A person can control everything: he can create the world with his own hands, making it amazing and beautiful, invent unthinkable things that change the consciousness of an entire generation and humanity. One only has to compare the level of medicine today and that of the last century. What about centuries! Even ten years ago this area left much to be desired.
But, as practice shows, not everything ingenious is the complex work of scientists. Each of us has a certain “magical” force - the subconscious. It can work wonders, literally pulling a person out of the other world with the help of an ordinary... pacifier (placebo) - a drug that has no medicinal properties. It is used instead of medicine to improve the patient's well-being. Have you heard anything about the placebo effect?
In this article we will figure out what the placebo effect is, talk about the pros and cons of this phenomenon, but first, let's dive into history.
Where did it all start?
This happened during World War II. In military hospitals there was an acute shortage of the painkiller - morphine, but the conditions did not allow stopping heavy operations, and then Henry Beecher decided to take a risky step: he had to operate on a seriously ill soldier, the lack of the drug threatened the onset of painful shock, and to prevent this from happening, he injected the wounded saline solution to the soldier, saying that it was morphine.
Beecher performed the operation as usual: removed the fragments and treated the wounds. Meanwhile, the wounded soldier acted as if he had actually received a dose of painkillers and felt only minor pain. After this incident, the surgeon continued his practice of replacing morphine with saline, and upon returning to the United States he began to study this phenomenon in more detail.
In 1955, Henry Beecher conducted a series of studies that proved the fact that a person is able to change physical reality with the power of thought. For the purity of the experiment, he compared the condition of not only patients who received pacifiers, but also those who were treated with medications. As a result, it turned out that the subjects who took the placebo felt much better than the other half of the patients studied.
Of course, this World War II story is not the first to point to the existence of the placebo effect. The Bible mentions miraculous healings; in particular, it talks about cases when the image of the Virgin Mary appeared to the sick, and they immediately recovered from all their ailments. Even in our time, after visiting holy places, people claim that their lives have changed for the better and they said goodbye to their illnesses.
Faith healing is not just about Christianity. The Indian guru Sathya Sai Baba, who is considered an incarnation of the deity, was known for healing the sick with his palms, which he first dipped into sacred ash. This healing method was practiced by the kings of England and France who reigned between the 4th and 9th centuries.
There are many similar stories in world practice that prove the incredible power of the subconscious. In the 1770s, Franz Anton Mesmer, a Viennese physician, based on Newton's teachings on the effects of earth's gravity on humans, concluded that there is a fluid in the body that can be controlled. He called it “animal magnetism” [D. Dispenza, 2016].
The essence of Mesmer's technique was as follows: he asked patients to look intently into his eyes, while he himself moved magnets around the body. This is how he brought the magnetic fluid into balance (then he did the same thing, only without magnets). During the entire process, patients began to twitch, some went into convulsions, it was believed that this condition indicated recovery.
Mesmer's follower was Armand-Marie-Jacques de Chastenet, an aristocrat from France. It caused “magnetic somnambulism” in people, a condition similar to sleepwalking. In this state, patients were immersed in deep thoughts and insights about their health, and when they emerged from it, they did not remember anything about what happened to them.
Later, James Braid, a Scottish surgeon, began to develop the topic of hypnotism and practice hypnosis treatment on his patients: he asked them to focus on a specific idea while looking at an object, while he himself manipulated their subconscious. He described his experiments in the book “Neurypnology”.
French neurologist Jean-Martin Charcot believed that people suffering from hysteria are susceptible to hypnosis. He used it not for treatment, but to study the symptoms of the disease. But there were those who supported James Braid's approach: Dr. Hippolyte Bernheim suggested to his patients during their trance that after the end of the hypnotic session they would feel better and all signs of illness would disappear.
Each of those who studied the influence of the subconscious on a person’s health used their own healing methods, and in fact, they were all able to help many patients, changing their ideas about the disease.
The technique of hypnotic suggestibility was used during the First and Second World Wars to treat soldiers for psychological trauma. Such techniques for working with the subconscious were so successful that doctors began to widely use them in practice. We are talking not only about hypnosis, but also about simple sugar pills that were given to patients as miracle cures [M. Shoifet, 2006].
In the late 1970s, it was proven that placebos trigger the production of endorphins - hormones of joy and pleasure that act no worse than drugs. John Levine, MD, gave pacifiers instead of pain medication to 40 dental patients after wisdom tooth removal. Patients felt significant relief, and when they were then given an antidote to morphine, they began to experience pain. It turns out that the placebo causes relief not only in the head, but also in the body, which indicates the production of endorphins.
An interesting study was conducted by Robert Ader, PhD, which helped him prove that the placebo effect is directly related to the development of a conditioned reflex. This reflex, which implies a connection between conditioned circumstances and natural functions, was discovered by Ivan Pavlov, a Russian physiologist. He proved it using the example of dogs: every time before feeding them, the scientist rang a bell. Later, when the dogs heard the bell ringing, they produced saliva. It turns out that the acquired reflex triggers the work of the subconscious [X. Koshtoyants, 1936].
Ader conducted his experiment on rats: he gave them sweet water, which contained cyclophosphamide, which causes abdominal pain. As a result, the rats not only suffered from pain, but also died from various infections, because this substance suppressed the immune system.
Animals began to avoid contact with sweet water, even water that did not contain this substance. But at the same time, when the scientist forcefully gave them ordinary sweet water, they also got sick and died: the water transmitted a signal to the nervous system to suppress the immune system. This experiment clearly showed that the placebo effect can lead not only to a positive, but also to a negative outcome [D. Dispenza, 2016].
Introduction
The medical history of the term “placebo” dates back to the 18th century, when placebos were described in Scotland as a means of treating patients who had failed active therapy while pleasing them (“placebo” is Latin for “I please”). 1 [1, 2]. In the 30s of the last century, the term “placebo group” was introduced into science to designate a control group receiving an inert effect when studying the effectiveness of medicinal drugs, devices or procedures [2], to distinguish those that actually act from those that act due to emotional factors associated with physical properties of the products (color, smell, tactile sensations, etc.). Today, a placebo is defined as an inactive substance or procedure that “does not have the intrinsic properties to produce the desired or expected result” [3], and the placebo effect is described as a psychobiological phenomenon that occurs in the human brain after taking a placebo, the procedure of which is accompanied by verbal statements (or other messages) about the clinical benefits of placebo treatment [4]. The occurrence of placebo effects has been described at almost all levels of human activity (neurobiological, physiological, psychological and social) [4, 5].
Expectations are recognized as the main psychological mechanism of placebo effects
human [5, 6]: the placebo effect occurs because the person expects it to occur. Already the appearance of the drug “tells” the patient what reaction awaits him: thus, instrumental procedures (acupuncture, injections) are perceived by patients as more effective compared to tablets [7], and expensive drugs are considered more effective [8].
The role of patients’ expectations in the occurrence of placebo effects is also confirmed by neuroscientists [9, 10]. A future event can influence various physiological functions by increasing or decreasing anxiety or by activating neural networks of the reward system [5]. There is evidence [11] about the participation in the formation of positive and negative expectations from the action of placebo of different neurochemical systems of the brain, the activation of which is noted in the regulation of various affective reactions.
Although placebo effects have been established for many pathological conditions, the therapeutic potential of placebos has been a subject of debate in the scientific community since the 1950s. Suffice it to recall the statement of H. Beecher [12] that 32.5% of the effect of any treatment depends solely on the “powerful” placebo effect, which has been repeatedly criticized [13] due to the lack of delimitation of placebo effects from spontaneous remission, a natural change in the course of the disease. disease, the effects of the influence of the doctor and the patient himself, additional interventions, etc. Modern studies of “pure” placebo effects rather confirm the thesis about the therapeutic nature of inert procedures, supported by expectations of a positive (negative) result, rather than refute them [14, 15]. Therefore, the attitude towards the use of placebo effects in medicine remains ambivalent: if clinicians generally consider the use of placebo justified, and its effects are beneficial for the treatment of diseases [16, 17], then in the academic environment and among supporters of evidence-based medicine, the more widespread opinion is that “ Treatment involves interventions that affect the patient's anatomy and physiology, and it is these changes that improve the patient's condition...” [18].
In the case of mental and drug addiction diseases, ambivalence towards placebos becomes especially obvious when the question arises about the legality of using psychotherapeutic methods of treating them. This often refers to their placebo nature, which means “low significance” [18], and less effectiveness (or ineffectiveness) compared to psychopharmacotherapy2. However, it is in the process of psychotherapy that the phenomenon of the placebo effect is taken into account and becomes an effective healing agent, as well as the subject of rigorous scientific research [19].
The motivation for writing this review was the need for a broader discussion of the therapeutic potential of the placebo effect in the treatment of addiction disorders. Today in Russian medicine, placebo effects are most often associated with the use of object-mediated psychotherapy procedures (“coding”), all kinds of placebo therapy (“binders”; oral administration of drugs that “cure” addiction) or frankly marginal methods of treating drug addiction diseases (flogging, frame 25, exorcism, etc.). However, we believe that the placebo effect can be used by doctors and in ethical clinical practice, reinforcing the effect of psychopharmaco- and psychotherapy. We believed that the discursive and popular science style of the article would demonstrate the power of the placebo effect and its role in psychotherapy for substance abuse disorders, especially in terms of the therapeutic and ethical implications of using the placebo effect.
The influence of the placebo effect as a general factor in psychotherapy in addiction medicine
Studies of pure placebo effects have produced mixed results. Thus, in one study [21], when comparing the use of placebo in 60 diseases with three approaches (active treatment, no treatment, and placebo), no significant therapeutic effect of placebo (except for pain and nausea) was found. A reanalysis of the same data with a slight change in methodology [14]—a comparison between active treatment and placebo—found that placebo and active treatment had comparable effect sizes, while relatively potent placebo was effective both on its own and and being part of a therapeutic regimen.
In the field of psychiatry, the results of several meta-analyses of research on major depressive disorder are noteworthy [22–26]. Some of them [22, 23] showed a relatively limited (statistically significant, but not clinically significant) advantage of antidepressants over placebo therapy. The positive therapeutic response of patients to placebo and psychopharmacotherapy depended on the initial severity of symptoms: the active substance was effective only in patients with high severity of depressive symptoms, and the magnitude of the placebo effect corresponded to 80% of all improvements in the drug group [22]. The authors attributed the relationship between the initial severity of symptoms and the effectiveness of antidepressants to a decrease in the sensitivity of the patients themselves to placebo, and not to an increase in the effectiveness of the medications. According to other data [24], the effectiveness of antidepressant treatment in patients with mild to moderate levels of symptoms compared to placebo was minimal or absent. Moreover, it was found [25] that 68% of the effect of antidepressants was the placebo effect. The results of the above studies gave rise to the question of whether antidepressant therapy is placebo therapy, how methodologically verified these meta-analyses are; is it possible to deprive patients with moderate depression of the opportunity to use pharmacotherapy [26]. However, in clinical terms, these data could mean that the effect of the drug is reinforced by the effect of the expectation of positive results and leads to better resolution of symptoms, and a moderate placebo effect can presumably be used in the treatment of a patient if its magnitude is comparable to the effect of the best available active therapy, thus Moreover, a placebo has no side effects and is more cost-effective than active treatment.
The stated pragmatic position underlies the patterns of placebo use by foreign general practitioners: for example, up to 56% of physicians in the United States have ever prescribed a placebo: a nonspecific drug (11%) or an “active” placebo, such as antibiotics (40%) [16]; 96% of doctors are confident that placebo has therapeutic effects, 40% believe that in some diseases it has a beneficial effect on physiological processes [17], and only 12% of therapists are categorically against the use of placebo in the clinic [17].
In the practice of psychotherapy, the placebo effect is considered as a general or nonspecific treatment factor, the influence of which on the result is at least 15% [20]. Interestingly, psychotherapists themselves sometimes equate the effects of psychotherapy with the placebo effect, since the results of corresponding well-designed double-blind studies were comparable [27]. In this case, the similarity of psychotherapy with methods of folk healing, shamanic and religious rituals is often pointed out [28]. It is argued that psychotherapy is a culturally embedded healing practice that arose in connection with the human ability to interpret the world, because comprehension through interpretation allows us to explain physical and mental illnesses [29]. In this sense, the type of therapy is not so important, but what is important is the extent to which it changes the patient’s vision, internal picture of the world and creates expectations
success or failure of treatment.
From a neuromorphological point of view, the placebo effect (expectations) and the effect of psychotherapy have a similar basis: they are possible only in the absence of gross disturbances in the activity of the prefrontal cortex of the brain, which is responsible for complex and executive cognitive functions (planning, outcome prediction, goal setting, decision making, abstract thinking, inhibition control, etc.) [5].
The expectancy effect significantly influences patient retention in the process of psychotherapy and specific therapeutic results. Positive expectations lead to a decrease in stress at the beginning of treatment, greater awareness of psychological processes, and an improvement in the patient’s condition even before the start of treatment (when making an appointment with a psychotherapist), while negative or low expectations, on the contrary, contribute to a general decrease in the effectiveness of psychotherapy [30]. At the same time, the coincidence of the patient’s expectations with the explanation of the future treatment process, which the psychotherapist gives at the first contact, significantly influences the patient’s further participation in treatment [31]. In addition, patients may come to a psychotherapist with ready-made expectations regarding how psychotherapy will be carried out and what its results may be: the higher the expectations, the more the patient is involved in the treatment process, the greater the effect can be seen during therapy and the “remoralization” effect is stronger [30-33]. An analogy can be drawn here with the phenomenon of “miracle” in religion. For example, in Russia, in the Vysotsky and Vladychny monasteries, miraculous copies of the icon of the Mother of God “Inexhaustible Chalice” are kept, which is famous for miracles of healing from alcohol and drug addiction, and Catholics recovering from alcoholism around the world offer prayers to Saint Martin of Tours (the Merciful) so that he will strengthen them on the path to sobriety.
In addiction medicine, the role of expectation was confirmed experimentally in a Finnish multicenter study [34] in outpatient treatment of addiction diseases. In a sample of 327 people, the influence of patients’ pre-treatment expectations on the effectiveness of treatment was assessed by indicators of patient retention in the 12-step treatment program, the number of days of sobriety according to six-month follow-up data, etc. A larger number of patients retained in the program and an increase in the percentage of days of sobriety during its implementation were are directly related to more positive expectations.
The role of positive expectations in drug treatment of patients was paradoxically confirmed by the ineffectiveness of behavioral therapy (BT) without placebo in a multicenter study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA, USA) [35]. Combinations of BT with pharmacotherapy for the treatment of alcohol dependence have been studied. Participants in a matched program who received BTX, a drug placebo, and regular follow-up with a drug treatment specialist had more days sober than participants who received BTX alone. Moreover, in terms of remission rates, BT was significantly inferior to the combination of placebo and doctor visits. The study authors concluded that the lower efficacy of BT in this case could be due to the nocebo effect (a negative non-specific effect of therapy [36]): since 8 of 9 patients were randomly assigned to take medication (2/3 received active treatment) , the majority were positively disposed to taking pills, while those sent to BT and left without “medicines” and additional attention from a narcologist were disappointed. A similar result was obtained in a study of the treatment of anxiety disorders, where taking a placebo in the acute phase of the disorder in addition to cognitive behavioral therapy (CBT) (which has proven effectiveness in treating anxiety) increased the effectiveness of treatment by 26% compared to patients receiving CBT alone [ 37].
Indirect confirmation of the data presented was obtained in a meta-analysis [38] of 47 studies of psychopharmacological drugs (naltrexone, acamprosate, sertraline, topiramate, etc.) for the treatment of alcohol dependence, schizophrenia and depression. It was found that the use of placebo significantly improved the condition of patients from the beginning to the end of the study. Moreover, this effect increases over time, and there is an increase in the frequency of placebo intake in patients with more severe disease. The latter is associated with subjective assessments of the symptoms of the disease, especially those related to alcoholic behavior, but not the desire for alcohol, the assessment of which is highly subjective.
The data presented are interesting in two aspects. First, they show that placebo effects are dynamic and can increase or decrease over time, which is important to consider when building therapeutic programs that “take advantage” of the placebo effect. Second, it appears that frequency of placebo use is associated with increased positive expectancy effects. Taking into account the prevalence of hidden drug administration in modern clinical trials, which makes it possible to eliminate the emotional component as much as possible, it can be assumed that an increase in the placebo effect will likely occur due to an increase in the frequency of contacts with the treating specialist. It is no coincidence that the placebo effect is characterized as the “interpersonal component of healing,” distinct from spontaneous natural healing and technical cures dependent on biologically active drugs and procedures [39]. In this sense, the placebo effect is much broader than the effect of taking an inert substance or procedure, equipped with an appropriate verbal or non-verbal design. The placebo effect is inherent in any therapeutic agent. And in its maintenance, a key role is played by the specialist helping the psychotherapist (in our case, a narcologist, psychotherapist, psychologist) as a person recognized by society and capable of forming positive expectations from treatment [6].
So, in the context of an emotional, trusting relationship, the psychotherapist has the opportunity to instill new hope in the patient and restore the patient's morale by offering a new perspective on problems and life situations, and new methods or procedures that allow the patient to experience the “experience of success” [40]. “Trivial” relief of symptoms and overcoming demoralization seems all the more important because the patient’s anxiety can trigger neurobiological mechanisms that lead to the formation of the nocebo effect - “the other side of the placebo” [5].
Practical application of the placebo effect and placebo therapy
Toxic placebo.
Forming expectations of a toxic reaction during placebo therapy with the drugs "torpedo" or "esperal" ("filers" in client and medical jargon), based on preliminary sensitization of the patient using, for example, disulfiram and a subsequent alcohol test, is common for the treatment of alcoholism in Russia . A toxic reaction against the background of disulfiram contributes to the appearance of the nocebo effect, creating in the patient an expectation of a negative result, which increases the level of anxiety due to the antagonistic effect of the cholecystokinergic system on the opioidergic system at different levels and the deactivation of m-opioids and D2-D3 dopamine receptors in the nucleus accumbens of the brain [15 ].
The nocebo effect in the process of sensitization is reinforced by psychotherapeutic influence - suggestion. This procedure for treating alcoholism is designated by the term “coding,” which is also commonly called “object-mediated psychotherapy” [41]3. Inspired prohibitive attitudes contribute to the patient’s development of persistent negative expectations regarding drinking alcohol as threatening his health or even life. Despite a number of data on the occurrence of long-term remissions in the treatment of alcohol dependence using methods of mediated psychotherapy [41], today their effectiveness is questioned, as well as the ethics of their use [42].
Behavioral psychotherapy with disulfiram.
Psychotherapy using disulfiram as a drug reinforcement of psychotherapeutic effects is best known in the treatment of Antabuse [43]. This method is empirically substantiated [44] and is not based on misleading the patient regarding the effect, duration, or danger of the drug, but on a clear contractual relationship between the patient, the doctor (psychotherapist) and his relatives, describing the rights and obligations of the parties to the contract, as well as possible sanctions and the consequences of failure to comply. The expectation of a toxic reaction is formed solely due to the doctor’s story and the presence of a “sanctions” list, with which the patient expresses consent by concluding a contract. Thus, the effectiveness of treatment here is determined by deterring use due to fear of consequences; by suggestion or self-hypnosis; participation in the therapeutic ritual and decision-making process (conscious decision to “stay sober” and control of desire) [45].
Opioid receptor antagonists (AORs).
In parallel with the observed reduction in “coding” and “filing” procedures, including through active administrative intervention, the opinion is gaining strength among narcologists that it is now “possible” to “encode” using long-acting opioid antagonists (for example, naltrexone). Despite recommendations on the combination of AOR with psychotherapy and drug counseling, in real practice AOR is used as a purely pharmacological method - a “pill” that “gets rid” of addiction and craving, allowing to achieve a reduction in the use of psychoactive substances (PAS) with minimal labor costs, and does not require the patient makes additional efforts to change his lifestyle and behavior. “AOR coders” actually give the patient a message: “The medicine will definitely help you, you will no longer have euphoria and desire, and you don’t need to do anything else.” However, while in the case of traditional “coding” such “motivation” could work, in the case of AOP it is useless due to the nature of these drugs.
With the administration of the opioid blocker naloxone [46], which inhibits the behavioral and neurological effects of placebo and placebo-induced responses in cortical systems, such as the rostral anterior cingulate cortex (associated with emotional regulation) - rACC, as well as the hypothalamus, periaqueductal gray matter (PAG), In the rostral ventromedial medulla oblongata, due to pharmacological blockade of the functioning of the prefrontal opioidergic system, a corresponding blockade of placebo effects occurs. The same “reversal” of the placebo effect, similar to the blockade of functional connections between the prefrontal areas as a result of their degeneration and the rest of the brain in Alzheimer's disease [5], probably occurs with the use of naltrexone [47]. Although AORs, not without reason [48], are positioned as reducing craving for alcohol or opioids (for example, in the “Point of Sobriety” program), the reduction in craving is, rather, a function of the loss of the feeling of pleasure from taking psychoactive substances with repeated exposure to stimuli associated with the use of psychoactive substances, and not the AOR effect. Thus, in one study [49], treatment-seeking patients with alcoholism received 50 mg of naltrexone or placebo for 7 days, and then underwent an experiment using alcohol stimuli with the introduction of an isotonic solution and alcohol on the 9th day. Surprisingly, patients in the experimental group reported increased craving in response to alcohol stimuli and increased subjective reactions to alcohol compared to the placebo group. In a randomized, double-blind, placebo-controlled trial [50] using a naloxone challenge and alcohol-related stimuli, blocking the endogenous opioid system did not reduce craving in alcohol-dependent patients compared with placebo.
Motivational interventions.
Motivational interventions aimed at increasing the motivation of patients with substance addictions to treatment [51] also actively use the placebo effect, in the sense that they concentrate on the formation of positive expectations from taking medications and concomitant psychotherapy and provide an anti-relapse effect, even in the absence of actual behavioral anti-relapse effects. Thus, short-term (no more than 1 session lasting 15-30 minutes) motivational interventions are more effective than structured and intensive CBT interventions for reducing alcohol consumption in the short term (6 months), apparently precisely due to the greater effect of expectations formed during a single session [52]. It is likely that a similar mechanism is involved here as when taking a placebo during the acute phase of an anxiety disorder [37], with the difference that the patient’s anxiety regarding treatment and the possibility of recovery is not modulated “medically”, but by the psychotherapist during the so-called conversation about change when the patient's attention is concentrated on formulations reflecting the possibility of change; the patient's arguments for change are identified and explored using specific techniques; the maladaptive formulations supporting the use of surfactants are revealed.
The goal of the intervention is to shift the balance in the patient's ambivalent attitude towards treatment, when part of the patient's personality expects positive results from treatment, and the other part seeks to maintain positive expectations from drinking alcohol. The results of neurobiological studies [53, 54] suggest that a change in the negative part of the set occurs due to a significant weakening of the activation of the reward zone in response to alcoholic stimuli or “turning off” the associative connection between taste stimuli and activation of the reward zone after providing the patient with information about the corresponding changes . When the patient's expectations for treatment are reinforced and reflected by the therapist, patients form opinions in favor of the necessary changes and shift the balance of decisions in favor of abstaining from alcohol use [55]. Patients of “motivation-focused” psychotherapists who received CBT and achieved positive results often reported that they were able to feel cooperation with the therapist, freedom in choosing the direction of work, feeling comfortable and trusting in the treatment process, contrary to their initial expectations from “highly structured” behavioral training ; patients with a negative treatment outcome did not experience such experiences [56].
So how does it work?
Before understanding how placebos work, let's go over the basic concepts again. Placebo is a substance that does not have obvious medicinal properties, which is used as an imitation of a medicinal drug in order to cure any ailment. These can be tablets, powders, liquid substances, injections. Translated from Latin, placebo means “I will like you.”
The placebo effect is the improvement of a patient’s condition with the help of a placebo, or more precisely, thanks to the patient’s belief that this substance, which is actually a dummy, will cure him.
Despite the fact that the placebo effect has been the subject of scientific research many times, it is impossible to say with certainty what the reasons for its influence on humans are.
There are several mechanisms that trigger the healing process after taking a placebo:
- Waiting for the patient. A person receives a “magic pill”, which, as the doctor assured, should cure him of his ailments. As a result, the patient enters a state of anticipation of the required effect, the level of stress hormones decreases, and the symptoms begin to seem less acute than they were before taking the medicine.
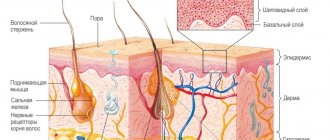
- The relationship between the placebo effect and the brain. Imaging of the human brain has shown that the placebo effect affects the nervous system, resulting in placebo analgesia (decreased pain sensitivity). This process involves parts of the spinal cord and brain stem, the nucleus accumbens and the amygdala. It has also been found that dopamine and opioid receptors increase activity in people while taking a placebo. These substances help reduce pain. Such changes occur in those areas of the brain that are affected by antidepressants [Med Special, 2019].
- Psychoneuroimmunology. This new direction of science explains the influence of brain activity on immunity. This is exactly what we talked about earlier when we described the experiment with mice and sweet water. In simple words, a person’s positive attitude can cure him of an illness.
- Development of mechanisms regulating health status. For example, a fever promotes the death of bacteria and viruses by increasing core temperature. It is no coincidence that doctors do not recommend reducing fever with medications if it is below 38 degrees. But at the same time, the brain itself “decides” when it will respond to the disease: for example, in the late stages of pregnancy with insufficient nutrition, fever does not occur, because high temperature can negatively affect the child.
This is what happens with the placebo effect: the brain “understands” that it does not need to respond to pain or other negative symptoms [Med Special, 2019].
As you can see, the placebo effect is explained from the point of view of psychology and medicine, but the attitude towards it in these areas of application is different, and the advisability of using the placebo effect still causes a lot of controversy. Let's figure out what's what.
The other side of placebo is nocebo
After taking an expensive drug, people prepare for significant side effects. This belief increases the harm from drugs and is called the nocebo effect.
The reverse placebo effect was studied by scientists from Germany, the USA and the UK in 2021. The results of the experiment were published in the journal Science.
49 volunteers participated in the study. The organizers asked the subjects to apply an anti-itch cream to their hands, which actually did not contain active ingredients.
Half of the volunteers were given an expensive-looking cream, and the other half were given a cream in a cheap package. The researchers warned that a side effect of the expensive cream could be increased sensitivity to pain.
Participants placed their hands on a device set to 45°C. Volunteers who applied the “expensive” cream to their hands rated the pain from the object twice as high. Participants in the experiment with the “cheap” cream stated that the pain subsided, while those who tested the “expensive” cream stated that the pain increased.
Placebo effect in psychology
The placebo effect is the result of an influence on our subconscious. The severity of the effect depends on how suggestible a person is. Placebo works great on extroverts and children; people with low self-esteem and neurotic types are even more affected by the placebo effect.
Placebos are successfully used in the treatment of psychosomatic disorders, because when the disease arises in the patient’s “head”, it is logical to involve psychology, and not real drugs. The main thing is to suggest that the pacifier is a miracle cure, otherwise such therapy will have the opposite effect due to the patient’s strong self-hypnosis (he may decide that the “medicine” will harm him).
As practice shows, insomnia, anxiety, and depression are well treated with pacifiers.
If we are talking about the treatment of psychological trauma, then the use of placebo does not always give positive results, especially if the patient is an introvert. The same story occurs in the treatment of personality disorder: as a rule, distrustful people with whom it is difficult to establish emotional contact are susceptible to this mental illness [G. Kibardin, 2018].
The main mechanism of placebo is to subjugate people's subconscious. This technique is used in various methods of alternative medicine (spells, removing the evil eye, damage, etc.) The effect of such “treatment” depends on the degree of suggestibility of a person and, as a rule, those who are in deep despair turn to such “healers” or during a period of psychological distress. You can suggest anything to a person when he is in an unstable mental state, and charlatans actively take advantage of this.
In fact, meditation and visualization also work on the placebo principle, and are perhaps one of the safest ways to work with the subconscious, if, of course, you know how to use these methods correctly.
In any case, it is important to understand that the placebo effect will only give a positive result when a person’s belief in recovery is especially strong. Once he is disappointed in the miraculousness of the drug, the body can trigger the reverse mechanism of action - nocebo.
Another interesting fact: our daily mentality determines our future. Scientists observed people over 50 years of age for more than 20 years and came to the conclusion that those who had a positive attitude towards approaching old age lived 7 years longer than those who had a negative attitude [Ya. S. Hamilton, 2010].
It has been proven that optimists cope with business and difficult situations more easily, get sick less, experience pain less often and recover faster, because emotions directly affect the functionality of a person’s internal organs.
Instead of output
A placebo is a first aid kit that is always with us and freely available. It doesn't always work yet, but scientists have not yet fully studied this phenomenon.
Who knows, perhaps in the future scientists will be able to understand the mechanism of how placebos work and create effective drugs that will work using the internal potential of the body.
Here's the test. Don't be lazy and test your knowledge. Good luck! PPS If the test is not displayed, wait a moment, it is loading.
Was there anything you didn’t like about this article, do you have anything to add, or did you find an error? Be sure to write about it in the comments. Not a single comment will be left unattended!
The placebo effect in medicine
According to research, in the United States, placebos are very often used to alleviate the condition of patients. In Germany in 2012, approximately 88% of doctors prescribed a placebo to their patients at least once, and in the UK, 97% of doctors used this approach to treatment in 2013. There is no exact data on how things are in Russia, but there is reason to believe that such a practice exists, because we have a “Hit List of Drugs” - a list of drugs whose effectiveness has not been proven [J. Howick, 2013].
The placebo effect is used in medicine to relieve a patient's pain when there are no effective drugs available for a specific case. It is also used when there is no confidence that a real medicine will help cope with the disease. It happens that a doctor prescribes an “empty” drug out of ignorance: he is confident in its effectiveness, although from a medical point of view the substance is completely useless.
But there are cases when a placebo is the only way to avoid conflict: the patient is sure that he needs medicine, although there is no direct indication. In this case, the doctor prescribes neutral substances to calm the person.
Doctors have repeatedly tried to use placebos in surgery, cardiology and other branches of medicine, and practice shows that pacifiers are good at relieving symptoms: nausea, headaches, etc. Studies have shown positive dynamics of recovery for people suffering from Parkinson's disease. It turns out that a placebo can also affect a person’s motor functions, including [A. Quattrone, G. Barbagallo, A. Cerasa, A. J. Stoessi, 2018].
A serious disadvantage of placebos is the unpredictability of the outcome of its use. Side effects depend on the patient's mood. There have been many recorded cases where neutral drugs, on the contrary, worsened a person’s condition, for example, causing toxicosis.
In some countries, it is prohibited to use placebos for medical purposes, because... All treatment is based on compliance with the principle of voluntary informed consent. If a doctor prescribes a pacifier to a patient, it means he deliberately cheated.
Plus, modern studies have shown that a person’s natural recovery and possible errors in the patient’s test results are often mistaken for the placebo effect [RAN, 2017].
The use of placebos in medicine is considered a gross violation if there is an effective drug, the benefits of which have been scientifically proven and it is known for sure that the placebo will not bring the desired effect.
It turns out that, despite the seemingly clear evidence of the benefits of the placebo effect, its use in medicine is a last resort when there are no other treatment options left.
Tricks of invention
The placebo effect has a long and rich history. It played a big role in the medicine of past centuries, when patients had to be treated with herbs and useless drugs.
The first scientific demonstration of the placebo effect occurred in 1799, when the British physician John Haygarth decided to test one of the “healing” drugs that were sold in shops at the time: expensive metal rods called “Perkins tractors” that supposedly drew diseases out of the body and helped to cope. with rheumatism thanks to a special alloy. Haygarth replaced the “healing” metal rods with wooden ones and, under the guise of “Perkins tractors,” offered them to subjects. Four out of five patients with rheumatic fever reported that their pain had improved.
We are happy to be deceived
Caricature of Elisha Perkins trying to cure a patient with his metal "tractors", 1754
Photo: Getty Images/Photo 12
The term itself first appeared in 1920 in an article in The Lancet. The placebo effect came into clinical practice after American anesthesiologist Henry C. Beecher noticed during World War II that some wounded people mistook regular saline as a painkiller.
Farm factor: the EAEU may have its own medical agency
A single regulator, an analogue of the European EMA, will speed up the registration of drugs in the member countries of the union
At Dr. Beecher's insistence, placebos became the basis for double-blind drug trials, in which one group of people was given the real drug and the other a sham drug. A drug was considered effective only if it was statistically superior to placebo.
Amazing Facts About the Placebo Effect
The very existence of the placebo effect is an amazing fact that not everyone can still wrap their head around. Many people understand this phenomenon as an opportunity to heal with the power of thought, but there are several more interesting nuances that are striking:
- The placebo effect works in animals: we have already given examples of studies that prove this. Here's another one: 34 dogs received medications for epilepsy, or rather, half were real medications, and half were dummies. Ultimately, 79% of dogs treated with placebo experienced a reduction in the number of seizures [K. Muñana, D. Zhang, E Patterson, 2010].
- Alcohol intoxication can occur from self-hypnosis: it turns out that you don’t have to drink alcohol to get drunk. It is enough to simply believe that the glass contains a strong drink and not lemonade, and your body will trigger the corresponding reaction, as in the placebo effect. This fact was proven by a simple experiment: a group of people were given tonic and lime under the guise of vodka, and a little later they were asked to take an IQ test. The test result showed that the mental abilities of the subjects decreased, because... they believed they were intoxicated [D. Decher, 2013].
- Most antidepressants act like placebos: these medications are now often prescribed by doctors to combat stress, nervous disorders and depression, but independent studies have proven that some of them do not provide any drug benefit, but cause a placebo effect [Boseley, 2008].
- Even if the patient finds out that he is taking a placebo, the result of the “treatment” will not change: it is generally accepted that a placebo is effective when a person thinks that it is a very effective medicine. But it has been proven that even if the patient finds out about the dummy, the positive dynamics of the “treatment” may not change for the worse [Jha, 2010].
- The results of patients taking placebos differ depending on their cultural background: in America, people believe in the healing power of pills because... There is a powerful propaganda of medicines there. Placebo trials for the treatment of stomach ulcers showed good results in Germany, but in Brazil this approach in medicine did not produce the expected effect. It turns out that the patient’s cultural background, his faith, fears and beliefs have a strong impact on his subconscious.
- Two different infections can trigger the placebo effect: scientists divided a group of asthma patients into two parts. They infected one half of the subjects with parasites, and convinced the rest that they were also infected with them, assuring them of the effectiveness of this approach in treating asthma. As a result, both groups of subjects improved their health, and many patients refused to be treated for parasites after the experiment, because believed that they helped them fight asthma. This fact explains why we are willing to do reckless things for the sake of our health.
- A placebo can have a negative effect: there is another side to the coin. If the patient expects side effects or worsening of the condition from the pacifier, such an attitude will lead to negative consequences. In 1962, an experiment was conducted in Japan: children rubbed poison ivy leaves on their hand and were told that it was a harmless plant, and rubbed their other hand with sakura leaves and claimed that it was poison ivy. As a result, children developed a rash on the hand that was rubbed with sakura. This is how a pre-established negative attitude influences the situation.
- Color affects the subconscious: scientists have proven that the result of using a placebo depends on the color of the “magic” pill. Yellow pills have a positive effect in the treatment of depression, red pills increase tone, and green pills relieve symptoms of stomach ulcers.
- Imitation of surgical interventions also gives a placebo effect: if a person who is indicated for an operation is told that it was performed, the body will begin to recover due to self-hypnosis. This fact has also been proven by scientific experiment [D. Decher, 2013].
Can you imagine the power our subconscious has?! But, as you see, a person’s faith, beliefs or fear can either cure him or destroy him. It all depends on what he is in the mood for and how much he can control his thoughts. From placebo to nocebo – one step.
Shape matters
Placebo tablets affect patients differently depending on the color, size, shape and type of coating. Manchester scientists came to this conclusion after two years of research for the Sandoz pharmaceutical plant.
Patients perceive blue pills as sedative, and pink pills as stimulating. The larger the tablet, the better the effect on a person. Bitter placebos treat more effectively than sweet placebos, while capsules are more effective than tablets. Injections are perceived by patients as the most powerful remedy.
The Placebo Effect: Real Life Examples
Janice Schoenfeld, a 46-year-old designer from California, suffered from depression since childhood, but she did not try to get rid of her illness until she saw an advertisement that the Neuropsychiatric Institute of the University of California at Los Angeles was planning to test a new drug for depression and was looking for it. volunteers. Janice decided that this was her chance to recover and took part in the experiment.
She was handed a bottle of pills, and at the same time she was aware that some of the subjects would receive the real medicine, and some would receive a placebo. Soon after taking the pills, Janice began to feel better than ever, and there were even side effects from taking the medicine (nausea), so she was sure that she was taking real drugs. Imagine Janice’s surprise when the doctor said that she had been taking a placebo all this time.
In 1957, Bruno Klopfer, a psychologist at the same institute where Janice's experiment took place, published an article about his patient Mr. Wright. He had cancer of the lymph glands: huge tumors that did not respond to standard treatments.
The patient himself believed in a cure, unlike his attending physician. Wright learned that tests were being conducted on the experimental drug krebiozen, he voluntarily became a study subject, although according to the rules he had no right to do so, because. his condition was very bad.
After receiving the injection, within a couple of days he began to feel much better, and the doctor noted that his tumors began to shrink. After some time, he was discharged from the hospital, because... he was completely healthy.
Soon the newspapers published an article that Krebiozen was a fake. Wright read it and went back to the hospital: the tumors had returned. The doctor realized that the personal result was achieved thanks to the placebo effect and, realizing that this was the only chance to get him back on his feet, he told the patient that real Krebiozen would soon be admitted to the hospital. This news has already had a positive effect on Wright's condition.
A few days later he received his injection again, but it was simple distilled water (which, of course, he did not know about). The tumors disappeared, the patient went home, but a repeated article about the ineffectiveness of Krebiozen killed him. After reading it, Wright no longer believed in his healing, and literally three days later he died.
In the late 1950s, researchers from Kansas City and Seattle conducted the following experiment: they divided heart patients into two groups. The first group underwent heart surgery, and the other group simulated such an operation: surgeons made small incisions in their chests, which they simply stitched up without performing any other surgical interventions.
The results were astounding: 67% of patients who underwent real surgery began to feel less pain, and among the other half of the subjects, 83% of the patients did. It turns out that faith in healing turned out to be stronger than real operations [D. Dispenza, 2016].
For what purposes is placebo used: examples
It would be strange if people did not use the healing bonus from the body in their lives. Where is the placebo effect used and when is it appropriate?
In pharmacotherapy
Treating a person with a placebo in medicine is considered unethical . After all, prescribing to a patient any drugs that have nothing in common with drugs in the usual sense is deception.
According to recommendations from international and national organizations, physicians should not use placebos as part of therapy. Especially for the treatment of serious diseases, such as autoimmune, infectious and oncological diseases.
Oxford and Southampton University conducted a joint study in which they found that 97% of British doctors had given a placebo to patients at least once in their medical practice.
Despite the absence of indications indicating the need to use a placebo, doctors sometimes prescribe a dummy drug to a certain circle of patients. For example, to check whether drug treatment is required or whether psychotherapy will be sufficient.
This technique is especially relevant for suggestible people, hypochondriacs (people who are overly concerned about their health) or for people with anxiety disorders.
This way you can avoid the use of various medications . By the way, homeopathy is based on the same placebo effect.
Interesting Obecalp tablets are produced in the USA (just read the name backwards to understand how the medicine works). The tablets consist of sugar and are given to children to “cure laziness.”
The placebo effect works best for psychosomatic illnesses. It activates neurological and mental mechanisms, thereby increasing the activity of the prefrontal cortex, nucleus accumbens and pleasure center.
The work of these areas contributes to the production of substances that reduce anxiety and fear, as well as have a relaxing effect. A positive emotional state can help a person recover, but does not guarantee it.
Placebos are also used to relieve pain when the desired drug is not available. Well, placebos can also be used unknowingly, for example, if the doctor thinks that the drug is effective, but in fact it does not work.
In narcology
The placebo effect is also used in addiction medicine. Coding and stitching exploit the placebo effect.
The authority and confidence of the doctor, supported by tablets, ampoules and various procedures, help a person to believe in the effectiveness of treatment. Ignorance and lack of education also play a major role in addiction treatment.
At the end of therapy, the patient is sure that if he abuses alcohol or drugs again, he will die.
In order to convince the patient of the effectiveness of treatment and instill fear in him, the doctor uses a variety of methods during therapy.
In addition to pills, ampoules and hypnosis, a contract can be used, according to which the patient bears all responsibility for a possible breakdown. Simulated surgeries are also often used to mislead patients.
During the procedure, the doctor may use a method based on provocation . A solution of nicotinic acid or magnesium sulfate is injected intravenously, and they, in turn, cause fever and suffocation. Then the patient drinks alcohol, and it begins to seem to him that the fever and suffocation are caused by alcohol. What do we get as a result? The fear of death intensifies.
In clinical trials
Why else do you need a placebo? Most often it is used in clinical trials as a control drug, that is, to test the effectiveness of new drugs . New drugs that pharmaceutical companies create should work better than placebos. How are the tests carried out?
The subjects are divided into two groups: the first group is given an experimental drug, the other group is given a placebo. The health status of the first group must not only improve, but be significantly better than that of the second, in order for the drug to be considered therapeutic. That is, if a medicine shows itself to be worse or not much better than a placebo, then it is sent for revision.
A clinical trial is called “blind, placebo-controlled” if only the attending physician knows who is receiving what.
But the most reliable is considered to be a “double-blind, placebo-controlled study . Its essence is that neither the staff nor the subjects know who receives the placebo and who receives the drug. It is considered the most reliable, since the doctor will be more convincing, plus the doctor will not be able to accidentally reveal the secret to the patient through facial expressions or gestures.
All these studies can also be randomized , that is, patients are randomly selected into groups.
Recently, there have been increasing proposals for placebo-controlled studies to include three groups . The first two would receive a placebo and an experimental drug, while the third would receive nothing. What is it for? To separate the placebo effect from the real effect (self-healing of the body) and other unaccounted factors.
Summarize
The human subconscious is an amazing thing, it can heal him, you just need to use the trigger mechanism - a placebo. Many people say that faith is the best medicine. It is not for nothing that many religious scriptures contain examples of miraculous recovery.
In fact, a positive attitude and confidence that the treatment will have a positive effect play a huge role. Negative thoughts trigger irreversible processes in the body that destroy it from the inside, and even the most advanced medications will not help here, not to mention placebos.
If you still don’t believe in the power of thought and the subconscious, or simply haven’t wondered what the human brain is capable of, we recommend taking our online Cognitive Science program, where in a few weeks you will learn how to apply more than 20 thinking techniques that will change the way you think about your own abilities.
The topic of the placebo effect was perfectly covered by Joe Dispenza in his book “Be Your Own Placebo: How to Harness the Power of the Subconscious Mind for Health and Prosperity.” In it you will find several more real stories, descriptions of experiments and a detailed scientific explanation of why pacifiers heal, but, on the contrary, can kill someone. The future is in the hands of those who are optimistic, confident, believe in the best and do not give free rein to negative thoughts. Draw conclusions, or better yet, smile right now - heal your body with a positive attitude. Be healthy!
We also invite you to take a short survey:
We also recommend reading:
- Storytelling
- What is consciousness?
- Rosenhan's experiment. One step from health to madness
- The power of thought: scientific facts and research
- Aromatherapy: your tone, health, peace of mind
- Seven Visualization Techniques
- 7 popular pseudosciences
- Psychoimmunology – strengthening the immune system through mental health!
- Anniversary syndrome: what is it and how to avoid it
- Sleeper effect
- The Rosenthal effect or how to wisely lead a team
Key words:1Cognitive science