - acute megakaryocytic leukemia.
Diagnostics
The diagnosis of AML is made in more than 30% of cases when blasts are detected in the bone marrow. Blasts must have morphological and cytochemical characteristics of one of the FAB variants of AML.
Cytochemical data aimed at diagnosing variants of the disease are a positive reaction to myeloperoxidase, with Sudan black B and nonspecific esterase inhibited by sodium fluoride. Moreover, the totality of these indicators differs in different types of AML. Thus, the presence of a positive reaction to myeloperoxidase is typical for variants M1, M2, M3 and M4, and nonspecific esterase, inhibited by sodium fluoride, is specific for variants M4 and M5.
A significant addition to the diagnosis of AML are immunophenotypic studies that clarify the standard morphological diagnosis and variants of AML.
The most common and widely used to confirm the non-lymphoid nature of leukemia are CD13 and CD33 antigens; CD65 is used somewhat less frequently. Evaluation of these three markers allows us to confirm the myeloid nature of tumor cells in 98% of cases of AML in children.
Chromosomal analysis is necessary to predict the outcome of AML treatment. In approximately 75% of children with AML, one or another chromosomal aberration can be identified, among which there are anomalies that are characteristic only of certain variants of AML. Thus, t(8;21) is associated with the M2 variant, t(15;17) - with the M3 variant, inv(16) - with the M4 variant with eosinophilia. The 11q23 anomaly occurs in the M4 and M5 variants and t(1;22) in the M7 variant. Using molecular biological diagnostic methods - polymerase chain reaction (PCR) and FISH (fluorescent in situ hybridization) - it is possible to determine a chromosomal aberration that was not detected by a standard cytogenetic study. This is especially important for choosing a specific type of treatment if the M3 variant is confirmed. In addition, thanks to the introduction of molecular diagnostic methods for AML, it is now possible to establish not only clinical and hematological, but also molecular remission in patients, followed by monitoring of minimal residual disease and determination of molecular relapse.
Clinic
The clinical picture of AML is quite well known and is manifested by the following syndromes: anemic, hemorrhagic and toxic, which are characterized by pallor of the skin, severe weakness, dizziness, decreased appetite, increased fatigue, fever without manifestations of catarrhal phenomena.
The lymph nodes in most patients are small, painless, and not fused to the skin or to each other. In rare cases, enlarged lymph nodes ranging in size from 2.5 to 5 cm are observed with the formation of conglomerates in the cervical-supraclavicular region. Changes in the osteoarticular system in some cases are manifested by pronounced ossalgia in the lower extremities and in the spinal column, which is accompanied by disturbances in movements and gait. Radiographs of the skeletal system show destructive changes of various locations, periosteal reactions, and symptoms of osteoporosis. Most children experience a slight enlargement of the liver and spleen (protrude 2-3 cm from under the edge of the costal arch).
Extramedullary tumor lesions often manifest as gingivitis and exophthalmos, including bilateral ones; in rare cases, there is tumor infiltration of soft tissues, hypertrophy of the palatine tonsils, damage to the nasopharynx and facial nerve, as well as leukemides on the skin.
Extramedullary localizations of AML are united by the term “granulocytic (myeloblastic) sarcoma,” which includes classical chloroma and non-pigmented tumors.
According to autopsy data, granulocytic (myeloblastic) sarcoma is diagnosed in 3-8% of cases in patients with AML. It may precede or be combined with signs of AML, characterized by blastic infiltration of the bone marrow and the presence of blasts in the peripheral blood, and may also be observed during disease relapse. The most common localization of tumor growth is the orbit (orbital tissue and internal structures of the skull are affected). Blast cells are often represented by the M2 type, having the t(8;21) translocation. A number of authors indicate a worse prognosis in these patients than in typical AML.
Prognosis factors in patients with AML are less studied than in patients with ALL. A large number of single- and multifactorial studies have been conducted, with the help of which it became possible to determine favorable and unfavorable signs of the disease in order to prescribe rational treatment. The factors on which the prognosis of AML in children depends are divided into clinical and laboratory. Clinical factors include age, gender, medical history, size of parenchymal organs, severity of hemorrhagic syndrome, initial damage to the central nervous system, time of remission, number of chemotherapy courses. Among the laboratory prognostic factors are the sensitivity of blast cells to chemotherapy in vitro, the number of leukocytes in a peripheral blood test, the FAB variant of AML, fibrinogen level, lactate dehydrogenase level, and the presence of Auer rods in blasts.
The prognosis for AML depends on the FAB morphological variant, genetic testing data and the immunophenotype of blast cells. Thus, the most favorable group consists of patients with morphological variants M1, M2 and t(8;21), t(9;11), M3 and t(15;17) or M4 and inv(16). The group unfavorable for prognosis includes patients with variants M4 without inv(16), M5, M6 and M7, as well as patients whose tumor cell karyotype study revealed the following chromosomal abnormalities: t(9;22), t(6;11) ), t(10;11), del5q-, del7q-, monosomy -5, -7. In addition, our studies were able to prove that the prognosis of AML is adversely affected by the expression of erythroite and B-lineage antigens on the surface of blasts.
Treatment
Treatment of patients with AML is based on the principle of maximum destruction of the leukemic cell clone. The main method of treating the disease is polychemotherapy. Currently, there are several directions in the treatment of AML, including both the use of new cytostatics and increasing doses of already known chemotherapy drugs. In addition to these already sufficiently studied and traditional methods of influencing the leukemic process, there are experimental approaches using natural biologically active drugs that in one way or another affect the process of hematopoiesis (all germ factors, interleukins). Along with cytostatic agents, they are also trying to use drugs that have a powerful modeling effect on the immune system (cyclosporine, anti-leukocyte immunoglobulin). The use of germ factors in AML is currently being debated due to evidence that they can promote proliferation of the tumor cell clone. Currently, some researchers are proving the possibility of using colony-stimulating factors (granocyte, etc.) in patients with AML.
In recent years, bone marrow transplantation (BMT) has been widely introduced into treatment programs for acute nonlymphoblastic leukemia (ANLL), both allogeneic (in the presence of an HLA-compatible donor) and autologous transplantation of peripheral stem cells or bone marrow.
Modern treatment programs for AML consist of different stages - induction, consolidation, intensification and maintenance treatment during remission (usually lasting at least 2 years). At the same time, prevention of neuroleukemia is carried out using endolumbar administration of chemotherapy drugs (cytosine arabinoside). In recent years, preventive remote gamma therapy on the brain region has become more widely used.
When conducting inductive and consolidating courses of chemotherapy, maximum intensification is necessary, which leads to the fastest achievement of complete remissions. The consequence of such therapy is bone marrow aplasia, during which the likelihood of infectious and hemorrhagic complications increases sharply, and therefore patients require complex accompanying treatment, including replacement, antibacterial and detoxification therapy.
The main drugs included in the polychemotherapy programs used are combinations of cytosine arabinoside and anthracycline antibiotics. Until the 80s, the DAT and “7+3” schemes were used. Since the mid-80s, etoposide began to be introduced into treatment programs, which led to a higher number of complete remissions and an increase in relapse-free survival of patients. The most effective treatment programs that include etoposide are the BFM-83 and BFM-87 programs. Remission induction consists of cytosine arabinoside, daunorubicin and etoposide, and consolidation consists of vincristine, daunorubicin, cytosine arabinoside, 6-thioguanine, prednisolone, cyclophosphamide, followed by maintenance therapy (cytosine arabinoside and 6-thioguanine until 104 weeks from the onset of remission). According to the BFM-87 study, the five-year event-free survival rate was 47%.
One of the ways to intensify chemotherapy and achieve longer remissions is to increase the doses of cytosine arabinoside (up to 3000 mg/m2 every 12 hours).
Recently, studies have appeared on the use of mitoxantrone for the treatment of AML in children, especially in patients with a poor prognosis (M5, M7, M6, M4 without eosinophilia and inv(16), M2 with leukocytosis more than 50x109/l) and with relapse of the disease. The most effective therapy was a combination of high doses of cytosar, mitoxantrone, and etoposide. This therapy leads to severe myelodepression, without which it is impossible to achieve complete remission in AML, especially in patients with a poor prognosis and relapses of the disease. The use of mitoxantrone (12 mg/m2) in patients with a poor prognosis did not lead to an increase in the number of complications while achieving a greater number of complete remissions in patients with treatment-resistant forms of ALLL.
Currently available data indicate that, on the one hand, the intensification of chemotherapy has significantly increased the effectiveness of treatment, on the other hand, the number of adverse reactions and complications has increased, in some cases causing the death of patients.
The treatment direction associated with the use of differentiating agents, such as retinoic acid isomers, has achieved the greatest results in the treatment of acute promyelocytic leukemia (M3). In case of chromosomal aberration t(15;17), corresponding to M3 FAB, the breakpoint of chromosome 17 involves the gene corresponding to the nuclear receptor for alpharetinic acid, which makes it possible to restore the affected gene and promotes apoptosis of tumor cells while reducing the number of episodes of hemorrhagic complications.
The experience of the last 20 years has shown that the improvement of accompanying treatment technology, mainly methods of controlling infections in a patient with induced granulocytopenia, and the emergence of methods for obtaining thromboconcentrate have made it possible to achieve 80% of complete remissions, despite a significant tightening of polychemotherapy regimens. That is why the main directions of modern protocols are various options for intensifying chemotherapy, which can be carried out using a number of options: introducing additional cytostatic agents into already known protocols; the use of new cytotoxic drugs as an alternative to those studied, for example, more active second-generation anthracyclines (idarubicin and mitoxantrone); cyclic intensive chemotherapy for 1.5-2 years after achieving remission; modification of standard chemotherapy programs based on the kinetic parameters of blast cells during therapy and the characteristic features of hematopoietic restoration after cytostatic exposure; the use of germ factors to accelerate recovery from post-chemotherapy aplasia; early use of autologous and allogeneic bone marrow transplantation. The principle of early intensification is currently the main one in the treatment of AML and, according to many studies, has an advantage over the standard one. It makes it possible to reduce the number of patients with resistant forms of AML by increasing the power of cytostatic effects in the first, early stages of therapy.
When analyzing data from different research groups, it becomes obvious that in approximately half of patients who achieve remission, AML relapses. Moreover, 75% of relapses are detected within the first year from the start of therapy, another 15% - during the second year, and 10% of relapses are recorded later than 2 years from the start of therapy. In this regard, the goal of post-remission therapy is to eradicate the residual leukemic clone. Post-remission therapy is generally classified as follows: 1) consolidation therapy—post-remission therapy similar in intensity to induction, using multiple, non-cross-resistant drugs; 2) intensification therapy: post-remission therapy, the purpose of which is to overcome drug resistance (usually these are drugs previously used in induction); 3) maintenance therapy: significantly less intensive post-remission therapy (in some studies up to 3 years).
It has now been proven that the results of treatment of patients with AML who received all stages of polychemotherapy (induction of remission and post-remission therapy) in full are significantly higher.
In most AML treatment protocols, the most common supportive therapy recommended by the BFM group, which consists of daily 6-thioguanine at a dose of 40 mg/m2 in combination with subcutaneous cytosine arabinoside (40 mg/m2 x 4) every 4 weeks. It is carried out for up to 18 months from the start of treatment. However, as the intensity of post-remission therapy increases, the duration of maintenance treatment decreases.
Prevention of neuroleukemia consists of endolumbar administration of cytosine arabinoside, methotrexate, or a combination of these drugs with hydrocortisone, with or without cranial irradiation. A number of authors consider cranial irradiation of patients with AML to be a necessary component of therapy, others are of the opinion that cranial irradiation is necessary only for children with primary damage to the nervous system, as well as for patients with the M4 variant, with chromosomal abnormalities inv (16). Preference for cranial irradiation is expressed by researchers from the BFM group, who showed a decrease in the incidence of not only neuroleukemia, but also bone marrow relapses when it is performed.
The question of the role of allogeneic BMT (allo-BMT) in children with AML in the first clinical and hematological remission is currently actively debated. Although allo-BMT is an effective therapy for AML, issues of donor availability and process toxicity limit its use. The key issue in the use of allo-BMT in children with AML in first remission is to identify the relationship between the anti-leukemic effect, increasing the survival rate of patients with a further acceptable quality of life.
Currently, candidates for allo-BMT are high-risk patients who have an HLA-identical bone marrow donor. The issue of autologous BMT (auto-BMT) or peripheral stem cells (PSC) is currently being studied. At the Research Institute of Pediatric Oncology and Hematology, Russian Cancer Research Center named after. N.N. Blokhin of the Russian Academy of Medical Sciences has developed treatment protocols for patients using auto-BMT and PSK in high-risk AML patients in first remission and in case of disease relapses. Already today, encouraging results of treatment have been obtained.
Due to the fact that AML is represented by a group of heterogeneous diseases, the main plan for optimizing treatment is the individualization of therapy, supplemented by preventing the risk of relapse and knowledge about the biology of individual AML subvariants.
New drugs introduced into treatment protocols for pediatric AML in the last decade are 2-chlorodeoxyadenosine (2-CDA) and fludarabine. The use of new agents in therapy, including immunotherapy with interleukin-2, lymphokine-activated killer (LAK) cells generated from peripheral blood mononuclear cells, provides hope for significant advances in the treatment of AML in the future.
The Leukemia Chemotherapy Department of the Research Institute of Pediatric Oncology and Hematology, established 25 years ago, treated 200 AML patients aged from 1.5 months to 16 years. Over the past 10 years, thanks to the use of new approaches to the treatment of children with AML with the inclusion of new chemotherapeutic agents and BMT, it has been possible to increase patient survival to 50%, which is twice as high as the results of therapy using the “7+3” treatment program (cytosine arabinoside and rubomycin).
Thanks to the introduction of new technologies into the diagnosis and program therapy of AML, significant progress has been achieved in the results of treatment of relapsed AML in children.
Svetlana MAYAKOVA, Head of the Department of Chemotherapy for Leukemia, Doctor of Medical Sciences. Alexander POPA, senior researcher at the leukemia chemotherapy department, candidate of medical sciences. Research Institute of Pediatric Oncology and Hematology, Russian Cancer Research Center named after N.N. Blokhin, Russian Academy of Medical Sciences.
The first signs of leukemia in adults
Symptoms are nonspecific and have common features for many diseases. Manifestations depend on the massiveness of the lesion and its location.
The first signs of leukemia in adults:
- causeless low-grade fever, profuse sweating at night;
- weakness, increased fatigue;
- swollen lymph nodes;
- enlarged spleen and liver;
- joint pain;
- constant headaches;
- external manifestations associated with bleeding disorders: bleeding gums, bruises, nosebleeds, the presence of red dots under the skin.