Published: 07/16/2021 11:20:00 Updated: 07/16/2021
Thyroiditis - inflammation of the thyroid tissue - is a group of pathological conditions that differ in nature, origin and clinical manifestations. This inflammation can be acute or chronic, be autoimmune or infectious, and develop after childbirth or a cytokine storm. In terms of frequency of occurrence, thyroiditis ranks second among disorders of the endocrine system.
Causes of thyroiditis
There are a number of predisposing factors that allow the doctor to assume this diagnosis in the presence of the following clinical signs:
- family predisposition;
- other autoimmune diseases;
- diabetes mellitus (type 1);
- female;
- period from 1 to 6 months after birth;
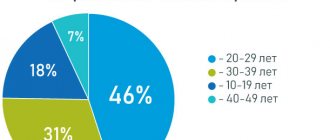
- age (the risk of developing the disease increases with age).
Thyroiditis causes destruction of the thyroid gland, which naturally leads to a decrease in its function, temporary (in acute or subacute process) or permanent (in chronic inflammation).
Acute thyroiditis is often of infectious origin (fungal, bacterial or viral). The pathogen penetrates the thyroid gland through the blood or lymph flow, less often - due to injuries or anatomical abnormalities of this organ.
Subacute thyroiditis can be granulomatous or lymphocytic.
Granulomas - nodules - form on the surface of the thyroid gland under the influence of inflammation. With lymphocytic thyroiditis, the thyroid tissue becomes saturated with lymphocytes, macrophages and other inflammatory cells.
Subacute granulomatous thyroiditis (de Quervain's goiter, viral or giant cell thyroiditis) most often develops after a viral infection (Coxsackie virus, mumps) and has a genetic predisposition. The disease is seasonal, occurring mainly in autumn and winter.
Infraspinous lymphocytic thyroiditis - painless (“silent”), postpartum, spontaneously resolving with thyrotoxicosis - belongs to the group of autoimmune diseases that also have a family predisposition. Beginning as hyperthyroidism, it later leads to hypofunction, but becoming chronic, it slightly affects the level of thyroid hormones.
Chronic thyroiditis can be immune or fibrotic.
Chronic autoimmune thyroiditis - Hashimoto's thyroiditis (goiter), CAIT, lymphocytic struma - is an organ-specific genetically determined autoimmune disease. Antibodies destroy thyroid cells, and the defect can be replaced by lymphoid (hypertrophic form) or fibrous (atrophic form) tissue. The hypertrophic form is characterized by an increase in the tissue of the affected organ, and a nodular goiter may occur. In both cases, the amount of hormones decreases (hypothyroidism). It is Hashimoto's goiter that is more common than other forms of thyroiditis.
Chronic fibrous thyroiditis - thyroiditis or Riedel's struma, woody thyroiditis - a rare fibrous inflammation of the thyroid tissue against the background of widespread or focal sclerosis. The process progresses relatively quickly and ends in hypothyroidism.
Diet for Hashimoto's disease
Using a properly balanced diet is an important support in treating Hashimoto's. In this case, there is no need to use a restrictive elimination diet (if a food allergy is not detected).
Diet recommendations. Important:
- eat regularly (4-5 times a day);
- eliminate animal fats (replace them with vegetable fats);
- eat fresh fruits and vegetables;
- avoid simple sugars;
- to refuse from bad habits.
Fresh fruits and vegetables
Rejection of bad habits
The calorie content of the diet and menu should be determined individually with an endocrinologist.
Symptoms of thyroiditis
Clinic of acute thyroiditis:
- swelling of the neck in front;
- high fever;
- pain radiating to the ear, lower jaw, when swallowing and turning the head;
- redness of the skin on the neck;
- pain when palpating the projection of the thyroid gland.
When an abscess attaches: fever, chills, intoxication.
Possible symptoms of subacute thyroiditis:
- low-grade fever;
- the goiter is dense, sometimes painful on palpation;
- neck pain may occur. The pain starts on one side of the neck and gradually spreads to the other half. The pain can be localized in the middle of the neck, radiating to any direction;
- pain (if any) often radiates to the ear, lower jaw, intensifying when turning the head and swallowing;
- enlarged lymph nodes (cervical, parotid, submandibular);
- tachycardia;
- weight loss;
- sweating;
- anxiety;
- heartbeat;
- irritability.
Clinic of chronic autoimmune thyroiditis (Hashimoto's goiter):
- there may be compression in the neck area;
- possible development of hoarseness;
- drowsiness, lethargy;
- fatigue, asthenia;
- enlargement of the thyroid gland;
- the goiter is dense, mobile, painful to the touch;
- Pain may appear in the front of the neck.
Clinic of chronic fibrous thyroiditis (Riedel's struma):
- compression in the neck;
- dense, motionless goiter;
- pain in the neck;
- difficulty breathing;
- swallowing disorders.
Hashimoto's and other autoimmune diseases (type 1 diabetes, Addison's disease)
Hashimoto's disease often coexists with other autoimmune diseases, such as type 1 diabetes and Addison's disease (primary adrenal insufficiency).
When Hashimoto's meets Addison's disease, we talk about Schmidt's syndrome, that is, a concomitant autoimmune thyroid disease (mainly Hashimoto's) and primary hypoadrenocorticism.
If type 1 diabetes additionally occurs, Carpenter syndrome is diagnosed. Both syndromes constitute autoimmune polyglandular deficiency syndrome type 2 (abbreviated as APS-2).
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Diagnosis of thyroiditis
The diagnosis of thyroiditis, regardless of its form and origin, is based on a clinical examination and laboratory diagnosis.
During the examination, body weight is measured, pulse and blood pressure are determined, as well as palpation of the thyroid gland. Of the instrumental studies, scintigraphy is specific - a radioisotope study of the absorption of charged iodine isotopes by thyroid tissue.
Ultrasound examination of the thyroid gland can detect significant changes in its tissues, lymphoid or fibroid degeneration of its areas. To diagnose complications, computed tomography is prescribed.
The most accurate invasive procedure is puncture of the thyroid gland with collection of biological material for biopsy. Its gentle modification is widely used - fine-needle aspiration biopsy or FNA. The procedure lasts a few seconds and allows you to obtain sufficient material for histological examination.
Thyroiditis quickly leads to functional impairment, so making a diagnosis requires starting with a battery of laboratory tests.
Tests for thyroiditis:
- Thyroid hormones in blood serum: total triiodothyronine (T3) and free and serum levels.
- TSH (thyroid stimulating hormone).
- Immunological study of the presence of antibodies to thyroid tissue (antibodies to thyroid peroxidase and antibodies to thyroglobulin).
- A comprehensive clinical blood test, which can reveal a shift in the leukocyte formula to the left, an increase in ESR, neutrophilia, and an increase in the level of C-reactive protein.
Clinical manifestations
The debut of CAIT does not have a specific clinical picture. The onset of an autoimmune process, as a rule, does not have any clinical manifestations at all and is therefore detected either by chance during an ultrasound of the thyroid gland, or is suspected during an appointment with an endocrinologist during palpation of the thyroid gland. During the collection of complaints, the patient may pay attention to mild apathy or nervousness, general weakness or headaches or other autonomic disorders.
As a result of prolonged autoimmune inflammation, protective factors weaken and gland cells begin to destroy, which affects the patient’s well-being. During this period, the clinical picture depends on changes in thyroid function. Basically, the result of the autoimmune process is hypothyroidism, but sometimes the debut of the clinical stage of CAIT begins with thyrotoxicosis. Then the patient notes:
- increase in the above symptoms;
- feeling of heat throughout the body, increased sweating;
- constant heartbeat;
- trembling in hands;
- loss of body weight against the background of increasing appetite;
- disruptions of the menstrual cycle in women, decreased libido in men;
- an increase in the volume of the neck caused by the growth of the thyroid gland.
For hypothyroidism:
- fatigue, drowsiness;
- swelling of the face and legs;
- increased blood pressure and decreased heart rate;
- constipation;
- enlargement of the neck above the jugular fossa.
Most often, changes in thyroid function during CAIT occur according to the following scheme: euthyroidism - thyrotoxicosis - euthyroidism - hypothyroidism. But sometimes the phase of thyrotoxicosis is so short-lived that it cannot be diagnosed
Treatment of thyroiditis
Acute thyroiditis in the case of purulent inflammation requires the use of antibiotics and possibly surgical treatment.
Otherwise, it is treated symptomatically - non-steroidal anti-inflammatory drugs and beta blockers, glucocorticosteroid hormones. For subacute thyroiditis of a non-infectious nature, antihistamines are prescribed, in severe cases - corticosteroids, beta-blockers and NSAIDs, inhaled anti-inflammatory drugs.
Treatment of autoimmune thyroiditis consists of compensating for decreased thyroid function using hormone replacement therapy - taking thyroid hormones in tablets. There are currently no methods of influencing the autoimmune process in the gland itself with proven effectiveness.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
Hashimoto's disease - treatment and prognosis
There is still no effective treatment for hashimoto's. Therapy consists mainly of treating the consequences of the disease, that is, treating hypothyroidism.
Patients whose blood tests show the presence of antibodies, but at the same time no thyroid dysfunction is detected, are advised to undergo systematic testing for the condition of the thyroid gland.
If a diagnosis of hypothyroidism is made, then pharmacological therapy is most often prescribed, which includes taking the missing hormones.
Pharmacological therapy
The key drug in the treatment of hashimoto’s in European clinics is levothyroxine. This is a stable form of a synthetic analogue of natural thyroxine. Preparations with levothyroxine (levothyroxine sodium, Levothyroxinum natricum) have similar properties to the hormone produced by the thyroid gland and are used as hormone replacement therapy for hypothyroidism, chronic thyroiditis (Hashimoto's disease) and thyroid cancer.
If Hashimoto's disease is treated correctly, it does not cause serious consequences. Very rarely, thyroiditis progresses to primary malignant thyroid lymphoma or papillary thyroid cancer.
Stages and types of disease
The World Health Organization divides the development of diffuse nodular goiter into several forms:
- zero;
- primary;
- secondary.
They are determined by the severity of symptoms. With the zero form of diffuse nodular goiter, there are no clinical manifestations. The primary form of the disease can be diagnosed after palpation. Secondary diffuse nodular goiter is when the tumor is visually noticeable.
Classification is also used according to the type of nodular formations. From this point of view, cystic formations and pseudonodules are distinguished. Their number also varies - from single or solitary formations to multinodular, conglomerate ones.
Prevention
Since the exact reasons why diffuse nodular goiter of the thyroid gland develops are not yet clear, preventive measures are precautionary in nature.
Endocrinologists strongly recommend enriching your diet with foods rich in iodine:
- sea fish;
- crustaceans;
- seaweed;
- whole milk;
- beef.
Adequate nutrition is especially important when the immune system is weakened, in childhood and old age. If one of your close relatives has been diagnosed with diffuse nodular goiter, it is recommended to regularly visit an endocrinologist and monitor hormone levels through testing - at least once a year. Good sleep, a properly organized rest regimen, and an active lifestyle will also help reduce the risk of developing the disease.