Meningitis - symptoms and treatment
The variety of pathogens and the individual characteristics of individuals in the human population also determine the fairly pronounced variability in the forms and manifestations of meningitis and the risk of infection for other people, so in this article we will focus on the most significant forms of diseases and their causative agents in social terms.
Meningococcal meningitis is always an acute (acute) disease. Caused by Wekselbaum's meningococcus (a gram-negative bacterium, unstable in the environment, at a temperature of 50 degrees Celsius it dies after 5 minutes, UV irradiation and 70% alcohol kill almost instantly). The source of the spread of infection is a sick person (including meningococcal nasopharyngitis) and a bacteria carrier; transmission occurs by airborne droplets.
The site of introduction (gate) is the mucous membrane of the nasopharynx. In the vast majority of cases, the infectious process does not develop or local forms of the disease develop. When meningococcus overcomes local anti-infective barriers, hematogenous spread of infection occurs and a generalized meningococcal infection occurs, including the development of meningococcal meningitis, which, in the absence of adequate treatment, ends in death in more than 50% of cases. In the pathogenesis of the disease, toxins that are released after the death of bacteria in the bloodstream and damage to the walls of blood vessels play a role, which leads to hemodynamic disturbances, hemorrhages in organs and profound metabolic disorders. Hyperirritation of the meninges occurs, the development of purulent inflammation of the tissue and a rapid increase in intracranial pressure. Often, due to edema and swelling of the brain tissue, the brain becomes wedged into the foramen magnum and the patient dies from respiratory paralysis.
The latent period of illness is from 2 to 10 days. The onset is acute (even more correctly, acute). In the first hours of the disease, there is a sharp increasing increase in body temperature to 38.5 degrees and above, severe lethargy, fatigue, pain in the periorbital region, loss of appetite, and a sharp headache. A characteristic sign of a headache is a constant increase in its intensity, diffuse pain without clear localization, bursting or pressing in nature, causing true agony for the patient. At the height of the headache, vomiting occurs without preceding nausea, which does not bring any relief. Sometimes in patients with a severe uncontrolled course, mainly in children in an unconscious state, there is an uncontrollable cry, accompanied by clasping the head with one’s hands - the so-called. “hydrocephalic cry” caused by a sharp increase in intracranial pressure. The appearance of the patients is etched in the memory - sharpening of facial features (Lafora’s symptom), meningeal posture on the 2-3rd day of the disease (still “coping dog”). Some patients develop hemorrhagic rashes on the body, resembling a star-shaped rash (an unfavorable sign). Over the course of 2-3 days, the severity of symptoms increases, hallucinations and delusions may appear. The degree of impairment of consciousness can vary from somnolence to coma; if untreated, death can occur at any time.
Tuberculous meningitis is a slowly developing pathology. It is mainly secondary, developing in the context of existing tuberculosis in other organs. It has several periods of development, consistently developing over a long time:
1. prodromal (up to 10 days, characterized by mild symptoms of general malaise)
2. sensorimotor irritation (from 8 to 15 days, the appearance of initial cerebral and weak meningeal manifestations)
3. paresis and paralysis (attracts attention from the 3rd week from the onset of the infectious process in the form of changes and loss of consciousness, difficulty swallowing, speech).
Initially, a moderate increase in body temperature appears without pronounced jumps and rises, quite tolerable headaches of low intensity, well relieved by taking analgesics. In the future, headaches intensify, nausea and vomiting become involved. An invariable sign of tuberculous meningitis is a rise in temperature, fever, and the numbers and duration can vary from subfebrile to hectic values. Gradually, from the end of the second week, symptoms of disorientation and stupor appear and slowly increase, ending in deep “congestion” of the patient, stupor and coma. Dysfunction of the pelvic organs and abdominal pain develop. Meningeal symptoms also gradually develop, and truly classic symptoms (the “pointing dog” position) develop only in advanced cases.
Herpetic meningitis is most often caused by herpes simplex viruses types 1 and 2, the chickenpox virus and develops against a background of weakening of the body due to acute respiratory viral infections or serious immunosuppression, incl. AIDS. It is divided into primary (when the process develops during initial infection with the virus) and secondary (reactivation of the infection against the background of decreased immunity). Always an acute disease, the primary manifestations depend on the previous premorbid background. More often, against the background of acute respiratory viral infections, herpetic rashes of the perioral area and genital organs, a severe headache of a diffuse nature occurs, increasing over time, and vomiting, which does not bring relief. All this can occur against the background of a moderate or high increase in body temperature and mild meningeal symptoms. Brain damage is often associated; in such cases, mental disorders (often aggression), hallucinations, disorientation, and generalized convulsions occur within 3-4 days. With proper treatment, the prognosis is usually quite favorable; in the absence of adequate treatment in conditions of impaired immunological resistance, death or persistent residual effects are possible [2].
Relationship with sinusitis. If left untreated, sinusitis can cause the bones in the sinuses to melt.
Through them, pus enters the meninges, and meningitis develops.
What is this?
Meningitis (from the Latin meninx - “brain membrane”, suffix -itis - “inflammation”) is an inflammation of the membranes of the brain and spinal cord.
It is the membranes, and not the brain tissue itself. Inflammation of the brain is encephalitis (from the Latin encephalon - “brain”, suffix -itis - “inflammation”).
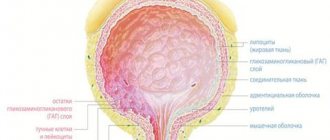
The brain has three membranes:
- hard;
- arachnoid (arachnoid);
- soft (Fig. 1).
Figure 1. Meninges of the brain.
Source: SVG by Mysid, original by SEER Development Team [1], Jmarchn / Wikipedia (Creative Commons Attribution-Share Alike 3.0 Unported license) The dura mater is adjacent to the inner surface of the skull. It consists of two leaves: outer and inner. The outer leaf is tightly adjacent to the inner surfaces of the bones of the vault and base of the skull, the inner leaf forms dense outgrowths of this shell into the cranial cavity, which play the role of a frame for the brain and divide it into several sections. Between the leaves there are important formations - venous sinuses. They collect blood, which flows from the brain, enters the jugular veins and then into the heart through the superior vena cava.
The arachnoid membrane is thin, it occupies an intermediate position between hard and soft and connects them to each other.
Finally, the pia mater is loose and covers the brain, extending into all its grooves and crevices. In the thickness of the soft shell there are a large number of vessels that nourish the brain tissue.
Most often (perhaps due to the abundant blood supply), it is the pia mater that becomes inflamed. However, inflammation of the dura and arachnoid membranes also occurs. If both the arachnoid and soft membranes are inflamed at the same time, the disease is called leptomeningitis, if we are talking only about the hard membrane - pachymeningitis.
The spinal cord also has dura, arachnoid and pia mater. In structure, they are almost no different from the membranes of the brain. Their inflammation is also called meningitis. It is dangerous because it can spread to the tissue of the spinal cord itself. However, these will be different pathological conditions with their own complications.
Consequences
Serous meningitis can have various consequences.
When the first symptoms of this disease appear, it is important to seek medical help promptly. The best thing to do is call an ambulance. Treatment of serous meningitis must necessarily take place in a hospital setting. Self-medication is unacceptable. The sooner adequate medical care is provided, the greater the chance that the consequences of the disease will never appear or will be minimal.
In cases where the patient delays treatment for too long, the following complications may occur:
- blindness;
- deafness;
- brain disorders;
- dysfunction of the speech apparatus;
- delay in psychomotor development.
In medical practice, in the advanced stage of serous meningitis, in the absence of treatment, paralysis, coma and death occurred. But this is rather an exception to the rule. In most cases, serous meningitis is not as serious as, for example, tuberculosis.
Even with favorable treatment and prognosis, the patient may experience headaches for a long time. If after a course of therapy pain persists for more than 2 months, you should definitely consult a doctor. If necessary, repeated examination is possible.
How to prepare for going to the doctor?
To go to the doctor, you don’t need to make any extensive preparations; on the contrary, if there are symptoms of meningitis , you shouldn’t put off going to the doctor, in this case you need to react immediately. Just remember all the signs that you had and tell your doctor about them. This will help make a correct diagnosis. You can't ignore these signs. Signs of meningitis in an adult can appear within a couple of hours, so urgent help is needed to avoid complications and even death.
Additional diagnostic measures
During the diagnosis, a blood test and analysis of the separated elements of the skin rash are also carried out. If a specialist suspects the presence of secondary purulent meningitis, then an additional examination is prescribed, the purpose of which is to identify the primary infectious focus. For this, the patient is sent for consultation to a pulmonologist, otolaryngologist or therapist. Effective diagnostic measures here would be otoscopy, x-ray of the paranasal sinuses, and x-ray of the lungs.
Differential diagnosis is carried out with viral meningitis, subarachnoid hemorrhage, meningism, which is also observed in typhus, leptospirosis and severe cases of influenza.
Causes
Serous viral meningitis is an infectious disease.
In 75-80% of cases, viral meningitis is caused by enterovirus infection (Coxsackie and ECHO viruses). Less commonly, the cause of serous meningitis is the mumps virus, adenoviruses, Epstein-Barr virus (the causative agent of infectious mononucleosis), cytomegalovirus, herpes and measles viruses. HIV infection can also lead to the development of viral meningitis. Viral meningitis has a seasonal incidence, which depends on the type of pathogen. Most cases of serous meningitis occur in the summer. The mumps virus has a peak incidence in spring and winter. Serous meningitis can be not only viral, but also bacterial (with syphilis, tuberculosis), and sometimes fungal.
Sources
- Global, regional, and national burden of meningitis, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 [Electronic resource] // The Lancet. Neurology, 2021.
- Epidemiology of Meningitis Caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenza [Electronic resource] // cdc.gov, 2021.
- Rebecca M. Cantu; Joe M Das. Viral Meningitis [Electronic resource] // NCBI, 2021.
- Meningitis [Electronic resource] // who.int
- What Do You Want to Know About Meningitis? [Electronic resource] // healthline.com, 2021.
- YouTube. Research and assessment of meningeal symptoms in a child.
- Clinical protocol for diagnosis and treatment. Meningitis in children and adults [Electronic resource] // rcrz.kz, 2021.
- Kenadeed Hersi; Francisco J. Gonzalez; Noah P. Kondamudi. Meningitis [Electronic resource] // NCBI, 2021.
Diagnostics
To make a diagnosis of meningitis and determine its causative agent, it is necessary:
- Collect anamnesis. It is important to understand whether the patient has had contact with people infected with meningitis, has traveled to areas where meningitis is endemic, and whether he or she has specific immune status—possibly suffering from HIV or other immunodeficiencies, or taking medications that suppress the immune system.
- Assess the general condition. The doctor conducts a clinical examination of the patient, assesses the severity of his condition, and checks for the presence of specific symptoms.
- Carry out the necessary laboratory tests. This includes classic laboratory tests, such as a general urine test, a complete blood count, a biochemical blood test, and most importantly, a lumbar puncture.
Lumbar puncture is a procedure during which, under local anesthesia, the doctor inserts a special needle into the spinal cord (directly into its subarachnoid space) between the III and IV lumbar vertebrae and collects cerebrospinal fluid. Next, it is examined and the color, the presence of sediment, the predominance of certain cells, the presence of bacteria, the amount of protein and glucose are assessed. Based on the results of the study, it is possible to determine the type of meningitis, draw a conclusion about the nature of the inflammatory process, isolate the pathogen, and determine the necessary treatment.
It is worth noting that if bacterial meningitis is suspected, antibacterial therapy is prescribed immediately, before test results are obtained. This is done with the aim of starting treatment as early as possible, since in the case of meningococcal infection, the clock is ticking. Further, based on the test results, treatment can be adjusted and other antibiotics may be prescribed.
At-risk groups
There are factors that increase your risk of getting meningitis. These include:
- Age. Newborns, children of primary school age, adolescents 13-17 years old, as well as older people are considered more susceptible to meningitis pathogens.
- Organized teams. Outbreaks of meningococcal infection have been observed more than once in places where a large number of people are forced to stay in one area for a long time: in barracks, university campuses, etc.
- Medical factors. This may include certain health problems: immunodeficiency conditions and diseases of the immune system, HIV infection, absence of a spleen, taking certain groups of medications that lower natural immunity (chemotherapy, cytostatics, etc.), as well as surgical interventions.
- Contact with infections that cause meningitis. This factor is especially relevant for microbiologists, who may regularly come into contact with meningitis pathogens due to the specific nature of their work.
- Trips. Visiting geographic areas where a particular pathogen is endemic (its characteristic habitat) also increases the risk of meningitis. For example, staying in the countries of the meningitis belt in Africa.
What prevention is there?
There is a special vaccination against meningitis. This is what helps prevent the spread of the disease. It should be done for people who often communicate with infected people. Doctors also recommend doing this to children, as they are often exposed to this disease. Vaccination against meningitis is indicated for people with weak immune systems.
Moreover, prevention consists of increasing human immunity. It is necessary to strengthen the body, lead a healthy lifestyle, play sports, often be in the fresh air, and also protect yourself from infectious sources. You can also drink complexes with vitamins and minerals to boost your immunity. It is very important to maintain a balanced diet.