Meningitis is characterized by inflammation of the meninges of the spinal cord and brain. The disease is classified as infectious. Meningitis affects adults and children. In children, meningitis often occurs in a fulminant or acute form. Adults are more likely to suffer from meningitis caused by meningococcal infection; women are sick less often than men.
The Yusupov Hospital diagnoses and treats meningitis. In the laboratory you can undergo a number of tests for the causative agent of the disease, and experienced doctors provide consultations in the hospital. Meningitis can have a fulminant course, in which case qualified assistance should be provided immediately. With meningitis, it is very important that the diagnosis be made in the first days of the disease.
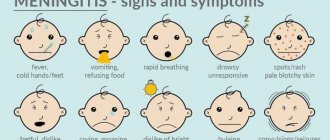
Symptoms of meningitis
Signs of meningitis are as follows:
- severe pain in the head,
- temperature, pain in the muscles of the neck,
- hearing loss,
- fainting,
- vomiting and nausea,
- mental problems (paranoia, delusions, excited or apathetic state, increased anxiety),
- convulsive states,
- hives,
- drowsiness.
It all depends on the type of meningitis in adults , so the following stages of the disease can be noted:
- Purulent meningitis . The form is severe, pus appears in the brain capsules. This disease is provoked by bacterial infections, more precisely: staphylococcus, streptococcus, pneumococcus, meningococcus.
- Serous meningitis . The disease is less severe than the first option. At the time of inflammation, no pus appears. This is a kind of viral meningitis. This category includes such types as tuberculosis, influenza, mumps, and syphilitic.
Depending on the course of the disease, the following forms are observed:
- Instant. Symptoms of meningitis in children appear instantly. A person can die in the first 24 hours after infection.
- Spicy. Infectious type meningitis occurs within a couple of days after infection. A person can die instantly. Meningitis symptoms in adults have a bright course.
- Chronic. Symptoms gradually appear and get worse.
Depending on the duration of meningitis and the proliferation of inflammation, there are the following forms:
- Basal. Inflammation occurs in the center of the brain.
- Convexital. Pathological processes concern convex areas of the brain.
- Total. Inflammation affects all parts of the brain.
- Spinal. Inflammation is observed on the surface of the spinal cord.
Depending on the severity, the disease can be mild, moderate or severe.
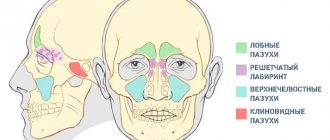
Sinusitis and meningitis: the relationship of diseases
Meningitis develops as an independent disease and can be a complication of pathological processes. Sinusitis and meningitis are interrelated, since the accumulation of pus in the maxillary sinuses can cause inflammation of the lining of the brain. It is important for people at risk to know how sinusitis turns into meningitis and what symptoms the patient experiences. The development of sinusitis by contact occurs against the background of an existing infectious process. Infection accumulated in the paranasal sinuses can cause inflammation of the meninges.
The development of complications with sinusitis is rare, since modern specialists use effective treatment methods. However, if treatment is untimely and ineffective against the background of reduced immunity, the patient may develop meningitis. If a patient suspects meningitis or their health has sharply worsened, it is necessary to consult a general practitioner or neurologist, who will prescribe an examination and determine the cause of the problem.
At the Yusupov Hospital, patients are provided with a wide range of medical services, which include examinations, therapeutic measures, disease prevention and recovery after illness. If meningitis is suspected, patients are urgently hospitalized.
The most important and revealing test for suspected inflammatory processes in the membranes of the brain and spinal cord is a lumbar puncture. It is necessary to examine the cerebrospinal fluid to identify the cause of inflammation and prescribe adequate therapy.
Causes of the disease
The main causes of meningitis in children, symptoms and signs, lie in various infectious pathogens. The types of disease differ from each other depending on the sources:
- Bacterial. Often the disease is provoked by microbes, in particular, we are talking about staphylococcus, streptococcus, meningococcus, and E. coli.
- Viral. People suffering from meningitis often have herpes, mumps, and influenza viruses.
- Candida. Occurs due to candida and critococci.
- Simple microbes. These include amoebas and toxoplasma.
In a separate group, diseases of a combined form appear. In this situation, the disease appears due to several different pathogens.
Meningitis
The source of the disease are patients with generalized forms of meningococcal infection, acute nasopharyngitis and “healthy” carriers.
There is a fairly wide ratio between patients and bacteria carriers (1:2000 - 1:50,000). During periods of outbreaks, up to 3% of the population of bacteria carriers is registered, during epidemics - up to 30%. The carrier period is about 3 weeks. In 70%, bacterial carriage ceases within 1 week.
In patients with chronic diseases of the nasopharynx, this period is significantly longer. The most virulent strains are isolated by patients with generalized forms. Despite this, their rapid hospitalization and isolation do not have such an impact on the spread of infection as it does in “healthy” carriers.
Meningitis carriers are identified during mass examination of individuals from foci of the disease or accidentally, during examination of smears taken from the mucous membrane of the nasopharynx. Carriers of meningococci do not have any symptoms of the disease. The more severe the epidemic situation, the more carriers of the infection are identified in groups.
Out of 200 bacteria carriers, 1 bacteria carrier gets sick.
Rice. 3. The mechanism of transmission of meningococcal infection is aerosol (droplet).
How can you get infected?
If you are interested in how you can become infected with meningitis, then first you should know about the way the infection multiplies. The methods of its reproduction are different, but the most common are:
- Airborne (the patient may sneeze and cough).
- Contact and household (personal hygiene rules are not followed).
- Oral-fecal (eating unwashed foods or eating with unwashed hands).
- Hematogenous (infection occurs through blood).
- Lymphogenic (infection through lymph).
- Placental (at the time of pregnancy and birth of a child from mother to her fetus).
- If a person bathes in dirty water, the infection enters the body.
The incubation period for this disease ranges from 2 to 4 days, this period from infection to the first signs. But sometimes it lasts a couple of hours or, on the contrary, it takes up to 20 hours. It is also important to consider that the disease can be primary and secondary. The first option is an independent disease. The second is a consequence of the fact that there is already an infection in the body, for example, a person suffers from influenza, otitis media, tuberculosis.
meningitis symptoms
If it is serous meningitis, then it is considered contagious. If the disease is secondary, then other people will not become infected with it.
Symptoms of meningitis that every parent should know
10.03.2020
Hearing the word “meningitis” from a doctor when diagnosing a child, any parent will be horrified. Having an extremely poor understanding of the symptoms and etymology of the disease, everyone has heard about the terrible consequences. The disease is insidious, sometimes taking a lightning-fast form. Therefore, all parents need to know the enemy as best as possible, so as not only to give the child the opportunity to rest at home with a general malaise, but to call an ambulance and provide emergency assistance.
What is meningitis?
Meningitis is an inflammation of the membranes of the brain that develops as a result of a bacterial, viral or fungal infection.
The cause of bacterial meningitis can be any purulent lesion in the body. This species is of particular importance because it is the most dangerous type of disease.
Symptoms appear unexpectedly, and the disease develops at lightning speed. That's when minutes count.
With viral meningitis, the causative agent can be any of the common infections - chickenpox, measles, rubella, mumps, and influenza. Accordingly, it can be infected from another person. What makes it even more dangerous is that parents have no way to track and check all the people who come into contact with their child. It turns out that no one is immune from the disease.
The fungal form of meningitis most often affects people with weakened immune systems . At risk are carriers of HIV infection and people with cancer undergoing chemotherapy. This form is not transmitted by airborne droplets.
Symptoms
- Sudden rise in temperature. The fever begins suddenly, the child complains of chills. High body temperature, which is very difficult to bring down with antipyretics, and at the same time cold hands and feet .
- Unbearable stabbing headache. In infants, one of the symptoms may be swelling of the fontanel.
- Deterioration of vision , impaired mobility of the eyeballs and, as a result, double vision . Also, the patient does not have the ability to focus his gaze on an object.
- Stomach pain , nausea , vomiting, loss of appetite. Typically, “fountain” vomiting is characteristic, which is not associated with food intake and does not bring relief. Afterwards the headache only gets worse.
- Tearing and increased nausea in bright sunlight. The child squints and experiences pain when exposed to direct sunlight. In this case, it is recommended to curtain the windows and wait for the doctor in the twilight.
- Increased tone of the occipital muscles, or Brudzinski's sign. You can identify it yourself. To do this, you need to put the back of the child's head on your hand and bend your neck , bringing your chin to your chest . A patient with meningitis will experience pain during such manipulations, and his legs will instantly bend at the knees .
- Pointer dog pose. In severe cases of the disease, the child lies in a certain position: legs bent at the knees and pressed to the stomach , arms leaning against the chest, head tilted back.
- Skin rashes. to distinguish a meningitis from a normal rash. To do this, take a glass glass, place it on the rash and press firmly. If the spots do not fade, you should urgently call a doctor .
What to do if you notice symptoms?
If a child exhibits at least one of these symptoms, you should immediately call a doctor or an ambulance. On site, an experienced employee will conduct a full examination and confirm or refute the diagnosis. If the disease is still detected, it is recommended not to refuse hospitalization and undergo treatment in a hospital . In this case, the likelihood of avoiding consequences is much higher.
Published in Neurology Premium Clinic
Who is at risk?
A key factor contributing to the onset of meningitis is a weak immune system. It is the body’s defense against various infections. Human immunity becomes weak due to:
- previously suffered infectious diseases (respiratory, pneumonia, pharyngitis, influenza, sore throat),
- chronic pathologies, especially syphilis, HIV, tuberculosis, liver cirrhosis, severe stress,
- vitamin deficiency and strict diets,
- head and back injuries,
- total hypothermia of the body,
- alcohol and drug abuse,
- long-term use of tablets with non-compliance with recommendations.
All this can cause infection in a person, as the body becomes weak.
First aid when detecting signs
It is important to understand that if you suspect the occurrence of this disease, it is necessary to take urgent action.
Undoubtedly, the patient should be transferred to doctors as quickly as possible. However, before the doctors arrive, it is necessary to take measures to alleviate the patient’s condition :
- If there is a high temperature (39 and above), the patient should undress, apply a cold compress to the head, wipe the body with a damp cloth, and turn on the fan.
- Medicines to reduce fever (eg Paracetamol) may be given.
- Make sure your teenager drinks plenty of water.
- Stay near the patient until the doctors arrive.
When should you see a doctor?
Every person needs to know how to detect signs of meningitis in children . There is no need to delay contacting a doctor if you often experience headaches, nausea and vomiting, an increase in body temperature, photophobia, sensitivity to sounds, or muscle pain in the back of the head. Also considered key symptoms are apathy and a constant desire to sleep, fainting, anxiety, and convulsions. A rash with meningitis is also observed; it affects the skin and mucous membranes. Mental disorders are also observed.
diagnosis of meningitis
Meningitis must be treated by a doctor in the infectious diseases department.
Clinical forms and classification of meningococcal infection
Meningococcal infection is characterized by large polymorphism, which is associated with the pathogenesis of the disease.
- Clinical forms of the disease are divided into localized and generalized. Localized forms include meningitis and nasopharyngitis, generalized forms include meningococcemia with rashes (typical form) and without rashes (atypical form).
- Localized and generalized forms can occur without metastasis to internal organs and with metastasis (meningitis, meningoencephalitis - the most common forms and pericarditis, myocarditis, arthritis, pneumonia, iridocyclitis and other rare forms).
- According to the severity of the course, meningococcal infection is divided into mild, moderate, severe and very severe. The degree of toxicosis, adrenal insufficiency, the rate of progression and severity of signs of damage to the central nervous system, the development of disseminated intravascular coagulation syndrome and infectious-toxic shock are the main criteria for the severity of meningococcal infection.
- If the duration of the disease is up to 3 months, they speak of an acute course, more than 3 months - a protracted course, and more than 6 months - a chronic course. The chronic form of menigococcemia and meningitis can have a relapsing course.
Rice. 2. The photo shows meningococcal infection in children. One of the main symptoms of the disease is a rash. Minor hemorrhages in the skin with meningococcal infection (left) and extensive bruises in a child with severe meningococcal sepsis (right).
How to prepare for going to the doctor?
To go to the doctor, you don’t need to make any extensive preparations; on the contrary, if there are symptoms of meningitis , you shouldn’t put off going to the doctor, in this case you need to react immediately. Just remember all the signs that you had and tell your doctor about them. This will help make a correct diagnosis. You can't ignore these signs. Signs of meningitis in an adult can appear within a couple of hours, so urgent help is needed to avoid complications and even death.
Why is self-medication dangerous?
Meningitis is a very dangerous disease, the occurrence of which in a teenager often poses a threat to life.
It is important to understand that self-medication is not acceptable here, since sometimes the countdown of time can already go to the clock. Urgent intervention by professionals in white coats is required. Therapy should be carried out exclusively in a medical institution , where treatment is prescribed by a doctor according to a special regimen, including antibiotics, vitamins and diuretics.
It is important to understand that the final result largely depends on the stage at which full treatment began. When the disease starts, in the best case, serious consequences can occur; in the worst case, the teenager dies.
So, the main complications of meningitis in a teenager include :
- the occurrence of blindness;
- strabismus;
- paralysis of various parts of the body;
- development of bedsores;
- developmental delay.
Read more about treating meningitis at home in this article.
How is the treatment carried out?
Treatment of meningitis is performed using several methods:
- Antimicrobial. Used when illness is caused by germs.
- Antiviral. Here doctors prescribe interferon and glucocorticosteroids to block the spread of the virus and improve the functioning of the immune system.
- Antifungal. If the disease appears due to candida, then antimycotic medications are used.
Therapy is also aimed at eliminating symptoms, that is, they give pain-relieving injections, normalize body temperature, and eliminate intoxication and dehydration.
Signs and symptoms of meningoencephalitis
Meningoencephalitis is a rare form of meningococcal infection. It accounts for 3 to 6% of all cases. The disease is always severe. General intoxication syndrome is combined with meningeal and encephalic syndromes. In recent years, a combination of meningoencephalitis and meningococcemia—acute meningococcal sepsis—has been observed.
- Serous inflammation of the meninges quickly acquires the character of purulent inflammation. The inflammatory process spreads to the white matter of the brain. After 5 - 8 days, the pus turns into a fibrous mass.
- After 12 hours, symptoms of meningeal irritation appear, abdominal, periosteal and tendon reflexes decrease, and their unevenness is noted.
- General cerebral symptoms increase rapidly. Psychomotor agitation, auditory and visual hallucinations and delirium are replaced within a day by a deep disturbance of consciousness (stupor).
- As the symptoms of intoxication and cerebral edema decrease, signs of encephalitis appear. Focal cerebral insufficiency manifests itself in the form of damage to the cranial nerves - facial, oculomotor, trigeminal, sublingual and auditory; cortical and subcortical paresis and paralysis develop. Sometimes convulsions appear, which are general or local in nature, the psyche is disturbed, amnesia develops, auditory and visual hallucinations, depression or euphoria appear.
- There are moderate signs of changes in the functioning of the cardiovascular system. When the vasomotor center is involved in the pathological process, bradycardia occurs, and sometimes cardiac arrest is recorded.
- With hyperthermia, increased breathing is observed. During convulsions, short-term cessation of breathing may occur. Damage to the respiratory center leads to respiratory arrest.
The disease lasts from 4 to 6 weeks. In case of timely and adequate treatment, the prognosis is favorable. With late diagnosis and untimely treatment, the prognosis of the disease is unfavorable. Fatalities are common. Surviving children have epilepsy, delayed psycho-motor development and hydrocephalus. One of the severe complications of meningoencephalitis is inflammation of the ependyma of the ventricles of the brain. Damage to the auditory nerve can result in deafness.
In children suffering from rickets, malnutrition, and exudative diathesis, a protracted course (up to 2 months) of the disease is noted. There are also cases of long-term meningoencephalitis. The reasons for the chronicity of the pathological process have not been sufficiently studied.
Rice. 7. The photo shows purulent meningitis.
Misconceptions regarding the treatment of meningitis
- You can get meningitis if you don't wear a hat. Usually these phrases scare children. Sources of infection are considered to be a consequence of the inflammatory process, but not cold.
- Meningitis is not a dangerous disease at all. In reality, death is possible.
- Meningitis cannot be cured. In reality, fungal and bacterial forms can be treated with drugs, since special drugs have been created against such infections. If the form is viral, then things are worse, since there are no effective antiviral agents.
- After meningitis, a person is prescribed disability. In reality, after suffering bacterial meningitis, only 20% of people become disabled. The most common complication is hearing loss, but there are also problems with remembering and completing schoolwork if meningitis is detected in children.
Diagnosis and treatment
Neurologists make the initial diagnosis of meningococcal meningitis during a clinical examination, during which a spinal tap is performed to obtain cerebrospinal fluid.
Then the laboratory technicians perform a bacterioscopy of the cerebrospinal fluid. The diagnosis is confirmed by growing microorganisms found in the cerebrospinal fluid or blood. The laboratory also studies biological fluids using polymerase chain reaction. To make the optimal choice of antibacterial agents, laboratory technicians identify the serotype of the pathogen and determine sensitivity to antibiotics. A patient with meningococcal meningitis is hospitalized at the neurology clinic of the Yusupov Hospital. Antibacterial therapy begins immediately after a spinal puncture. Patients are prescribed antibacterial or antiviral drugs immediately after receiving the results of a cerebrospinal fluid analysis and identification of the infectious agent. If lumbar puncture is contraindicated, antibiotics are selected empirically. The following antibiotics are used for initial therapy:
- Penicillin;
- Ampicillin;
- Chloramphenicol;
- Ceftriaxone.
They are administered intramuscularly and intravenously.
Before the first administration of the antibiotic, an infusion of glucocorticoid hormones is given. To reduce cerebrospinal fluid pressure, dehydration therapy is carried out with furosemide, Lasix or mannitol. Infusion therapy is carried out with solutions that have a detoxifying effect and replenish fluid loss by the body. They are administered intravenously. Timely establishment of an accurate diagnosis and adequate antimicrobial therapy allow doctors at the Yusupov Hospital to quickly stabilize the condition of patients with infectious meningitis and prevent the development of complications. If there is reliable information about a severe allergy to beta-lactams, vancomycin is prescribed for pneumococcal meningitis, and chloramphenicol is prescribed for meningococcal meningitis. Patients with identified risk factors for listeria infectious meningitis are prescribed intravenous amoxicillin in addition to third-generation cephalosporins. Dexamethasone is used simultaneously with antibiotics for pneumococcal and hemophilic infectious meningitis.
If the nature of infectious bacterial meningitis is not established, antibacterial therapy is carried out for 10–14 days. For meningitis caused by meningococcus, the duration of antibiotic use varies from 5 to 7 days. Meningitis caused by Haemophilus influenzae type b requires antibiotic therapy for 7-14 days. The course of antibacterial treatment for listeria meningitis is 21 days, and for meningitis caused by Pseudomonas aeruginosa or gram-negative microorganisms, it can last for 21–28 days.
Symptomatic therapy for infectious meningitis involves the use of diuretics, infusions of fluid replenishers, and the administration of antipyretic drugs and analgesics. For increased intracranial pressure, a 20% mannitol solution is prescribed. It increases plasma pressure, and thereby promotes the transfer of fluid from brain tissue into the bloodstream. Diacarb prevents the formation of cerebrospinal fluid. Furosemide inhibits the reabsorption of sodium in the renal tubules, resulting in increased diuresis.
In the presence of convulsive syndrome, doctors prescribe diazepam, sodium hydroxybutyrate, and aminazine to patients with infectious meningitis. From the very first minutes of a patient’s admission to the neurology clinic, doctors administer oxygen therapy. If indicated, the patient is given tracheal intubation and artificial ventilation.
What prevention is there?
There is a special vaccination against meningitis. This is what helps prevent the spread of the disease. It should be done for people who often communicate with infected people. Doctors also recommend doing this to children, as they are often exposed to this disease. Vaccination against meningitis is indicated for people with weak immune systems.
Moreover, prevention consists of increasing human immunity. It is necessary to strengthen the body, lead a healthy lifestyle, play sports, often be in the fresh air, and also protect yourself from infectious sources. You can also drink complexes with vitamins and minerals to boost your immunity. It is very important to maintain a balanced diet.
Causes and mechanism of development
Meningococcal meningitis is a bacterial infection of the meninges. The causative agents of the infection are Neisseria meningitis (meningococci) of twelve serological groups. They are transmitted from person to person through droplets of secretions from the throat and upper respiratory tract of the bacilli carrier or a sick person. The spread of microorganisms is facilitated by close, prolonged contact:
- Sneezing or coughing towards another person;
- Sharing utensils;
- Kisses;
- Living in close proximity to an infected person.
- According to the course of the disease, the following forms of infectious meningitis are distinguished:
- Fulminant (a detailed clinical picture is formed in less than 24 hours);
- Acute;
- Subacute.
According to the nature of the inflammatory process, purulent and serous meningitis are distinguished.
With primary infectious meningitis, infectious agents penetrate from the external environment directly into the nervous tissue. Secondary meningitis develops when the infectious agent moves from the primary foci of inflammation to the membranes of the brain. Make an appointment