ATTENTION! From December 2021, a new medical center will open for you at the address: Dmitrovskoye Shosse, 81 (5 min. walk from Selegerskaya metro station), where you can receive a wide range of medical services, including CT (computer tomography).
- home
- Surgery
- Hidradenitis surgery
A medical doctor in North-Eastern Administrative District of Moscow performs an operation to remove hidradenitis.
Hidradenitis suppurativa is a disease accompanied by inflammation of the apocrine sweat glands due to infection with a staphylococcal microorganism. The axillary region is most often affected, but inflammation of the groin, periumbilical, anus, and near the external genitalia also occurs.
Doctors surgeons
Dzhadzhiev Andrey Borisovich Surgeon
Cost of admission 1500
₽
Make an appointment
Marynich Alexander Alexandrovich Vascular surgeon, phlebologist, angiologist
Cost of admission 1500
₽
Make an appointment
Myshlyaev Anton Vsevolodovich Surgeon coloproctologist
Cost of admission 2000
₽
Make an appointment
Folk remedies
Photo: cadencehealth.com.au
It is difficult for a non-specialist to determine the required composition of the drug, taking into account the stage of inflammation, so the use of local remedies often results in the progression of the purulent process and the occurrence of complications. When using traditional recipes, it is better to limit yourself to safer decoctions for oral administration.
For hidradenitis, a herbal mixture of eucalyptus and plantain leaves, calendula and elderberry flowers is effective. All plants are taken in the same proportions. One glass of raw materials is crushed and filled with water, the mixture is brought to a boil over low heat. The medicine is taken several times a day after infusion in a dark place. For taste, you can add a teaspoon of honey to the broth. This folk remedy has anti-inflammatory properties and improves immunity.
To increase the body's defenses, rose hip tea, cranberry juice, vitamin compotes, sea buckthorn infusion and a decoction of bay leaves are also useful. The use of traditional methods is allowed only after consultation with a doctor, and does not replace surgical operations and treatment with official medicine.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Method of operation
Surgery to remove hidradenitis under the arm involves a surgical technique. Surgeons from our clinic practice two main methods:
- autopsy - occurs by resection of the skin of the abscess, followed by evacuation of pus. The wound remains open and heals naturally;
- excision is a radical method in which the sweat gland is completely removed with suppuration to the extent of healthy tissue. The wound is sutured after surgery, and if a large amount of tissue is removed, skin grafting may be necessary.
The patient is operated on under local anesthesia for 30-40 minutes. In advanced cases and with multiple spread of abscesses, it may be necessary to treat hidradenitis in a hospital setting, with removal of the inflamed area under general anesthesia.
Preparation, diagnostics
Upon examination, the surgeon differentiates hidradenitis from other purulent lesions of the skin and soft tissues and determines the stage of the disease. For adequate antibiotic therapy, bacterial culture of purulent discharge is carried out to determine microflora and sensitivity to antibiotics. For prolonged and recurrent pathologies, an immunogram is prescribed. Surgical intervention does not require specific preparation. All you need to do is pass a standard package of tests. Thanks to our own laboratory, the answers will be ready within an hour, after which the surgeon will carry out the treatment.
Causes and symptoms of hidradenitis development
Factors that provoke the development of the disease may include:
- tissue infection due to cuts and injuries;
- insufficient compliance with hygiene rules;
- low immunity;
- diabetes;
- pathology of the sweat glands.
Inflammation is provoked by an infection of streptococcus aureus and steptophylococcus, which penetrates through the sweat ducts and the lymphatic system to the fatty tissue.
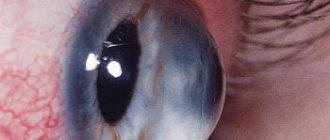
Hidradenitis is characterized by itching with the formation of a hard swelling up to 2 cm in size. The tumor quickly increases in size, and pain is felt. The skin takes on a red tint, with further softening of the tissue and the formation of a fistula with discharged pus, often with blood. The patient's condition worsens, headache and fever appear.
Specialists at the KDS Clinic will perform the operation as quickly as possible. The cost of our services for the removal of hidradenitis in the region and in Moscow is below average, therefore available to a wide range of the population.
Chronic hidradenitis suppurativa (HSS) is a multifactorial disease with a chronic relapsing course [1]. Apocrine glands, involved in the pathological process in CHG, begin to function in puberty. Previously, some glands, for example in the areola, were considered modified apocrine glands; now it is recognized that all of them are true apocrines [2].
The exact pathogenetic mechanism of the disease remains unclear. Possible causes of CHG are associated with genetic, environmental, endocrine and microbiological factors. Several studies have indicated higher incidence rates in smokers (70–90%), and have also noted a correlation between body mass index and the severity of CHG. Also, some bacteria and their associations isolated from lesions are considered one of the causes of the inflammatory process. However, CHG is not a classic infectious disease, since it is still not clear what role bacteria play in pathogenesis: primary or secondary [3]. Currently, the number of scientific publications on this aspect of the disease is growing.
The histological picture of CHG varies. Thus, according to G. Jemec et al. [4], in a study of 60 samples of biopsy material, only 17 of them showed follicular occlusion, while in the axillary region apocrine glands were involved in the inflammatory process more often than in the inguinal region. Other biopsy studies have shown the presence of occlusion of the hair follicle due to hyperkeratinization, which led to its expansion, the formation of nodules or cysts and, ultimately, tissue rupture with the formation of sinuses, fistulas and fibrosis [5]. Perhaps the heterogeneity of the histological picture causes difficulties in the treatment of CHG.
Dermatologists and surgeons usually make a diagnosis of CHG based on the characteristic localization and clinical symptoms, but, unfortunately, often with a long diagnostic delay, when the disease already reaches III-IV severity. On average, the time from the onset of the disease to diagnosis takes about 7 years [6]. It has been established that patients turn to doctors of various specialties (surgeons, dermatologists, urologists, proctologists, immunologists, homeopaths), self-medicate for a long time, which also contributes to late diagnosis and delay of timely adequate treatment, and, ultimately, aggravation of the clinical picture and deterioration quality of life.
There are three main diagnostic criteria for CHG [7]:
1) typical anatomical localization of foci of inflammation: axillary and inguinal areas (symmetrical lesions);
2) typical clinical symptoms: moderate pain, deep nodes, conglomerates of nodes, “heavy” tissue infiltration, abscess formation, fistula tracts with purulent discharge, fibrosis, scars;
3) recurrence and chronic course.
Additional criteria include hereditary predisposition, the presence of CHG in relatives; pilonoid sinus, a history of suppurating sacrococcygeal cyst; metabolic syndrome, hyperhidrosis, smoking. A. Jørgensen et al. [8] studied the clinical presentation of patients with different body mass index (BMI) and found phenotypic heterogeneity in individuals with high and low BMI. The authors emphasized that these two phenotypes may reflect different etiologies and prognosis and, therefore, require different approaches to management tactics.
To facilitate the assessment of the severity of the clinical picture and the severity of the process, various rating scales are used around the world to help the attending physician choose the optimal treatment algorithm and tactics for managing a patient with hidradenitis.
In existing European clinical guidelines [7], the choice of a particular treatment method is based on a staged approach, taking into account the severity of the disease according to H. Hurley. Later, other rating scales were proposed that allow the doctor to determine the indications for a therapeutic or surgical method of treating a given disease, depending on the severity of the clinical picture.
In accordance with the classification according to H. Hurley, there are three degrees of severity of CHG [9]:
— I degree of severity is characterized by the formation of one or several painless or slightly painful isolated nodes and/or abscesses that are not prone to acute progression and suppuration; fistula formation and scarring are absent;
- II degree of severity - intensification of the inflammatory process limited to one localization, recurrent nodes and abscesses are delimited from each other, do not merge, open up, form fistulous tracts with purulent-suppurative discharge, some elements are scarred;
- III degree of severity - a diffuse conglomerate of inflammatory infiltrates is formed, consisting of merging nodes and abscesses, fluctuation intensifies, many interconnected fistulas are formed, scarring continues; Limitations of joint mobility due to pain sometimes lead to contractures.
There is also a more complex system for determining the severity index of CHG - the modified Sartorius score, which involves quantitative scoring depending on the presence of the main clinical parameters of the disease: the number of certain anatomical zones involved in the process, the number of painful nodes, abscesses, fistula tracts with purulent discharge, scars, superficial pustules and folliculitis, the distance between damaged areas, the presence of healthy skin in the lesion [10].
Some authors [11] use the “Physician General Assessment of the Severity of CHG” (HS-PGA) criteria. The minimum degree is one or more non-inflamed, painless nodes; mild degree - 1-4 inflamed formations, one abscess or fistula; moderate degree - less than 10 inflammatory elements, 1-5 abscesses and fistulas; severe degree - more than 10 nodes, 2-5 abscesses and fistulas; very severe severity - more than 5 abscesses and fistulas.
There is also a scale for assessing the HSSI severity index in points: mild - from 0 to 7 points, moderate - 8-12, severe - 13 or more. When calculating, the number of affected areas, pain syndrome, number of inflammatory elements, socialization, etc. are taken into account [12, 13].
The Hidradenitis Suppurativa Clinical Response Scale (HiSCR) was one of the latest to be developed to assess CHG. This scale was proposed in the treatment of CHG with adalimumab; it shows a decrease of 50% or more in the number of inflammatory elements and no signs of an increase in abscesses or fistulas with CHG compared with the baseline [14, 15].
A multidisciplinary approach to solving the problem of CHG requires not only the study of severity and the development of rating scales, but also the analysis of laboratory parameters and the development of the most optimal tactics in the treatment of such patients by both dermatologists and surgeons. N. Yaşar et al. [16] focused on changes in hematological parameters in CHG depending on the severity of the disease. It was found that hemoglobin level was higher in stage I than in stage III, while hematocrit, mean platelet volume, corpuscular hemoglobin concentration level and platelet count did not differ between stages. The number of leukocytes and neutrophils was higher in stage III than in stage II, and the number of lymphocytes was lower in stage III than in stage II. These changes can be further used to assess the severity of CHG.
Treatment of CHG can be divided into conservative and surgical. Conservative methods include local, systemic and other types of therapy. Considering the impact of the disease on the quality of life, increased attention should be paid to the psychosocial adaptation of patients. The doctor's recommendations should also be aimed at reducing risk factors for the disease. Since smoking and obesity show the strongest correlation with the severity of the pathological process, patients with CHG should be advised to quit smoking and take measures to reduce body weight [2].
In our country, the approach to the treatment of CHG is similar to the treatment of deep pyoderma and is determined by the use of anti-inflammatory and antibacterial drugs [17, 18]. Recent publications by Russian authors show a positive effect of therapy with TNF-α inhibitors, but, unfortunately, these studies are rare [19].
In European recommendations [20], antibiotics are mentioned as first-line drugs in the treatment of CHG, taking into account the severity according to H. Hurley. However, antibacterial therapy, especially long-term, is often accompanied by complications from parenchymal organs. In addition, if it is impossible to identify the species of bacteria in culture and determine the sensitivity of the microflora from the lesion, antibacterial therapy may be ineffective and cause only a short-term effect. Antibiotics, as a rule, are used for all degrees of severity of CHG and without fail in the pre- and postoperative periods. Most often these are lincosamides, tetracyclines, rifampicin, cephalosporins, etc.
The use of steroid drugs and dapsone was abandoned due to their low clinical effectiveness [21–24].
Therapy with biological drugs and tumor necrosis factor-α blockers against CHG is effective, but has a number of limitations: it is not used in severe forms of the disease, profuse suppuration and abscess formation, the risk of spreading infection, initiation of immunosuppressive therapy, and some diseases of internal organs [25, 26]. Adalimumab, which is used at a dose of 40 mg/week, has been more thoroughly studied [27]. Less popular is etanercept, which has shown little effectiveness in treating CHG [28].
The results of a number of studies have been published [29, 30] based on small clinical material on the use of new immune methods of exposure to the drug apremilast, a molecular selective inhibitor of phosphodiesterase 4 (PDE4). Some effectiveness has been shown in the treatment of CHG.
Recent publications show that timely, early and wide surgical excision of purulent foci in the treatment of any stages of CHG is the most effective way to achieve recovery, prevent complications and relapses, and quickly improve the quality of life of patients [31-33]. The volume and type of surgical intervention are determined individually in accordance with the age, severity, localization of the inflammatory process and general status of the patient. Preoperative preparation is important because it affects the outcome of surgery and subsequent recovery. Z. Alharbi et al. [30] conducted a retrospective analysis of 50 operations with wide surgical access in 32 patients; 81.25% had no relapses after treatment.
Other methods of intervention for CHG have been described: cryoinsufflation, botulinum therapy, photodynamic therapy (PDT). However, the results are heterogeneous and isolated [33].
Along with traditional surgical methods, laser surgery is used. Carbon dioxide (CO2) laser ablation has shown fairly high efficiency. P. Hazen et al. [34], using a sample of 22 patients, showed positive results in the treatment of hidradenitis using a long-pulse neodymium diode yttrium aluminum garnet laser (Nd:YAG laser) - 72.7 compared to 22.9%.
In the context of growing interest in the problem of CHG in our country, a search is being carried out for new medications and optimal surgical methods for treating this disease, algorithms for patient management are being created depending on the duration of the disease, localization, severity and prevalence of the purulent-inflammatory process, rules for preoperative preparation and postoperative preparation are being developed. management of patients with CHG.
A necessary condition for radical excision of foci of inflammation and the success of the operation is careful preoperative preparation of the patient. In order to maximize the relief of perifocal inflammation, reduce purulent discharge from fistulas, delimit infiltrates from healthy tissue, increase the overall resistance of the body, normalize the temperature reaction, peripheral blood parameters and immunological parameters, antibiotic and actinolysate therapy are carried out, as well as evacuation of purulent masses with microorganisms from the fistula tracts by washing them with antiseptic solutions [35, 36].
In our country, there is no single algorithm that would allow us to determine the indications for conservative and surgical treatment of CHG. The search for new treatment methods, as well as the development of a unified clinical classification and rating scales are urgent tasks at the present stage.
Thus, future research should focus on optimizing treatment.
Information about authors
Burova S.A. — https://orcid.org/0000-0003-0017-621X
Borodulina K.S. – https://orcid.org/0000-0001-7670-1450
Corresponding author:
Borodulina K.S. — email
Classification
There are several forms of axillary hidradenitis:
- Acute purulent form. The pathology develops due to blockage of the apocrine sweat and sebaceous glands. Among patients with this form of the disease are people who do not take good care of their armpits. Hidradenitis in this form occurs as a typical inflammation in the body: low-grade fever, sometimes rising to 38 degrees, malaise, discomfort, developing into pain in the armpits. The purulent form is life-threatening for the patient if he does not seek treatment from a doctor.
- Chronic hidradenitis is more often called a recurrent form, which is characterized by a purulent process that lasts a long time. The disease often appears at regular intervals with an acute purulent phase. The area of apocrine glands affected by inflammation increases. Lack of treatment for purulent processes is dangerous due to septic consequences, threatening the life of the patient.
- If you take sufficient care of your armpits, but do not shave carefully, the delicate skin of this area may become injured. Staphylococcal or other types of pathogenic microflora get into scratches and wounds. Hidradenitis nodosa begins to form, tending to develop into purulent if left untreated.
Like hidradenitis inguinalis, axillary develops through stages over 10 days.
Therapy for inflammation of the sweat glands
The disease is dangerous due to serious purulent complications, including the development of sepsis, so treatment of the symptoms of hidradenitis and elimination of the pathogen must be timely.
At the initial stages of the pathology, conservative therapy is successfully used, which consists of enhanced antiseptic treatment of the damaged area of the skin, exposure to dry heat, and ultraviolet light. To prevent further development of the disease, local antibacterial ointments and gels, application of bandages with an anti-inflammatory effect, as well as systemic antibacterial drugs are prescribed.