Home » Articles » How to give an injection at home: detailed instructions
During the treatment process, patients are often faced with the need to schedule a course of injections. Of course, they immediately wonder how much an intramuscular injection at home costs, but only a specialist can give the exact price, focusing on the type of drug, injection and duration of the course.
How to choose a syringe and needle for an injection in the buttock
The main thing you need to know when choosing a syringe for injection is that the volume of the instrument should not exceed the amount of the drug administered:
- for children – 2 ml;
- for adults – 5 ml (very rarely 10 ml).
Injections with a volume of more than 10 ml are not given into muscle tissue. A large amount of medicine is not able to quickly dissolve and spread throughout the body. This condition can lead to purulent abscesses.
To prevent the injection of the drug from being too deep, the most suitable needle length is considered to be 4–6 cm. This will also help not to catch the walls of capillaries and nerve endings,
Tips, notes, life hacks
If the injection is painful, inject the medicine slowly. It seems that the faster, the sooner a person will be exhausted, but in fact, a slow introduction is more comfortable. Average speed: 1 ml per 10 seconds.
Don’t be afraid to treat the ampoule, hands or skin with an antiseptic once again. Here it is better to overwork than to underwork.
If you need to change needles after drawing up medication, do not remove the cap from the new one until you install it on the syringe. Otherwise, you can inject yourself. For the same reason, never try to cap a needle if you have already removed it.
If you don't know how hard to stick a needle, at least practice on chicken fillet. Just to understand that it's not scary.
Preparing for intramuscular injection
The results of the procedure depend on a number of simple manipulations:
- Inspect the ampoule with the medicine for its integrity, and also check the expiration date of the drug.
- Collect all the medicine at the bottom of the ampoule. To do this, you will need to lightly shake the ampoule 1-2 times.
- Use a special file (supplied with the preparation) to file the upper part of the glass flask. Usually the incision site is marked with a colored rim.
- Break off the sawn tip of the ampoule. For safety, it is better to place the cone in a napkin so as not to get hurt when opening the glass vial.
- Release the syringe needle from the protective cap and immerse it in the medicinal liquid. Pull the handle of the instrument towards you and draw out the medicine.
When the syringe is filled with liquid, you need to tap it a little with your finger. This will help to collect all the air bubbles and, by gently pressing the piston, bring them out. After this, you can give the injection.
If the main medicinal substance is in powder form, it is diluted in a special solution (indicated in the instructions).
This is done as follows:
- remove the protective metal cap from the bottle;
- using a needle and syringe, inject the required amount of solution into the vial of powder;
- shake thoroughly;
- turn the bottle over, pierce the cap and collect the medicine in the syringe.
When the lid is pierced, the needle becomes dull. To make the injection less painful and to maintain sterility, it is better to replace the needle with a new one before injection.
Advantages
- The drugs dissolve very slowly, up to 12 months.
- They have a local effect on all joint tissues.
- Almost do not enter the systemic circulation and do not affect the functioning of internal organs.
- Thanks to the previous point, they can be used in patients with severe concomitant pathologies, when treatment with other methods is unacceptable.
- Intra-articular injections help avoid surgery.
- After the procedure, no rehabilitation is required; the doctor can only apply a tight bandage and warn against excessive physical exertion.
Instructions for performing an injection in the buttock
It is not difficult to give an injection to an adult or children. The main thing is to follow the sequence of actions and know all the nuances of the procedure.
Technique for injections in adults
The following scheme will help you give the injection as painlessly as possible.
- Place the patient on a flat surface face down and free the upper part of the buttock from clothing.
- Wipe the injection site with a cotton swab soaked in alcohol.
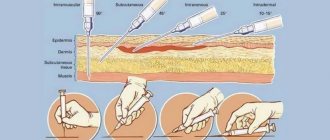
- You need to hold the syringe with your right hand and stretch the skin in the area of the upcoming injection with your left.
- The needle should be inserted three-quarters of the way into the muscle at an angle of 90 degrees. The hand movement should be confident and fast.
- Inject the medicinal solution by slowly pressing on the syringe plunger and sharply remove the needle from the buttock, covering the injured area with alcohol-soaked cotton wool.
It is important to understand that rapid administration of the medication makes the procedure very painful and can cause the formation of lumps and lumps.
How to properly give an injection to a child
Children are heavier than adults to tolerate injections that are given intramuscularly.
To make the unpleasant procedure as easy as possible for a small organism, several basic nuances should be taken into account:
- When preparing the injection site, the skin should not be stretched (as in adults), but rather folded.
- Massage the desired area of the muscle well.
- Insert the needle at an angle of 45 degrees.
The rest of the manipulations are the same as for an adult.
Intramuscular injections are not recommended to be injected into the same place more than 2 times a week. The buttocks must be alternated, and the distance between skin punctures should be 1-2 cm. This will avoid compaction in the muscle tissue and pain.
How to inject yourself
There are situations when there is no one to give an intramuscular injection and you have to carry out this manipulation yourself. Injecting yourself is not so convenient, but you can learn how to do a medical procedure if you know the basic nuances.
- Choose the right pose. Usually they stand in front of a mirror, relaxing the side in which the injection will be given (bend the leg at the knees, resting on the other limb). You can give injections while lying down, but it is recommended to lie on your side.
- Confidently insert the needle. To do this, you need to take the syringe with your right hand and with a sharp movement inject into a previously prepared place on the buttock. Slowly squeeze out the medicine.
- Complete the procedure correctly. Remove the needle sharply and treat the puncture area with cotton wool and alcohol (vodka). Massage thoroughly.
Important! It is important not to give injections if the skin on the upper part of the gluteal muscle is covered with acne or other damage. To avoid infection, it is recommended to inject the medicine into the muscle on the thigh.
Call a nurse now
Call a doctor at home
You can call a doctor online, we will call you back to clarify the procedure and arrival time.
Even a simple consultation or routine examination requires one thing - time. Patients have to set aside several hours and travel specifically to a clinic or city hospital, not to mention full-scale procedures that must be performed regularly.
A fast and affordable alternative is a doctor at home from Doctor Mos! Our specialists will arrive at a time that is convenient for you, and then carry out comprehensive work - from diagnostics to professional medical care.
If an injection in the buttock is given incorrectly - complications
Incorrectly given injections can provoke serious consequences:
- vascular damage, which is accompanied by hematomas and abscesses;
- development of compactions and bumps due to poor absorption of the drug;
- inflammation in soft tissues as a result of infection;
- fat or air embolism (air entering a capillary).
If after the injection your buttock hurts, your leg goes numb, or an allergic reaction occurs (redness, swelling), we are talking about improper administration of the medicine. To prevent complications, it is recommended to consult a doctor.
What happens if you give an injection with air?
A small amount of air entering the muscle or intercellular space during an injection is not dangerous. As a result, an air infiltrate (compaction, bumps) may occur, which hurts and becomes inflamed. To alleviate the condition, draw iodine nets, apply soda compresses, and cabbage leaves.
If air gets into the capillary, the small vessel dies. This is not harmful to health, but still refers to the undesirable consequences of an injection with air.
Injecting the buttock yourself is not difficult if you follow all the rules of the specific procedure. If the recommendations are not followed, lumps and lumps may form, which may be accompanied by infection and inflammation. It is important to pay attention to negative deviations in time to prevent the formation of abscesses.
PRP therapy
PRP stands for platelet-rich plasma. Platrlet rich plasma. Platelets are responsible for the formation of blood clots - blood clots that can clog damaged blood vessels. Platelets also actively participate in the processes of cleansing wounds of unnecessary proteins and stimulate the activity of fibroblasts. The latter are responsible for the production of collagen and elastin, which are the basis of connective tissue.
PRP therapy is injections for joint pain that have a number of advantages:
- do not cause allergies or side effects;
- rarely lead to the development of complications; (hormones);
- vitamins;
- do not transmit infection..
These advantages are due to the use of the patient’s own blood, which is completely compatible with body tissues. To improve the effect, plasma administration can be combined with hyaluronic acid preparations.
How to choose an antibiotic
In case of an acute viral disease, an antibiotic is prescribed by a doctor, referring to the results of laboratory tests.
To select the correct drug you need:
- determine the properties and type of infectious agent;
- choose a course of treatment and calculate the dose of the drug;
- select a set of medications for microorganisms that are difficult to treat;
- when the pathogen has not been identified, it is worth using a broad-spectrum antibiotic, and after bacteriological tests, use a drug with a narrow spectrum of influence.
To eliminate negative side effects, when prescribing drug treatment, the patient’s age, general condition, and severe symptoms are taken into account.
Hydroxychloroquine - treatment regimen for coronavirus
This antimalarial drug is distinguished by its ability to penetrate endosomes. These structures are located directly inside the cells where the SARS-CoV-2 virus penetrates. Presumably, the components of the drug can act on coronavirus in combination with an antibiotic.
However, during an analysis of the course of the disease in patients taking Hydroxychloroquine and Azithromycin, an incidence of death was observed. In this regard, WHO recommended not to use antimalarial drugs in COVID-19 treatment protocols. In the recommendations of the ministries of health of individual countries, Hydroxychloroquine is still included in the lists of recommended medicines and is included in treatment regimens for coronavirus.
Treatment regimen for coronavirus in humans - WHO recommendations
As we learned more about the virus, experts continually developed treatments for COVID-19. Assessing the effectiveness of individual measures, based on the data received, WHO periodically updates the recommendations issued. Since the outbreak of infection in China, the treatment regimen for coronavirus in humans has undergone changes more than once, but today there is no clear, effective algorithm for treating the infectious disease.
According to statistics, in most cases the disease is mild or asymptomatic. Only in 14% of patients the pathology becomes severe. The coronavirus treatment regimen for such patients is developed individually.
In general, the recommendations boil down to the following:
- Avoiding contact of those infected with COVID-19 with others.
- Use of antiviral agents.
- Prescribing antibiotics in case of complications and development of pneumonia.
- Oxygen support for patients in case of respiratory failure.
- Prevention of the development of multiple organ failure.
Treating coronavirus at home: what is the danger?
The main risk of home treatment for COVID-19 is isolation from a medical facility and, as a result, the danger of not getting help if it gets worse. Therefore, when treating at home, it is very important to carefully assess your condition.
An important indicator here is the most common symptom of coronavirus - temperature. If it stays at 38 degrees or higher for more than 4 days, this is a serious signal about a possible severe course of the disease. According to Ilya Varlamov, “if the temperature does not subside on the 5th day, you need to do a CT scan and see what’s in the lungs.”
Another important indicator is blood saturation. If possible, it makes sense to purchase a pulse oximeter device - it is compact and allows you to easily measure the level of oxygen in the blood.
In any case, you need to carefully monitor the external manifestations of lung dysfunction: shortness of breath, difficulty breathing.
Antiviral drugs
No specific antiviral drug has been developed targeting covid-19. But pharmacological research is being carried out to create it. Many pathogenic microorganisms contain similar genetic information. They are based on DNA or RNA.
Therefore, some drugs aimed at other viruses can help in diluting covid-19.
Doctors often prescribe a combination of lopinavir and ritonavir, but no precise data on positive dynamics have been found.
It is believed that these drugs help fight the disease, but basically the human immune system copes on its own. They are designed to speed up this process by eliminating parts of the pathogenic microorganism from the bloodstream and tissues. Antiviral drugs are prescribed for a limited course. Usually it is no more than 10 days. But the doctor can extend their use to 2 weeks.
Antiviral medications for coronavirus are not always prescribed. They are required only in moderate and severe pathology. If the patient has a mild stage, only symptomatic therapy is sufficient. It is important to remember that many antiviral medications have side effects. Therefore, during treatment and after its completion, laboratory tests of blood and urine are taken. If deviations occur, additional therapy will be required for recovery.
The Importance of Blood Thinning
Coronavirus is dangerous due to complications for the cardiovascular system. Therefore, the treatment regimen for coronavirus in people with moderate or severe pathology necessarily includes Heparin.
After its use, the following pharmacological action is formed:
- preventing the formation of clots from platelets and clotting factors;
- blood flow stabilization;
- no blockage of blood vessels or capillaries.
When a coronavirus infection develops, Heparin is injected into the abdominal area. This benefits the patient as the effect develops gradually and there is no risk of sudden bleeding. The effect of the drug is prolonged and fewer injections are required. The syringe is equipped with a thin, long needle, so pain during injection is reduced.
Heparin is used in a strict dosage, otherwise multiple side effects may develop, including intracavitary hemorrhage.
The drug should not be used with other anticoagulants, cardiac glycosides, tetracyclines, penicillins.
It is used in a strictly limited dosage and course of treatment. Typically, a decrease in blood clotting is observed within 12 hours, then a second injection is required.
Antibiotics for coronavirus from pneumonia - treatment regimens
Antibacterial drugs are used to treat moderate and severe forms of coronavirus infection. Antibiotics help eliminate changes in the lung tissue that occur against the background of lung damage by microbes, with pneumonia. According to established WHO guidelines, antibiotics are recommended for all critically ill patients undergoing invasive ventilation.
At the same time, the most popular antibiotic is Azithromycin, for coronavirus, the treatment regimen for which is as follows:
1. Average severity of the disease:
- Mefloquine + Azithromycin + Baricitinib;
- Hydroxychloroquine + Azithromycin + Olokizumab.
2. Severe coronavirus infection:
- Mefloquine + Azithromycin + Tocilizumab/Sarilumab;
- Lopinavir/Ritonavir + Hydroxychloroquine + Tocilizumab/Sarilumab.