The male reproductive system is extremely important, like the rest of the body systems that ensure normal functioning. Therefore, failure to contact a specialist in a timely manner, or, even worse, ignoring warning signs, creates much greater problems than they were initially.
The male reproductive system has three main tasks:
- The formation of sperm in the testes (spermiferous tubules). During one ejaculation, 30-500 million sperm are released.
- Evacuation of seminal fluid from the male genital organs and its delivery to the female genitals.
- Synthesis of the main androgen (a group of male steroid sex hormones) - testosterone.
TESTOSTERONE
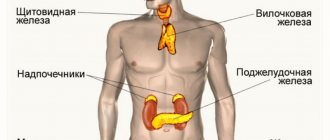
The bulk of testosterone (male sex hormone) is produced by the testes; a smaller amount is produced by cells of the reticular layer of the adrenal cortex and during transformation from precursors in peripheral tissues. In women, testosterone is formed during the process of peripheral transformation, as well as during synthesis in the cells of the inner lining of the ovarian follicle and the reticular layer of the adrenal cortex. Testosterone ensures in men the formation of the reproductive system according to the male type, the development of male secondary sexual characteristics during puberty, is responsible for maintaining sexual function (libido and potency), sperm maturation, development of the skeleton and muscle mass, stimulates the bone marrow, the activity of the sebaceous glands, modulates synthesis of b-endorphins (“hormones of joy”), insulin. In women, it is involved in the mechanism of follicle regression in the ovaries and in the regulation of the level of gonadotropic hormones of the pituitary gland. Only free testosterone dissolved in plasma is biologically active, which in the human body plays the role of a protein anabolic, that is, it stimulates protein synthesis. It is for this reason that men tend to be larger and more muscular than women. In many structures localized (located) in the skin, testosterone supplied with the blood determines the male type of hair (beard growth, etc.) and excess sebaceous secretions (seborrhea). Testosterone levels in men increase during puberty and remain high until the age of 60 on average. During the day, the concentration of the hormone in the blood plasma fluctuates (max. - in the morning, min. - in the evening). In women, the maximum concentration of testosterone is determined in the luteal phase and during ovulation. In pregnant women, it increases by the third trimester, exceeding almost 3 times the concentration in non-pregnant women. Indications for the analysis: In both sexes: infertility, baldness, acne, oily seborrhea, adrenal tumors. In women: hirsutism, anovulation, amenorrhea, oligomenorrhea, dysfunctional uterine bleeding, miscarriage, polycystic ovary syndrome, uterine fibroids, endometriosis, breast neoplasms, hypoplasia (underdevelopment) of the uterus and mammary glands. In men: impaired potency, decreased libido, male menopause, primary and secondary hypogonadism, chronic prostatitis, osteoporosis. An increase in testosterone levels in the blood may indicate premature puberty (in boys), adrenal hyperplasia, or tumors that produce sex hormones. Testosterone levels are usually reduced in Down syndrome, renal, liver failure, and gonadal failure. Preparation for the study: on the eve of the study, it is necessary to exclude physical activity (sports training) and smoking. In women, the analysis is performed on days 6-7 of the menstrual cycle, unless other dates are indicated by the attending physician.
HOW IS SPERM FORMED?
The production of sperm is called spermatogenesis. It can only occur under the influence of hormones, therefore, until puberty (12–16 years), the boy’s body is not able to produce sperm.
When testosterone levels rise in a teenager's body, spermatogonia, special stem cells in the testicles, are activated. They turn into spermatocytes. These cells contain a double set of chromosomes; after division, secondary spermatocytes are formed, each containing one set of chromosomes.
A person has two sex chromosomes - X and Y. An egg can only contain chromosome X. A sperm can contain either X or Y. If the egg is fertilized by a sperm with a Y chromosome, the result is a boy, if with an X, the result is a girl.
Spermatid cells are formed from spermatocytes. The complex process of sperm formation does not end there. Spermatid cells go through a process known as spermiogenesis. They grow tails and acquire features characteristic of sperm. After maturation in the epididymis, they are ready to leave the man’s body in search of an egg.
A mature sperm can move at a speed of 20 cm per hour. And this despite the fact that its length is 0.05 mm.
SHBG (SEX HORMONE BINDING GLOBULIN)
Most of the testosterone entering the blood binds to a specific transport protein - SHBG. A decrease in SHBG synthesis leads to disruption of the delivery of hormones to target organs and the performance of their physiological functions. In men, SHBG secretion increases with age. This can lead to a decrease in active testosterone and an increase in the effects of estrogen, which is manifested by gynecomastia (enlargement of the mammary glands in men) and redistribution of fatty tissue according to the female type. In women, the SHBG content is almost twice as high as in men, since estrogens increase the level of SHBG synthesis in the liver, and androgens, on the contrary, reduce its production. Indications for the analysis: In both sexes: clinical signs of an increase or decrease in androgen levels with normal testosterone levels, baldness, acne, oily seborrhea. In women: hirsutism, anovulation, amenorrhea, polycystic ovary syndrome, prediction of the development of preeclampsia (SHBG is reduced). In men: male menopause, chronic prostatitis, impaired potency, decreased libido. An increase in SHBG levels can be observed with thyrotoxicosis, liver cirrhosis, taking estrogens and oral contraceptives. A decrease in SHBG levels can occur with hypothyroidism, obesity, acromegaly, Cushing's syndrome, hyperprolactinemia, polycystic ovary syndrome, and after taking androgens. Preparation for the study: on an empty stomach.
Penis size and condom use
Condom rupture has been the subject of several studies. 92 monogamous heterosexual couples aged 18 to 40 years for women and 18 to 50 years for men were included in the upcoming Durex-Ramses condom study. At each sexual intercourse, a diary was kept, which included information about the use of a condom, its rupture and slippage. In France, a telephone survey of 20,000 random individuals involved 4,500 sexually active people, of whom 731 had used a condom in the previous year and 707 reported difficulties using condoms. A study in Australia in which 184 men used 3,658 condoms also looked at penis size as a factor in condom breakage and slippage.
Although the most common type of condom is made from latex and is highly stretchable, it is susceptible to dry friction (such as the dry friction movement of friction when heavy pressure is applied or there is no smooth, lubricated movement), as well as other errors in their use. In a separate study, for example, among people who had anal sex, condom breakage was more related to excess friction (in this case, the result of insufficient lubrication) than to penile size itself. The condom breakage rate when used correctly was 1.34% and the slippage rate was 2.05%, for an overall failure rate of 3.39%. Penis size had no effect on slippage, but penis circumference and condom breakage were highly correlated, with larger sizes increasing the breakage rate.
Currently, the problem of condom sizes seems far-fetched. Thus, in the USSR condoms were produced in three sizes: No. 1, No. 2, No. 3, which differed in size. The size No. 1 condom was gradually forced out of sale because it was not in demand - presumably due to the reluctance of men to admit to the smallest size. Condom No. 3 was forced out of production due to the reluctance of the planned economy to waste rubber unnecessarily. “Product No. 2” remained in use - and it was 54 mm wide and 180 mm long, which corresponds to the European size XXL. The production material was rubber. Currently, condoms are most often made from latex, but are not made from rubber at all. Since latex tends to stretch significantly, unlike rubber, the question about the size of the condom is most likely nominal.
Based on materials from Wikipedia - https://u.to/RmFRDg
PROLACTIN
Prolactin is a hormone produced in the anterior pituitary gland; a small amount is synthesized in peripheral tissues, and during pregnancy it is also produced in the endometrium. This hormone plays an extremely important role in many processes occurring in the body, in particular, in ensuring the normal functioning of the reproductive system. Prolactin also contributes to the formation of sexual behavior. It regulates water-salt metabolism, delaying the excretion of water and sodium by the kidneys, stimulates calcium absorption, and has a modulating effect on the immune system. In general, prolactin activates anabolic processes in the body. The daily secretion of prolactin has a pulsating character. During sleep, its level increases. After waking up, the concentration of prolactin decreases sharply, reaching a minimum in the late morning hours. After noon, the hormone level increases. In the absence of stress, daily fluctuations in levels are within normal values. During the menstrual cycle, prolactin levels are higher in the luteal phase than in the follicular phase. From the 8th week of pregnancy, prolactin levels increase, reaching a peak at 20-25 weeks, then decrease immediately before childbirth and increase again during lactation. During pregnancy, prolactin supports the existence of the corpus luteum and the production of progesterone, stimulates the growth and development of the mammary glands and milk formation. An increase in prolactin levels is one of the common causes of infertility. Indications for the analysis: galactorrhea, cyclical pain in the mammary gland, mastopathy, anovulation, oligomenorrhea, amenorrhea, dysfunctional uterine bleeding, infertility, diagnosis of sexual infantilism, chronic inflammation of the internal genital organs, severe menopause, obesity, decreased libido and potency (men) , gynecomastia (men), osteoporosis. The analysis shows an increase in prolactin levels in diseases of the hypothalamus, pituitary gland, primary hypothyroidism, polycystic ovary syndrome, chronic renal failure, cirrhosis of the liver, adrenal insufficiency and congenital dysfunction of the adrenal cortex; tumors that produce estrogen and other conditions. The level of prolactin in the blood is usually reduced in case of pituitary insufficiency, true post-term pregnancy. Preparation for the study: Avoid sexual intercourse and heat exposure (sauna) 1 day before, smoking 1 hour before. Since prolactin levels are greatly influenced by stressful situations, it is advisable to exclude factors that influence the research results: physical stress (running, climbing stairs), emotional arousal. Therefore, before the procedure you should rest for 10-15 minutes and calm down.
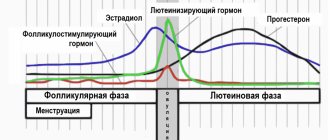
FSH (follicle stimulating hormone)
FSH is a pituitary hormone that regulates the functioning of the gonads. In men, it is secreted constantly evenly, in women - cyclically, increasing in the first phase of the menstrual cycle. FSH promotes the formation and maturation of germ cells: eggs and sperm. The egg in the ovary grows as part of a follicle consisting of follicular cells. These cells, during the growth of the follicle, under the influence of FSH, synthesize female sex hormones - estrogens, which, in turn, suppress the release of FSH (negative feedback principle). Indications for the analysis: decreased libido and potency, infertility, anovulation, oligomenorrhea, amenorrhea, dysfunctional uterine bleeding, miscarriage, premature sexual development or delay, polycystic ovary syndrome, endometriosis, growth retardation, chronic inflammation syndrome of the internal genital organs. An increase in FSH levels may indicate insufficient function of the gonads, a pituitary tumor, primary hypogonadism (in men), ovarian wasting syndrome (in women), renal failure, dysfunctional uterine bleeding and other conditions. The analysis will show a decrease in FSH levels with hypofunction of the pituitary gland or hypothalamus, pregnancy, secondary amenorrhea, polycystic ovary syndrome, hyperprolactinemia. Preparation for the study: The analysis is done on the 6-7th day of the menstrual cycle, unless other dates are indicated by the attending physician. 3 days before taking blood, you must avoid sports training. 1 hour before blood collection - smoking. Immediately before taking blood, you need to calm down. Blood is taken from a vein on an empty stomach, lying down.
Sex differences
The male reproductive gland is the testicle, and the female reproductive gland is the ovary. The presence of a male or female reproductive gland determines the so-called gametic sex (from the Greek gametes - spouse, gamete - spouse), namely the ability of the gland to produce sperm (male reproductive cells) or eggs (female reproductive cells) and produce male or female sex hormones. Sex hormones, in turn, influence the maturation of the genital organs and the appearance of secondary sexual characteristics, which include body features, hair location, structure of the larynx, development of muscles and fat deposits. The activity of the gonads is under the control of the pituitary gland, an endocrine gland located at the base of the brain.
There are significant differences between the sexes not only in the structure of the body, but also in the psyche. For example, women have better developed verbal (speech-related) abilities, while men have better developed mathematical and spatial orientation abilities. Gender (sex hormones) determines a person’s biological, psychological and social life, his sexual identity and behavior. In addition to hereditary factors, the culture to which a person belongs, family upbringing, and other environmental influences also have a significant impact on a person’s sexual behavior.
Let's look at the structure of the gonads.
LH (luteotropic hormone)
In women, luteotropic hormone stimulates the synthesis of estrogen; regulates the secretion of progesterone and the formation of the corpus luteum. In men, by stimulating the formation of sex hormone binding globulin (SHBG), it increases the permeability of the seminiferous tubules to testosterone. This increases the concentration of testosterone in the blood plasma, which promotes sperm maturation. In turn, testosterone re-inhibits the release of LH. The release of the hormone is pulsating in nature and depends in women on the phase of the ovulation cycle. During puberty, LH levels increase, approaching values typical for adults. In the menstrual cycle in women, the peak concentration of LH occurs at ovulation, after which the level of the hormone drops and remains throughout the luteal phase at lower values than in the follicular phase. During pregnancy the concentration decreases. During the postmenopausal period, the concentration of LH increases, as does FSH (follicle-stimulating hormone). In women, the concentration of LH in the blood is maximum in the period from 12 to 24 hours before ovulation and is maintained throughout the day, reaching a concentration 10 times higher compared to the non-ovulatory period. In men, LH levels increase by 60-65 years. Indications for the analysis: hirsutism, decreased libido and potency, anovulation, oligomenorrhea, amenorrhea, infertility, dysfunctional uterine bleeding, miscarriage, premature sexual development or delay, sexual infantilism, endometriosis, monitoring the effectiveness of hormone therapy. An increase in LH levels is observed with insufficient function of the gonads, polycystic ovary syndrome, pituitary tumors, renal failure, and gonadal atrophy in men after testicular inflammation. A decrease in LH levels occurs with secondary amenorrhea; hypofunction of the pituitary gland and hypothalamus, genetic syndromes, anorexia nervosa, polycystic ovary syndrome, luteal phase deficiency, surgical interventions. Preparation for the study: 3 days before taking blood, you must avoid sports training. 1 hour before blood collection - smoking. Immediately before taking blood, you need to calm down. Blood is drawn on an empty stomach, lying down. The analysis is done on days 6-7 of the menstrual cycle, unless other dates are indicated by the attending physician.
What is the size?
Male penis size is a characteristic of the male penis in terms of length and width.
Thread on the forum where we discuss size - https://forum-makarova.ru/malenkij-razmer-chlena.t1559/
**Do you want to know everything about men's health? Streams on Tuesdays and Saturdays!** **Personally from Dr. Makarova! Join the chat so you don’t miss out!* — https://t.me/makarovamama
It is considered correct to measure the length of the penis - in a standing individual by placing a ruler on top of a fully erect penis, width - in several places with averaging. The documented largest penis is considered to be a penis with a length of 33.5 cm and a girth of 15 cm, which was described at the beginning of the 19th century. According to a number of studies, the average length of the penis is about 13-15 cm. And although the issue of women’s preferences is controversial, at all times the issue of increasing the size of the penis has received special attention.
ESTRADIOL
In women, estradiol is produced in the ovaries, placenta and zona reticularis of the adrenal cortex under the influence of FSH, LH and prolactin. Estradiol is formed in small quantities during the peripheral conversion of testosterone. In men, estradiol is formed in the testes, in the adrenal cortex, but most of it is formed in peripheral tissues due to the conversion of testosterone. Estradiol ensures in women the formation of the reproductive system according to the female type, the development of female secondary sexual characteristics during puberty, the formation and regulation of menstrual function, the development of the egg, the growth and development of the uterus during pregnancy. It is also responsible for the psychophysiological characteristics of sexual behavior and ensures the formation of subcutaneous fatty tissue according to the female type. A necessary condition for the effects of estradiol to occur is the correct relationship with testosterone levels. Estradiol has an anabolic effect, enhances bone turnover and accelerates the maturation of skeletal bones; promotes sodium and water retention in the body, reduces cholesterol levels and increases blood clotting activity. Daily fluctuations in the concentration of estradiol in the serum are associated with the rhythm of LH (luteinizing hormone) secretion: the maximum occurs between 15 and 18 hours, and the minimum between 24 and 2 hours. In women of childbearing age, the level of estradiol in the blood serum and plasma depends on the phase of the menstrual cycle. cycle. The highest levels of estradiol are observed in the late follicular phase. During pregnancy, the concentration of estradiol in serum and plasma increases at the time of delivery, and after delivery it returns to normal on the 4th day. With age, women experience a decrease in estradiol concentrations. During postmenopause, the concentration of estradiol decreases to the level observed in men. Indications for the purpose of the analysis: diagnosis of disorders of the menstrual cycle and fertility (ability to produce offspring) of women, amenorrhea, oligomenorrhea, anovulation, hypogonadism, disorders of puberty, osteoporosis (in women), hirsutism, infertility, premenstrual syndrome, signs of feminization in men. An increase in estradiol levels is observed with hyperestrogenism; endometrioid ovarian cysts; tumors of the ovaries, testicles, liver cirrhosis, pregnancy, taking hormonal drugs. Estradiol levels are reduced during intense physical activity in untrained women, with significant weight loss, a high-carbohydrate, low-fat diet, in vegetarians, and in early pregnant women who smoke; for chronic inflammation of the internal genital organs, chronic prostatitis, insufficiency of the gonads and other conditions. Preparation for the study: on the eve of the study, avoid physical activity (sports training) and smoking. In women, the analysis is performed on days 6-7 of the menstrual cycle, unless other dates are indicated by the attending physician.
Structure and functions of the external male genitalia
The group of male external reproductive organs includes:
- Penis (penis) is an organ involved in sexual intercourse, ejecting seminal fluid. The place of attachment of the phallus to the pubis is the root. The body of the penis and the head are covered by the foreskin (fold of skin), which normally should be easily and painlessly retracted, exposing the head. The foreskin contains multiple glands that produce smegma (sebaceous lubricant). Inside, the penis consists of two cavernous (cavernous) and one spongy (spongy) bodies. It is to the cavernous bodies that a man owes the appearance of an erection, in which the bodies are filled with blood and “swell”, increasing the size of the penis. The corpus spongiosum contains the urethra (urethra), which blocks the passage of urine during coitus and ejaculation.
- Testicles (testicles) - olive-shaped paired organs of different sizes produce testosterone and sperm. They are located in the sac (scrotum), which acts as a “climate control”. For healthy spermatogenesis (sperm production), the testicles must be maintained at a constant temperature below the general body temperature. This is provided by the scrotum and the external location of the testicles. Otherwise, spermatogenesis will be impaired, which will negatively affect fertility (the ability to conceive).
- The epididymis is an oblong narrow paired organ, part of the vas deferens. In the epididymis, sperm accumulate and mature for further movement into the vas deferens. Sperm accumulate in a thickening formed in the tail. In the scrotum, the epididymis is adjacent to the testicle, forming a pouch. Normally, it can be easily felt through the scrotum.
PROGESTERONE
Progesterone is a female sex hormone produced in the corpus luteum of the ovaries and adrenal glands. Outside of pregnancy, progesterone secretion begins to increase in the preovulatory period, reaching a maximum in the middle of the luteal phase, returning to its original level at the end of the cycle. The content of progesterone in the blood of a pregnant woman increases, doubling by 7-8 weeks, and then gradually increasing until 37-38 weeks. After ovulation - the release of an egg from the follicle - a corpus luteum is formed in its place in the ovary - a gland that secretes progesterone. It exists and secretes this hormone during 12-16 weeks of pregnancy until the moment when the placenta is fully formed and takes over the function of hormone synthesis. If conception does not occur, the corpus luteum dies after 12-14 days, and menstruation begins. Progesterone is determined to assess ovulation and the viability of the corpus luteum. With a regular cycle - a week before menstruation, when measuring rectal temperature - on the 5-7th day of its rise; with an irregular cycle - several times. A sign of ovulation and the formation of a full-fledged corpus luteum is a tenfold increase in progesterone levels. Indications for the analysis : identifying the causes of menstrual irregularities, infertility, dysfunctional uterine bleeding, assessing the condition of the placenta in the second half of pregnancy, differential diagnosis of true post-term pregnancy. An increase in progesterone levels is observed with adrenal hyperplasia, corpus luteum cyst, pregnancy, and delayed maturation of the placenta. The analysis will show a decrease in progesterone levels in the absence of ovulation, insufficiency of the corpus luteum, true postmaturity, placental insufficiency, intrauterine growth restriction, or threatened abortion. Preparation for the study: the analysis is carried out on the 22-23rd day of the menstrual cycle, unless other dates are indicated by the attending physician. Blood is taken in the morning on an empty stomach, that is, when 8-12 hours pass between the last meal and blood collection. You can drink water.
Measuring a man's penis
In order to take an accurate measurement, the penis must be fully erect. This may be difficult to achieve in a medical setting. At least one Brazilian doctor resorted to injecting drugs into the penis to induce a full erection, which produced more permanent results.
Some clinicians measured the penis by stretching it in a non-erect state as far as possible. Men's self-measurement of their penises is unreliable because they often want to report a larger penis.
To obtain the most accurate measurements of an individual's penis size, it is recommended that multiple measurements be taken on different days and at different times, preferably with different erections. After this, the results obtained are averaged. This approach accounts for what may be natural fluctuations in size due to level of sexual arousal, time of day, room temperature, frequency of sexual activity, and unreliability of measurement methods.
Measuring the length (from above) and width of the penis.
The length can be measured with a standing individual when the penis is parallel to the floor. The penis is measured along the upper surface from the base of the penis to its tip. The results are considered inaccurate if measurements were taken along the lower surface of the penis, as well as if the individual was sitting or bent over.
Penis girth
- This is the measurement of the circumference of the penis in a state of full erection. With variations, this is quoted as the average of three measurements: just below the glans penis, in the middle of the shaft, and at the base of the penis.
DEA-SO4 (Dehydroepiandrosterone sulfate)
DEA-SO4 is produced in the adrenal cortex. Its level is an adequate indicator of androgen-synthetic activity of the adrenal glands. The hormone has only a weak androgenic effect, but during its metabolism testosterone and dihydrotestosterone are formed in peripheral tissues. During pregnancy, DHEA-SO4 is produced by the adrenal cortex of the mother and fetus and serves as a precursor for the synthesis of placental estrogens. By puberty, the level of this hormone increases, and then gradually decreases as a person reaches reproductive age. The level of DHEA-SO4 also decreases during pregnancy. Indications for the analysis: adrenogenital syndrome, tumors of the adrenal cortex, ectopic ACTH-producing tumors, recurrent miscarriage, fetal hypotrophy, diagnosis of the state of the feto-placental complex from 12-15 weeks of pregnancy. Increased levels of DHEA-SO4 are observed in adrenogenital syndrome; tumors of the adrenal cortex; ectopic ACTH-producing tumors; Cushing's disease; feto-placental insufficiency; hirsutism in women; threat of intrauterine fetal death. The level of DHEA-SO4 is reduced in case of fetal adrenal hypoplasia (concentration in the blood of a pregnant woman); intrauterine infection; when taking gestagens.
Publications in the media
Diagnosis and clinical problems associated with distorted sexual differentiation require an understanding of the mechanisms of development of the gonads and ducts.
Normal sexual differentiation . The gonad primordia in humans do not develop sexual differentiation until the 45th–50th day of intrauterine development. In the early stages, internal genital ducts are present: both male (Wolffian, or mesonephric duct) and female (Müllerian, or paramesonephric duct) and undifferentiated gonads (genital ridges). Later (critical phase - 8 weeks of intrauterine development), differentiation of male and female genital organs occurs in various ways dictated by genetic and hormonal factors.
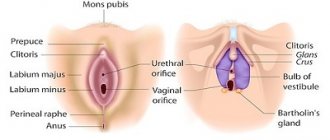
• Differentiation according to the male type. Genotype - 46,XY • Y-chrom. - male sex determinant. Under the influence of a regulatory factor (a factor that determines the development of testicles), encoded by the Y chromosome, the genital ridges develop as testicles; in the absence of the factor, the ovaries develop • Leidig cells of the fetal testicles, under the control of gonadotropins (chorionic and pituitary), secrete testosterone •• Under the influence of testosterone, the following develop from the mesonephric duct: vas deferens, epididymis, seminal vesicles •• 5-Reductase catalyzes the conversion of testosterone to dihydrotestosterone ( DHT), necessary for differentiation of the external genitalia (scrotum, penis), which is completed by 12–14 weeks of intrauterine development •• Sertoli cells of the fetal testicles secrete Müllerian inhibitory factor (MIF), which causes regression of the Müllerian ducts in the male fetus.
• Differentiation according to the female type (genotype - 46,XX) occurs in the absence of the factor Y-chromium, testosterone, DHT and MIF, which determines the development of the testicles. • In the absence of Y-chrom. genital ridges develop as ovaries • In the absence of MIF, the Mullerian duct develops into the fallopian tubes, uterus and upper third of the vagina • In the absence of testosterone and DHT, the Wolffian duct degenerates and the clitoris, labia majora and minora, and vagina develop • The ovaries begin to function at puberty; formation according to the female phenotype occurs autonomously, under the influence of hormones of the placenta and the maternal body. Distortions of sexual differentiation lead to the birth of a child who has characteristics of both male and female, but is not completely (phenotypically!) either male or female.
• True hermaphroditism . The gonads contain tissue from both the testes and ovaries. Karyotype: in approximately 80% - 46.XX, the remaining cases - 46.XY or mosaicism. The etiology is unclear •• There is usually significant virilization, as a result of which most true hermaphrodites are raised as males. Gynecomastia and cyclic hematuria may occur as a result of uterine bleeding. • A serious suspicion of true hermaphroditism should arise if the child has transitional type genitalia, an XX karyotype and a normal level of 17-hydroxyprogesterone, which excludes 21-hydroxylase deficiency. The final diagnosis is based on surgical exploration and detection of the gonads containing tissue from both the ovary and testes.
• Mixed dysgenesis of the gonads is observed with karyotype 45,X/46,XY •• Clinic: a wide range of structure of the external genital organs - from completely male to completely female ••• The gonads can look different: from externally recognizable ovaries to dysgenetic testes; Gonadal asymmetry is often observed ••• Effects of the 45,X cell line may mimic the phenotype of Turner syndrome •• Diagnosis is made by karyotyping.
• Male pseudohermaphroditism . Children of genotype 46,XY; there are testicles, but masculinization is incomplete (hypospadias, microphallia, underdeveloped scrotum with or without testicles). Male pseudohermaphroditism is observed in a variety of endocrine disorders (defects in testosterone synthesis, its metabolism and effects on target cells) •• Reifenstein syndrome. Familial form of male pseudohermaphroditism: phenotypically indeterminate gender of the genitals, hypospadias, postpubertal gynecomastia; infertility due to sclerosis of the seminiferous tubules. Synonym: Klinefelter–Reifenstein–Albright syndrome •• Testicular feminization (see Testicular feminization syndrome) •• Male pseudohermaphroditism (*300018, Xp21.3, DSS gene, À ) is a locus on the X chromosome, the duplication of which leads to sex inversion.
• 5a-reductase deficiency (*264600, r) impairs the conversion of testosterone to DHT •• Boys (karyotype 46XY) are born with external genitalia of indeterminate gender. Some newborns are classified as girls due to minimal evidence of virilization at birth •• Testosterone-dependent changes occur during puberty: movement of the testes to their final position, increase in muscle mass, deepening of the voice •• There is a report of one isolate in which many children were raised as girls, but after puberty they acquired pronounced features of a male phenotype •• Diagnosis can be made by detecting an increased testosterone/DHT ratio after HHT stimulation.
• Disorders of testosterone synthesis and metabolism are rarely observed; Several forms of enzyme deficiency are known (r) •• Cholesterol desmolase deficiency. A severe form of salt loss is characteristic. Severe deficiency of mineralocorticoids and GCs, as well as androgens, leads to death in early childhood, despite steroid hormone replacement therapy •• 3b-hydroxysteroid dehydrogenase deficiency. Men are not completely virilized (defect in testosterone synthesis). Women can be mildly virilized. The diagnosis is based on the detection of elevated blood concentrations of dehydroepiandrosterone and 17-hydroxypregnenolone •• 17a-hydroxylase deficiency •• 17-oxidoreductase deficiency prevents the conversion of androstenedione to testosterone. The diagnosis can be established by detecting an increased ratio of androstenedione to testosterone after HCG stimulation •• Testicular 17-a-ketosteroid reductase deficiency (*264300, 9q22, HSD17B3 gene, EDH17B3, r) - clinically indistinguishable from 5-a-reductase-2 deficiency (264600) •• 17,20-desmolase deficiency (*309150, À r) is a rare cause of male pseudohermaphroditism resulting from a block in the conversion of progestogens to androgens. The defect can be detected by a distorted ratio of progestogens and androgens both at basal levels and after stimulation with hCG. In women, the genitals are normal, but puberty does not occur (no estrogen).
• Female pseudohermaphroditism . Children with the 46.XX genotype (ovaries present) but usually have a male phenotype at birth. Increased sensitivity of the XX fetus to the effects of androgens during the critical period (8 weeks of intrauterine development) leads to the development of varying degrees of severity of labioscrotal fusion, the formation of the urogenital sinus and enlargement of the clitoris. Some babies appear male at birth with cryptorchidism •• Congenital adrenal hyperplasia. Defects leading to the development of female pseudohermaphroditism are deficiency of 21- and 11-hydroxylase, as well as 3--hydroxysterone dehydrogenase •• The influence of maternal androgens and progestin. As the potential danger to the developing fetus of drugs taken by the mother during pregnancy is realized, androgenic drugs are becoming an increasingly rare cause of female pseudohermaphroditism. Occasionally, the development of this pathology may be caused by a virilizing tumor or maternal illness during pregnancy. Careful collection of anamnestic data (pregnancy course, including drug intake and diseases) is necessary.
• Congenital defects of the external genitalia : hypospadias and microphallia •• Hypospadia of varying severity is recorded in isolation or in combination with other congenital defects, especially of the genitourinary system •• Microphallia. Boys' genitals are small, but well differentiated. There are standards for assessing the length of the erect penis, from early childhood to adulthood. Genital growth is determined by hormonal stimulation of the fetal testicles with pituitary gonadotropin ••• Etiology. Microphallia (penile hypoplasia) may indicate postnatal hypogonadotropic hypogonadism (as in Kallmann syndrome) or may reflect congenital hypopituitarism ••• Treatment. An effect can be expected from the use of testosterone (25–50 mg every 3 weeks for 3 months), which leads to a positive cosmetic effect without significantly accelerating skeletal maturation.
Management of a child with bisexual genitalia • A full diagnostic evaluation should be undertaken as soon as possible after the birth of a child with bisexual genitalia. It is necessary to convince parents to postpone giving the child a name and attributing gender until the end of the diagnostic measures. Needed: a thorough collection of family history, details of the course of pregnancy, general examination •• Examination. The size of the penis, the location of the urethra, the presence of palpable gonads (usually testes) and other signs (dysmorphic and asymmetric) should be assessed •• Laboratory studies include: chromosomal analysis, determination of electrolytes, testosterone, LH, FSH and 17-hydroxyprogesterone. Radiographic contrast examination of the urogenital sinuses often helps to detect the vagina and cervix, and sometimes it is possible to examine the fallopian tubes. Ultrasound of the pelvic organs can reveal the presence of the ovaries and uterus ••• With a karyotype of 46.XX and an increased content of 17-hydroxyprogesterone, 21-hydroxylase deficiency is most likely. With normal levels of 17-hydroxyprogesterone, true hermaphroditism is most likely. Assessment of the content of 11-deoxycortisol and dehydroepiandrosterone excludes the possibility of deficiency of 11-hydroxylase or 3-b-hydroxysterone dehydrogenase ••• With a karyotype of 46,XY, assessment of the content of sex and adrenal steroids before and after stimulation with ACTH and hCG allows us to identify rare forms of congenital adrenal hyperplasia and disorders synthesis and metabolism of testosterone ••• If glucocorticoid deficiency (including salt loss) is suspected, children should be closely monitored until test results are obtained ••• The diagnosis of partial androgen resistance depends on family history. High testosterone levels in newborns with elevated LH levels suggest androgen resistance.
• Gender assignment . To resolve many therapeutic and general issues, an accurate diagnosis is necessary •• Even noticeably virilized girls with 21 hydroxylase deficiency should be raised as girls, since with adequate treatment of the disease and cosmetic restoration of the external genitalia, they will have full reproductive capabilities •• For boys with a karyotype of 46, XY and bisexual genitalia, sex determination must be based on the decision of the ability to perform sexual functions as a man. This usually depends on the size of the penis and the surgeon's assessment of the possibility of surgical correction of hypospadias ••• Dysgenetic testicles and ovarian-testes should be removed, since the likelihood of their malignant transformation is high ••• To avoid unwanted hormonal influences during puberty, it is necessary to remove the gonads, not corresponding to gender.
• Treatment •• Adequate hormone replacement therapy, as a rule, should be prescribed during puberty •• Genetic counseling (including on issues of sexual behavior) of families and children is an important aspect of medical care •• Full, but tactful information about the results all tests (according to the patient's age) should lead to successful psychosexual adaptation •• Removal of the gonads. Due to possible malignancy, the XY gonad in resistant ovarian syndrome must be removed before puberty or immediately after diagnosis. There is no need to remove the gonads in patients with either Turner syndrome or Kallmann syndrome, since there is no potential for gonadal malignancy; with Turner syndrome hr. There is no Y, but in Kallmann syndrome the chromosomes are normal. Androgen insensitivity syndrome (see Testicular feminization syndrome) is characterized by the presence of type XY gonads; the gonads do not need to be removed before the completion of sexual development, since the risk of developing gonadal tumors is low until the age of 20 •• Sex change is carried out in case of hermaphroditism, as well as at the request of a transsexual, when the patient is convinced that his existing sexual characteristics do not correspond to his gender. After careful preoperative preparation (psychiatrist consultation, hormone replacement therapy), a destructive operation is performed, followed by organ reconstruction using various flaps and skin grafts.
Abbreviations. DHT - dihydrotestosterone, MIF - Mullerian inhibitory factor
ICD-10. Q56 Sex ambiguity and pseudohermaphroditism
Note. Hermaphroditism (from Greek mythology - Hermaphroditos, the son of the god Hermes [Hermes] and the goddess Aphrodite [Aphrodite]; while swimming, he merged his body with a nymph) - the presence of both male and female reproductive glands in an individual (true hermaphroditism) "androgyny" bisexuality • • The term is also (and from a genetic point of view - loosely) used in the meaning: the presence in an individual of characteristics of both sexes (including behavioral) “ambisexuality” bisexuality “bisexuality” intersexism “intersexuality.
17-OH-PROGESTERONE
17-OH-progesterone is a hormone responsible for human reproductive function. Produced in the adrenal glands, gonads and placenta. Indications for the analysis: diagnosis and monitoring of patients with congenital adrenal hyperplasia, hirsutism, cycle disorders and infertility in women; adrenal tumors. Most often, an increase in the level of 17-OH-progesterone is observed with congenital adrenal hyperplasia, tumors of the adrenal glands or ovaries. The level of 17-OH-progesterone is usually reduced in Addison's disease, pseudohermaphroditism in men. Preparation for the study: according to the instructions of the attending physician (in women, blood is usually taken for testing on the 3-5th day of the cycle), on an empty stomach. Our dictionary Galactorrhea is the discharge of milk, colostrum or milk-like fluid from the mammary glands. Amenorrhea is the absence of menstruation for 6 months or more. Oligomenorrhea is a menstrual disorder characterized by a short period of menstruation. Hypogonadism is a pathological condition characterized by underdevelopment of the internal and external genital organs and unclear expression of secondary sexual characteristics. Addison's disease is characterized by insufficient secretion of corticosteroid hormones by the adrenal glands. Symptoms of the disease: weakness, lethargy, hypotension, dark spots on the skin. Hirsutism is increased male pattern hair growth in women along the midline of the abdomen, face, chest and inner thighs. Adrenogenital syndrome (pseudogermaphroditism) is characterized by hyperfunction of the adrenal cortex and increased levels of androgens in the body. Anovulation is a change in the menstrual cycle characterized by the absence of an egg from the ovary. The luteal phase is the second phase of the menstrual cycle, beginning with the moment of ovulation and the formation of the corpus luteum. Duration – 12-16 days. Preeclampsia is a complication of pregnancy in which the function of vital organs, especially the vascular system and blood flow, is disrupted. Cushing's syndrome . The term is used to describe a complex of symptoms (a round, moon-shaped face that becomes reddish in color, fat deposits on the neck).
Results of studies on the size of male penises
Do you want to become a real man!? - Press!
How much should it be in cm?
Research on the optimal length (13.8 cm) in our separate article -
Although research results vary markedly, most experts in the United States agree that the average male penis is approximately 13-15 cm (5.1-5.9 inches) in length. At 95% confidence level this equals 10.7 to 19.1 cm (4.23 to 7.53 inches). The typical girth or circumference at full erection is approximately 12.3 cm (4.85 inches). The average size of a man's penis is slightly larger than his median size. The following results are based on measurements taken primarily in the USA.