Developmental defects and preterm birth are the leading causes of childhood mortality, chronic disease and disability in many countries. In 2010, the World Health Assembly adopted a resolution calling on all Member States to promote primary prevention and health promotion of children with developmental disabilities through:
- developing and strengthening registration and surveillance systems;
- gaining experience and building capacity;
- strengthening research and scientific work in the field of etiology, diagnosis and prevention;
- strengthening international cooperation.
Causes and risk factors
Approximately 50% of all birth defects cannot be attributed to a specific cause, but some causes or risk factors are known.
Socio-economic factors
Although low income may be an indirect determinant, developmental disabilities are more likely to occur in families and countries with limited resources. It is estimated that approximately 94% of severe malformations occur in middle- and low-income countries, where women often do not have access to enough and good enough food and may be exposed to some agent or factor, such as infection or alcohol, that provokes or enhances deviations from the norm in prenatal development. Moreover, motherhood in adulthood increases the risk of chromosomal abnormalities, including Down syndrome, while motherhood at a young age increases the risk of some congenital malformations.
Genetic factors
Incest (consanguinity) increases the prevalence of rare genetic birth defects and nearly doubles the risk of neonatal and infant mortality, mental retardation, and severe birth defects in children born to first-cousin couples. Some ethnic groups, such as Ashkenazi Jews and Finns, have a relatively high prevalence of rare genetic mutations that lead to an increased risk of birth defects.
Infections
Maternal infections such as syphilis or measles are common causes of birth defects in low- and middle-income countries.
Maternal nutrition
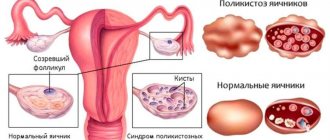
Iodine deficiency, folic acid deficiency, obesity or conditions such as diabetes mellitus are associated with certain developmental defects. For example, folic acid deficiency increases the risk of having a baby with a neural tube defect. In addition, increased intake of vitamin A may affect the normal development of the embryo or fetus.
Environmental factors
Maternal exposure to certain pesticides and other chemicals, as well as certain drugs, alcohol, tobacco, psychoactive substances, or radiation during pregnancy may increase the risk of the fetus or newborn developing birth defects. Working or living near or in the vicinity of landfills, smelters, or mines may also be a risk factor, especially if the mother is exposed to other environmental hazards or is malnourished.
Huntington's chorea
Huntington's chorea (Huntington's disease) is a genetic, progressive neurodegenerative disease characterized by the gradual development of involuntary muscle movements affecting the arms, legs, face and trunk, as well as progressive deterioration of cognitive processes and memory, and mental disorders.
The disease is inherited in an autosomal dominant manner (can be transmitted through both the female and male lines) and occurs as a result of mutations in the HHT gene (expansion of cytosine-adenine-guanine trinucleotide repeats).
Symptoms and physical manifestations of the disease result from the degeneration of nerve cells (neurons) in certain areas of the brain (basal ganglia, cortex) and usually appear between the ages of 35 and 45. The life expectancy of a person suffering from Huntington's disease is 15–20 years from the onset of symptoms. They include: choreic hyperkinesis (chaotic, jerky, erratic movements of varying amplitude and intensity), involuntary movements of the eyes (nystagmus) and facial muscles, frowning and raising the eyebrows, decreased cognitive abilities, irritability, anxiety, apathy, hallucinations, depression, anosmia, problems with balance and walking, general weakness, weight loss associated with malnutrition, in the late stage of the disease - muscle rigidity, bradykinesia (slowing of active movements), serious worsening of the choreic syndrome, loss of the ability to speak, move, dysphagia, inability to care for oneself.
There is a less common (5-10% of cases) form of hCG that develops in childhood or adolescence (juvenile Huntington's disease). It is also characterized by hyperkinesis, decreased cognitive abilities, impaired coordination and mental disorders. Children experience a rapidly progressive decline in school performance associated with impaired cognitive abilities. Other symptoms include bradykinesia, tremor, myoclonic spasms, dystonia, muscle rigidity, speech dysfunction, and dysphagia. These symptoms can affect the mental state, causing irritability, bad mood, sadness, fears, and aggression. In some cases, behavioral problems are the first sign of the onset of the disease.
The juvenile form is also inherited in an autosomal dominant manner (but most often from fathers) and occurs as a result of mutations in the HTT gene. Life expectancy (from the onset of symptoms) is no more than 15 years.
The diagnosis of Huntington's chorea is made based on symptoms, family history, and molecular genetic testing.
There are no medications that affect the cause of the disease. Patients with hCG are prescribed symptomatic therapy aimed at alleviating symptoms (in particular, choreic hyperkinesis, dystonia, muscle rigidity, behavioral and mental disorders) and improving quality of life.
Prevention
Preventive health measures taken in preparation for pregnancy and the period of conception, as well as prenatal care, reduce the incidence of some congenital malformations. Primary prevention of developmental defects includes the following measures:
- Improving women's nutrition throughout the reproductive years by ensuring adequate intake of vitamins and minerals, especially folic acid, through daily oral supplementation or fortification of staple foods such as wheat or corn flour.
- Monitoring that the pregnant woman does not consume or consumes in limited quantities unhealthy foods, especially alcohol.
- Prevention of diabetes in preparation for pregnancy and during pregnancy through counseling, weight control, proper nutrition and, if necessary, insulin administration.
- Prevention during pregnancy of exposure to hazardous substances contained in the environment (for example, heavy metals, pesticides, certain medications).
- Ensure that any exposure of a pregnant woman to drugs or radiation for medical purposes (such as X-rays) is justified and based on a careful analysis of risks and health benefits.
- Expanding vaccination coverage for women and children, especially against the rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine may also be given at least one month before pregnancy to women who have not received the vaccine or who did not have rubella in childhood.
- Expanding vaccination coverage for women and children, especially against the rubella virus. This disease can be prevented by vaccinating children. Rubella vaccine can also be given to women who are not immune to the disease at least one month before becoming pregnant.
- Expanding and strengthening training for health care workers and other staff involved in strengthening the prevention of developmental disabilities.
Acquired fetal pathologies
Acquired pathologies arise under the influence of negative factors (radiation, toxic poisoning) and the mother’s lifestyle (alcoholism, smoking, drug addiction).
Congenital defects of organs and bones
Rarely does a fetus develop one such defect; usually it is a complex of pathologies affecting several vital organs.
Congenital defects have the following types:
- aplasia - complete absence of an organ with preservation of the vascular pedicle;
- agenesis - complete absence of an organ without preservation of the vascular pedicle;
- hypoplasia - underdevelopment of an organ;
- Dystopia - placement of an organ in the wrong place.
Ultrasound diagnosis of congenital defects is carried out three times:
- 1st diagnosis - 10-13 weeks;
- 2nd diagnosis - 19-20 weeks;
- 3rd diagnosis - 31-32 weeks.
The study allows us to identify most pathologies:
- absence or deformation of an organ;
- anencephaly (absence of the brain);
- atresia (absence) of limbs;
- anomaly of the facial skeleton (cleft lip, cleft palate);
- non-closure of the spinal canal;
- heart defects;
- hydrocephalus (fluid accumulation in the brain).
Hypertensive-hydrocephalic syndrome
This is a pathology in which cerebrospinal fluid accumulates under the meninges. The complication is detected by ultrasound in the late stages of pregnancy.
It is characterized by a large volume of the fetal head, disproportion between the cerebral lobes, and protruding fontanel. The earlier the pathology is detected, the greater the chances of a favorable outcome.
Hydrocephalus
This is the accumulation of cerebrospinal fluid in the ventricles of the brain, as a result of which they increase in size and intracranial pressure increases.
Hydrocephalus is detected in the 2nd semester of pregnancy. The main indicator is an increase in the height of the body of the cerebral ventricle above normal (over 1.1 cm). At the same time, the echogenicity of the interhemispheric fissure decreases while the width of the fissure increases over 5 mm.
Heart defects
Heart defects in the fetus are not uncommon. They are detected on ultrasound during the 2nd routine examination (screening ultrasound of the second trimester).
These include:
- hypoplasia of the left side of the heart;
- lack of communication between the right chambers of the heart;
- absence of one of the ventricles of the heart;
- pathology of the heart muscle;
- arrhythmia;
- bradycardia;
- narrowing of the aortic lumen;
- narrowing of the pulmonary artery;
- tricuspid valve defect;
- tetralogy of Fallot (combined cardiac anomaly).
Most heart pathologies are corrected surgically. The earlier the surgery is performed, the greater the chances of a successful recovery.
Revealing
Health care before conception (preconception) and around the time of conception (periconception) includes basic reproductive health care as well as medical genetic screening and counseling. Screening can be done during the three periods listed below.
- Pre-pregnancy screening is designed to identify people who are at risk of developing certain health conditions or at risk of passing on certain health conditions to their children. Screening includes reviewing the family's medical history and screening to identify a carrier of infection. Screening is especially important in countries where incestuous marriages are common.
- Preconception screening: Maternal characteristics may increase risk, and screening results should be used to guide appropriate care based on risk. During this period, screening of young and mature mothers, as well as screening for the use of alcohol, tobacco and other psychoactive substances, can be carried out. Ultrasound examination methods can be used to detect Down syndrome during the first trimester of pregnancy and severe fetal malformations during the second trimester. Additional tests and amniocentesis can help identify neural tube defects and chromosomal abnormalities during the first and second trimesters of pregnancy.
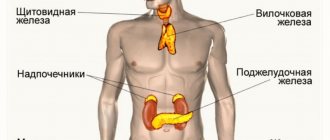
- Newborn screening involves a clinical examination as well as screening for hematological, metabolic and hormonal disorders. Screening for deafness and heart defects and early detection of birth defects can facilitate life-saving treatment and prevent the progression of the defect, which may lead to some form of physical, mental, or vision or hearing disability. In some countries, all newborn babies are screened for thyroid and adrenal pathologies before being discharged from the maternity ward.
How to prevent fetal defects and where to get a fetal ultrasound in St. Petersburg
You can prevent most problems with pregnancy and fetal pathologies by planning your pregnancy in advance. When undergoing examination during planning, both partners undergo tests that clearly show the likelihood of genetic abnormalities. A range of tests are also carried out for infections that can cause deformities in the baby (TORCH complex) and other studies.
We invite you to undergo an ultrasound scan for fetal pathology in St. Petersburg at the Diana Clinic. We have installed the latest ultrasound machine with Doppler. The examination is carried out in 3-D and 4-D formats. A disc with the recording is given to you.
If you find an error, please select a piece of text and press Ctrl+Enter
WHO activities
In 2010, the World Health Assembly published a report on birth defects. The report outlines the main components of establishing national programs for the prevention and care of birth defects before and after birth. The report also recommends priority actions for the international community to help establish and strengthen such national programs.
The Global Strategy for Women's and Children's Health, launched in September 2010 by the United Nations in collaboration with government leaders and other organizations such as WHO and UNICEF, plays a critical role in implementing effective and cost-effective actions to improve newborn health and children.
WHO is also working with the National Center on Birth and Developmental Disabilities, part of the US Centers for Disease Control and Prevention (CDC), and other partners to develop global policies to fortify foods with folate at the country level. In addition, WHO is working with partners to provide the necessary technical expertise to conduct surveillance for neural tube defects, monitor efforts to fortify foods with folic acid salts, and strengthen laboratory capacity to assess the risks of birth defects prevented by folic acid salts.
The International Clearinghouse for Surveillance and Research on Birth Defects is a voluntary, non-profit international organization in official relations with WHO. This organization collects birth defects surveillance data and research programs around the world to study, prevent, and mitigate the effects of birth defects.
The WHO Departments of Reproductive Health and Research and Nutrition for Health and Development, in collaboration with the International Clearinghouse for Birth Defects Surveillance and Research and the CDC National Center for Birth Defects and Development, organize annual workshops on birth defect surveillance and prevention and premature birth. The WHO Department of HIV/AIDS is working with these partners to strengthen surveillance of malformations among women receiving antiretroviral drugs during pregnancy as an integral part of the monitoring and evaluation of national HIV programmes.
The GAVI Alliance, whose partners include WHO, is helping developing countries to strengthen the control and elimination of rubella and congenital rubella syndrome through immunization.
WHO is developing normative instruments, including guidelines and a global action plan to strengthen health care and rehabilitation services in support of the implementation of the Convention on the Rights of Persons with Disabilities. Similarly, WHO is helping countries integrate health and rehabilitation services into general primary health care systems, supporting the development of community-based rehabilitation programs and strengthening specialized rehabilitation centers and their linkages with community-based rehabilitation centres.
UN Convention on the Rights of Persons with Disabilities
The WHO Department of Public Health and Environment works across a range of activities and develops interventions to address the environmental and social determinants of child development. These include: children's unique vulnerability to indoor and outdoor air pollution, water pollution, lack of basic hygiene, toxic compounds, heavy metals, waste components and radiation; mixed influence of factors related to the social environment, professional activity and nutrition, as well as the living conditions of children (home, school).
Minor malformations
Minor malformations are detected in approximately 15% of newborns. Structural abnormalities such as microtia (small ears), narrow palpebral fissures, and age spots are not harmful to the health of the individual, but are sometimes associated with serious defects. Thus, children with 1 minor anomaly have a 3% risk of detecting major anomalies, children with two minor anomalies have a 110% risk, and children with three or more have a 20% risk of detecting major malformations. Thus, abnormal ears are an indicator of other defects and are observed in almost all children with syndromic deficiencies.