Inflammation of the pancreas is accompanied by constant or periodic pain of various types. This is the main symptom of pancreatitis, which can develop in acute and chronic forms. At the first manifestation of girdle pain around the abdomen, you should consult a doctor for examination. In most cases, treatment with medications and long-term diet is indicated.
Inflammation of the pancreas
Pancreatitis is inflammation of the pancreas and can be acute or chronic. Causes – poor diet, stones in the bile ducts, poisoning, smoking, chronic alcoholism, disruption of the gastrointestinal tract (stomach, duodenum), viral diseases, infections, etc. Symptoms of acute pancreatitis – nausea, vomiting, heartburn, aching, monotonous pain in abdomen, in the left hypochondrium, persisting for several days. As well as spasmodic pain in the lower abdomen, flatulence, abnormal bowel movements (diarrhea or constipation), chills or excessive sweating, an unpleasant taste in the mouth, and changes in skin color.
How pancreatitis develops
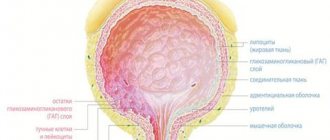
Inflammation in the gland occurs due to the fact that enzymes secreted by the pancreas accumulate in it and begin to destroy it itself (Fig. 3). Pain appears in the left upper abdomen, under the ribs, which then begins to radiate to the left shoulder blade. In most cases, the pain is accompanied by vomiting and fever. Enzymes, instead of going to the duodenum and further to other digestive organs, enter the blood. Intoxication of the body occurs.
Figure 3. Development of pancreatitis. Source: aboutkidshealth ca
When the pancreas loses its functionality, the duodenum is left without protection from stomach acid, which leads to the formation of ulcers in it. After all, before the pancreas produced sodium bicarbonate, which protected the intestines. Without the enzymes necessary for digestion, the intestines cannot cope with its contents. Intestinal obstruction and swelling of the organ occurs. In the chronic form of the disease, the pancreas itself suffers - it becomes covered with scars (pancreatic necrosis) and ceases to cope with its functions of producing enzymes and hormones.
Treatment of pancreatic inflammation
Treatment of acute pancreatitis should take place in a hospital.
First aid - you need to apply an ice bag to the left hypochondrium, avoid eating any food. Drug treatment includes taking antispasmodics, painkillers (opioid analgesics), and antiemetics. In the acute phase, infusion drugs are administered intravenously. For complications, antibiotics may be prescribed. Fasting is observed for three to five days or parenteral nutrition is used.
Therapy for the chronic form of the disease is based on quitting smoking, drinking alcohol, diet therapy with a small amount of fat in the diet, using painkillers, taking enzyme preparations; antidepressants (pregabalin, gabapentin) can be prescribed to relieve pain, as well as treatment of complications.
If there are stones in the gland ducts, then it is rational to perform lithotripsy and endoscopic therapy.
Surgical treatment is performed when drug therapy is impossible or the body is tolerant to their action.
The duration of treatment depends on the form and complications of the disease, and on the body’s susceptibility to therapy.
Causes of pancreatitis
Pancreatitis can be hereditary. The situation can be worsened by flaws in the diet, taking medications, bad habits and many other factors. What triggers the appearance of pancreatitis depends on the presence of chronic diseases.
Main reasons:
- injuries of the gastrointestinal tract,
- food poisoning,
- fungal diseases,
- endoscopic operations,
- eating fatty or spicy foods,
- alcohol consumption,
- smoking,
- infectious diseases.
Pancreatic tumors
A pancreatic tumor can be of two types – cancer and a hormonally active tumor.
Men are more often affected; the average age is 55 years. Most often the tumor is localized in the head of the gland. Factors that provoke the development of pancreatic cancer include smoking, chronic pancreatitis, high body mass index, and male gender.
Symptoms of cancer depend on the part of the gland that is affected. If the head of the gland is affected, jaundice may develop, because compression of the bile duct occurs. Skin itching appears. When the body and tail are affected, diabetes mellitus, varicose veins of the esophagus and stomach, and the risk of bleeding develop.
Treatment is surgical or chemotherapy.
Risk factors for the disease
There are some factors that increase the risk of cancer in this organ.
- Male gender. Men get sick 2 times more often than women.
- Age. After 50, the risk of the disease increases several times.
- Place of residence. Pathology occurs more often among city residents than among those living in rural areas.
- Race. Representatives of the Negroid race suffer from pancreatic cancer more often than representatives of the Caucasian race.
- Bad habits. Those who drink alcohol, eat a lot of fatty foods, and smoke are more likely to develop cancer than those who lead a healthy lifestyle.
- Type of work. Workers in hazardous industries are more susceptible to the disease.
- Having diabetes mellitus increases the risk of developing a tumor several times.
Sometimes congenital pathologies of the gland are discovered, which are formed at the stage of embryonic development, when the 2 rudiments of the organ should merge together.
There are such anomalies as:
- split gland, when the rudiments of the organ and its ducts do not merge with each other and 2 ducts flow into the duodenum;
- annular gland, when the tissue of the organ is displaced and completely (in a ring) covers the duodenum, as a result, the intestinal lumen narrows and this interferes with the passage of food;
- An ectopic gland is a collection of pancreatic tissue that does not have any contact with the main organ. Most often, this accumulation of tissue becomes inflamed or turns into a tumor.
Several less common conditions also occur.
- Gland cysts
. They can be congenital or acquired; they occur more often due to injury to the organ or infection with echinococci. They are quite large in size, and often the doctor can detect them even by palpation. - Fistulas
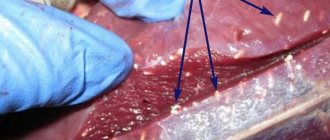
. The fistula looks like a canal of connective tissue that communicates with the duct of the gland. Fistulas can be external, when they exit through the skin, and internal, when they exit to the stomach and intestines. Due to the appearance of fistulas, a significant amount of pancreatic juice is lost, resulting in dehydration and severe exhaustion, which can lead to a coma. - Stones
. Sometimes calcifications form in the ducts - stones ranging in size from grains to small nuts. Stones can cause blockage of the gland, its inflammation, diabetes mellitus, they provoke cysts and abscesses. The pain in the presence of stones is severe, girdling, paroxysmal, and often cannot be relieved even with potent analgesics.
Pancreatic stones
Pancreolithiasis is the formation of stones in the pancreatic ducts.
Often stones form if there is a cyst or tumor; this is one of the complications of chronic pancreatitis. Stagnant processes occur in the organ, the secretion of the pancreas thickens, and the protein precipitates. The ducts dilate, the pressure in them increases, and symptoms of pancreatitis appear. Symptoms of pancreolithiasis:
- burning pain in the abdomen radiating to the back and shoulder blade;
- nausea, vomiting with bile;
- steatorrhea – “fatty” stool;
- diabetes;
- increased salivation;
- obstructive jaundice.
How can the doctor help?
Diagnosis of pancreatic problems includes a number of activities:
- Visual examination of the patient by a doctor. The specialist interviews the patient and observes the color of the mucous membranes and skin.
- Palpation of painful areas. For such an examination, the patient first takes a position lying on his back, and then on his left side. When the pancreas is affected, the pain in the side is usually less severe.
Also, the doctor usually prescribes a list of necessary tests, including:
- General blood analysis. Glandular dysfunction usually causes an increase in white blood cells.
- Detection of trypase, amylase and lipase levels in blood serum.
- Additionally, it is recommended to study liver enzymes: alkaline phosphatase, bilirubin and ATL. Elevated readings may indicate an attack of pancreatitis caused by the movement of gallstones.
- Urinalysis to detect amylase levels.
- Analysis of stool for excess fat, trypsin and chymotrypsin.
Additionally, instrumental diagnostic methods are used:
- Radiography. With its help, it is determined whether the gland is enlarged or not.
- Ultrasound. Helps to examine the features of the contours of the organ, determines the presence of gallstones, and the condition of the excretory duct.
- MRI. It is used to clarify the diagnosis and determines the presence of pancreatic necrosis or fluid in the peritoneum.
Diagnosis of pancreatic diseases
To diagnose diseases of the pancreas, the doctor examines and palpates the abdomen and prescribes laboratory and instrumental methods.
A biochemical blood test examines the level of pancreatic enzymes (amylase, lipase), blood glucose, and liver function tests.
A stool analysis is carried out to assess the deficiency of enzyme production, the presence of undigested food, fat, and certain enzymes (pancreatic elastase) is examined.
Visual instrumental examinations are carried out using transabdominal ultrasound (ultrasound of the abdominal cavity), CT, radiography, magnetic resonance cholangiopancreatography.
What to do?
First of all, it is worth noting that you cannot self-medicate, you must contact a specialist. You should not take painkillers or put heat on your stomach - this can only worsen the process. You need to see a therapist or gastroenterologist, undergo an ultrasound, ECG and MRI. The doctor may also prescribe additional tests or examinations if necessary.
If the disease is diagnosed at an early stage, drug treatment will help. If the disease is advanced, surgical intervention is prescribed. In any case, there is no time to waste, you need to contact specialists and not self-medicate!
Diet for diseases of the pancreas
The diet should include soft, well-chopped food.
Steam, bake, boil, stew foods. Include puree soups and cream soup in your diet. Bread can be consumed dried, yesterday's bread made from first and second grade flour. Meat - chicken, turkey, lean parts of beef, low-fat fish is allowed. Eggs should be in the form of omelettes, steamed in the oven. You can eat non-acidic types of fruits, baked fruits. You can drink rosehip decoction, sugar-free compote, herbal teas, water. Of the fats in the diet, butter with 82.5% fat content and sunflower oil should be present, but limited. Food should be taken warm. It is necessary to exclude sausages, smoked meats, fatty, fried, canned and pickled foods.
Forbidden:
- alcohol;
- spicy food;
- coffee;
- energy, carbonated sweet drinks;
- chocolate;
- ice cream;
- duck, goose meat, pork, lard, bacon;
- legume products;
- garlic, cabbage;
- grapes, bananas.
The severity of the diet depends on the disease of the pancreas. In the acute period, fasting is prescribed for three to five days; in case of exhaustion, parenteral and special enteral nutrition is used.
The most effective treatments
| Drug group | Brand names | Action |
| "Trasilol", Aprotex", "Ingiprol". | The drugs help suppress pancreatic secretions to reduce inflammation. They must be taken on the first day if acute pain occurs. | |
| “Phosphalugel”, “Gastrotsid”, “Alyumak”. | The products effectively neutralize hydrochloric acid. | |
| “Spazmonet”, “Drotaverine”, “Riabal”. | The drugs relieve spasm, helping to alleviate the condition. | |
| "Azithromycin", "Amoxiclav", "Azitrox". | The drugs help suppress the development of inflammation and prevent peritonitis and pancreatic necrosis. | |
| "Kuplaton", "Aprofen", "Chlorozin". | The drugs normalize motor activity and intestinal function. | |
| “Mikrazim”, “Festal”, “Creon”, “Panzinorm”. | Used to improve the digestion of proteins, fats and carbohydrates if the secretory function of the gland is impaired. | |
| A, B, C, D, E | If the outflow of pancreatic juice is disrupted, food digestion is impaired, and the person suffers from a lack of important microelements. Vitamin deficiency and anemia often develop. Vitamin complexes will help replenish the lack of essential substances in the body. |
To get rid of pain, you need to prepare a decoction:
- Grind 300 g of parsnips in a blender (or grind in a meat grinder), pour in 1 liter of milk.
- Put on fire, bring to a boil, let simmer for 15 minutes.
- The course of treatment is 2 days, it must be repeated 3 times with an interval of 10 days.
- On the first day, do an enema from the decoction. On the second day, prepare the same decoction, divide it into 4 doses and drink with an interval of 4 hours (do not eat anything on this day).
You can grind the rolled oats with a coffee grinder, pour it in a 1:2 ratio with chilled boiled water, and let it brew overnight. Half an hour before breakfast, mix thoroughly and eat the resulting mass.
Disease prevention
To prevent disease, first of all follow a diet:
- get rid of bad habits;
- fill your diet with cereals (buckwheat, oatmeal, barley);
- Eat less salty, spicy, fatty and sweet foods.
- Drink an infusion of potato flowers for two weeks:
- 3 tbsp. l. pour 400 ml of boiling water, let it brew for 3 hours, filter through a fine strainer.
- Take 100 ml before meals.
These are the main effective options for treating pancreas with folk remedies at home. It is important to try to change the method of treatment every few months, coordinating it with your doctor and the main course of medication.