Often young women are perplexed: where did the strange lump appear on their hand?
?
Although painless, but quite large (from 0.5 to 6 cm in diameter), it cannot go unnoticed due to its location. So what is hygroma
- cancer or a purely aesthetic defect?
Although hygroma on the arm is a tumor-like formation, it, contrary to misconceptions, is not an oncological disease
, and also
never degenerates into cancer
. This disease is quite widespread (up to 50% of all neoplasms on the hands) and can be successfully treated. On the other hand, this subcutaneous formation can cause discomfort or even interfere with normal blood circulation in the hands.
Hygroma
(or, as it is also called,
ganglion
) is a capsule-bag that is dense to the touch, filled with a viscous and jelly-like protein liquid mixed with fibrin. The hygroma noticeably protrudes over the ligaments and tendons and practically does not move under the skin. Most often, synovial cysts are observed in women aged 20 to 30 years (⅔ of the total number of patients). Children are least likely to suffer from it.
In what cases should you worry about treating hygroma and can it be prevented?
Hygroma - formation in the form of a tumor
What it is
Hygroma (synovial cyst or ganglion) is a formation that is a capsule filled with thick liquid.
This is a benign cyst that mainly forms in the joint area. Most often these tumors appear on the hands. More than half of all neoplasms on the hands are hygromas. The size of the hygroma varies from 0.5 to 6 cm in diameter. Small tumors, as a rule, do not cause discomfort other than aesthetic ones. Large hygromas can be difficult. This is due to pressure on nearby nerve fibers. This leads to pain, which requires prompt medical intervention. Moreover, in approximately 50% of cases, hygromas go away on their own¹.
According to one epidemiological study, hygromas are formed annually in 3 people for every 10 thousand population². In the vast majority of cases, these are persons aged 20-30 years. Hygromas are extremely rare in older people and children. In women, such tumors appear 2-3 times more often than in men.
"Professional" hygromas
Most often, hygromas are formed in athletes who use sports equipment. These are tennis players, hockey players, golfers, weightlifters and others. Musicians, typesetters, painters and turners also often encounter hygroma. Any work associated with high load on a joint (or group of joints) increases the risk of synovial cysts.
When is surgery needed?
Most people with hygroma want a clear answer to this question. However, the doctor cannot answer it. A synovial cyst is not a dangerous disease; it has a chance to go away without any treatment; surgery (like any intervention) has its own possible complications and risks. Whether to operate on a hygroma or not is a patient’s informed decision. When a person understands the situation and is ready to share responsibility for the decision made with the doctor, then one can choose the time and place to perform the intervention.
How is the operation to remove hygroma performed?
I will describe the basic principles using the example of the most common dorsal hygroma on the wrist.
- The operation is outpatient. There is no need to stay in the hospital.
- Local anesthesia. Anesthesia means unnecessary risks, as well as excessive preoperative examination. I use a mixture of lidocaine and epinephrine, this avoids discomfort from the tourniquet, reduces the likelihood of a toxic reaction to the anesthetic and prolongs the effect of pain relief to 4-5 hours.
- Transverse access. Longitudinal access leaves rough, unsightly scars.
- It is imperative to excise the fragment of the joint capsule from which the hand hygroma grows. Only the skin is sutured.
- I don't use immobilization. For the first 2-3 days, a thick soft bandage is applied, which limits movement and makes the early postoperative period as comfortable as possible. Prolonged immobilization after surgery can lead to stiffness, but does not affect the likelihood of relapse.
- The skin heals in about 2 weeks.
Hygroma symptoms
In 30-40% of cases, hygromas are asymptomatic. The only manifestation that worries a person is a compacted lump near the joint. Most often this is the wrist joint or fingers. In other places, synovial cysts appear much less frequently.
Hygromas are rarely large. They grow very slowly and simply do not have time to reach large sizes.
A doctor examines a hygroma. Photo: familylifestyle / Depositphotos
In addition to the pineal formation, other symptoms are also observed with a synovial cyst:
- limited mobility of the affected joint;
- pain in the area of the cyst (usually aching pain);
- decreased or increased sensitivity of the skin (possible slight numbness in the area of the hygroma);
- burning sensation, tingling, crawling and other sensations (arise due to pressure on nerve fibers).
More pronounced symptoms are observed when the hygroma is located under the joint ligament. In this case, a lump above the skin may not form. In this case, the skin over the cyst becomes rough and peels off. Subglottic hygromas often lead to dull and pressing pain. Sometimes the pain spreads to other parts of the limb.
How to distinguish a hygroma from a cancerous tumor
Only a doctor can do this, so if any formations (bumps, bumps, etc.) appear, you need to go to the clinic. Unlike malignant tumors, hygromas can increase and decrease in size. Typically, a synovial cyst shrinks with rest. After exercise, it noticeably increases in volume.
A characteristic feature of hygroma is that the skin above it retains all its properties (color, structure, elasticity). The exception is hygroma growing under the ligament. In most cases, hygromas on the arm remain painless on palpation.
When to see a doctor
You should consult a doctor if a characteristic lump or lump appears.
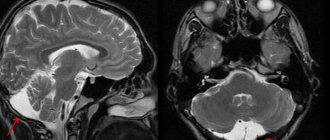
Diagnosis of wrist hygroma using MRI
Magnetic resonance imaging visualizes neoplasms whose size does not exceed 3 mm. If a hygroma of the wrist is suspected, the doctor may prescribe an MRI to clarify the location and size of the cyst.
During the procedure, the patient, lying on a mobile table, is placed inside the tomograph tunnel. The device generates a magnetic field. Sensitive sensors read the signal, which, using a computer program, is converted into a series of photographs of thin sections of the wrist joint and surrounding tissue.
The step width is from 1 mm, which allows you to see the slightest changes in the morphological elements of the articulation in the photographs. The scan is carried out in axial, sagittal and frontal projections; if necessary, the doctor reconstructs a 3D model of the wrist and hand.
Contrast-enhanced MRI is used in the diagnosis of tumors. The patient is injected intravenously with a “coloring” solution that fills the vascular bed and intercellular space in the area of interest. For enhancement, drugs containing gadolinium salts are used. The paramagnetic material is susceptible to the induction field of the tomograph and provides an intense response during scanning.
Cyst on magnetic resonance imaging
MRI of the hand is prescribed when the following symptoms appear:
- discomfort, pain when moving your hand;
- the appearance of a round elastic formation in the wrist area;
- limitation of joint mobility;
- paresthesia of the fingers.
Magnetic resonance imaging is used when other diagnostic methods are insufficiently effective. In case of preparation for surgery, MRI makes it possible to clarify the localization of the process and determine the nature of the intervention. During the rehabilitation period, scanning is used to monitor the restoration of joint functionality.
The study is highly informative in the diagnosis of wrist hygroma, does not carry radiation exposure, and is safe for the patient’s health. Contraindications to MRI are:
- the presence of implanted electromagnetic devices (pacemakers, etc.);
- tattoos on the patient’s body made with metal-containing inks;
- breast implants with magnetic guides.
The presence of metal endoprostheses in the area under consideration leads to the appearance of defects in the images and reduces the reliability of the diagnostic procedure.
Complications
The main danger of hygroma is that it can compress nerve fibers, blood vessels and soft tissues. This occurs when the size of the synovial cyst increases.
When nerve endings are compressed, pain occurs. In most cases it is aching or pressing pain. But there are also cases of acute unbearable pain (it all depends on the affected nerve endings).
When vessels are compressed, trophic disorders develop. In this case, the tissues do not receive enough oxygen and nutrients. In the most severe cases, this causes tissue necrosis (death).
In rare cases, a synovial cyst leads to the following serious complications:
- Thrombophlebitis is inflammation of the vein walls with the formation of blood clots. In this case, swelling forms near the hygroma, and the skin acquires a bluish tint.
- Damage to nerves with their further replacement. In this case, innervation is disrupted. The person experiences various sensations, often tingling or numbness.
- Contractures are a violation of joint mobility.
- Inflammatory joint diseases - bursitis and tendovaginitis.
- Suppuration and sepsis. Such complications arise when the hygroma bursts.
If the hygroma is damaged
This often happens with cysts located on the palmar surface. When performing household work, the hygroma can be damaged. In this case, there is no need to squeeze out the contents of the cyst. Treat the affected area with an antiseptic and apply a sterile bandage. Try to see a surgeon within a few hours.
How dangerous is hygroma? Is it a tumor?
Hygroma is a neoplasm, but does not contain mutated defective cells and cannot degenerate into a malignant tumor. But if the cyst is accompanied by an inflammatory process, then the synovial bursa may become filled with serous,
fibrinous or hemorrhagic exudate. As its quantity increases, unpleasant sensations appear due to the stretched bag and compression of soft tissues, blood vessels and nerves; the process of venous stagnation and neurological pain may begin.
Also, do not forget that a “harmless hygroma” may be a symptom of bursitis or actually be a tumor. Therefore, it is imperative to consult a traumatologist-orthopedic surgeon.
Treatment of hygroma
If the hygroma is small in size and does not cause problems, then you can do without special treatment. The only thing a person needs to do is get tested. You should make sure that it is really a hygroma and not another tumor.
As statistics show, in approximately 33% of cases, hygroma goes away on its own within several months or years (usually up to 6 years). And in 50% of cases, the period of spontaneous resorption of the cyst is 10 years³.
If the hygroma has many chambers, grows relatively quickly, or is a source of pain and inflammation, then it needs to be treated. The most effective way to treat hygroma is surgery. In 8-9 cases out of 10, after removal of the hygroma, no relapse occurs. With conservative treatment, hygromas reappear in 80-90% of cases.
Despite the obvious effectiveness of surgical treatment, doctors did not abandon conservative therapy. Let's look at these methods in more detail.
Conservative treatment
The main non-surgical method of treating hygroma is aspiration puncture. A small puncture is made in the cyst, from which the contents are sucked out using an aspirator or syringe. After this procedure, hormonal anti-inflammatory drugs and sclerosants are injected into the cyst cavity. The latter lead to gluing of the cyst walls and scarring (instead of liquid, the capsule is filled with connective tissue). If the hygroma contains pathogenic bacteria, then antibiotics are also introduced into the cavity.
Some clinics practice physiotherapeutic methods of treating hygroma. These are electrophoresis, magnetic therapy, mud therapy, paraffin baths and others. However, such methods of therapy are ineffective. If you decide to undergo such treatment, be prepared for the fact that it will be ineffective.
Surgery
As a rule, indications for surgical treatment of hygroma are:
- severe pain syndrome;
- contractures;
- rapid growth of the tumor;
- unaesthetic appearance.
If you notice rapid growth of a cyst, contact your surgeon as soon as possible. The larger the size of the hygroma, the more difficult it is to remove. This is due to compression of blood vessels and nerve fibers - it will be more difficult for the surgeon to separate the cyst.
Hygroma removal is a simple operation that is performed under local anesthesia. In case of complex localization of hygroma and/or its large size, general or conduction anesthesia (complete anesthesia of the desired area) is allowed.
Surgical removal of hygroma. Photo: familylifestyle / Depositphotos
When removing a joint hygroma, it is important to remove all cyst cells. Otherwise, there is a high probability of relapse of the disease. After removing the tumor and washing the capsule, a drainage tube is installed to drain the fluid. As a rule, after 1-2 days the tube is removed. A pressure bandage is applied to the patient's wound, and the limb is fixed with a plaster splint. Already on days 7-10, the postoperative wound heals and the patient’s stitches are removed.
ethnoscience
For hygroma, treatment with folk remedies includes compresses with sea salt, ointments based on yolk and vinegar, as well as rubbing the cyst with alcohol tinctures. This treatment is ineffective. This way you will only waste time. This is strictly forbidden, especially if the hygroma increases in size.
Diagnostics
To make an accurate diagnosis, you should consult an orthopedic surgeon. Determining the causes of the disease and treatment methods involves conducting an examination: the doctor must determine the location of the tumor and its size. Of the laboratory tests, only a biopsy will be indicative.
Diagnosis is carried out using:
- MRI or ;
- Ultrasound;
- X-rays;
- If necessary, a puncture of the hygroma is taken.
Types of hygroma
Hygromas can be single or multiple. There are cases when several synovial cysts form in a limited area of the body and then grow together.
Hygromas are classified according to their location on the body. Hygromas of the wrist, hand and fingers are most common. They account for about 90% of all cases. Much less often, such cysts form in the knee (Becker cyst) or ankle joints. Let's take a closer look at these varieties of hygroma.
Figure 1. Localization of hygroma. Image: kjpargeter/freepik.com
Hygroma of the wrist
This is the most common location of a synovial cyst. It is especially noticeable if the wrist joint is flexed. In most cases, such a cyst appears on the back of the joint. But sometimes a hygroma forms on the side or at the base of the palm.
This bump feels like rubber to the touch. On palpation, a springing effect is felt.
Hygroma of the hand
Most often, such tumors occur on the finger or palm. Hygroma of the hand is rarely a cause of concern. In most cases, it is small in size (up to 1 cm). Large hand hygromas can make themselves felt when performing household work.
Hygroma on the finger
In most cases, such hygromas form on the back of the finger near the nail. Such cysts are hard, so they can be mistakenly perceived as bone or cartilage growths.
Hygromas on the palmar side of the fingers are usually larger than those on the back. Because there are nerve fibers running along the sides of this side of the finger, these synovial cysts can be painful.
Hygromas of the lower extremities
Hygromas occur much less frequently on the legs. This most often occurs on the back of the fingers or feet, as well as in the ankle area. If the hygroma is large or located next to nerve fibers, then serious problems arise with wearing shoes.
What modern methods of getting rid of hygroma exist?
Removal of this bubble with a gel-like liquid is possible both from the skin and from the joint. There is a thin camera and special instruments that allow you to look inside the wrist joint through small punctures of 2-3 mm. This procedure is called arthroscopy from the words “arthro” joint and “scopy” to look. Through these punctures you can not only look into the joint, but also perform useful manipulations inside, for example, remove a hygroma. The advantages of the arthroscopic method are smaller scars on the skin, faster rehabilitation, and a relatively lower likelihood of relapse.
Causes
The exact causes of hygroma are unknown. There may be a hereditary component, since cysts form more often in blood relatives. This is due to the congenital weakness of the tissues that form the joint capsule. It is also noted that the cause may be inflammatory diseases of the joints - tenosynovitis, bursitis and others.
Among the factors contributing to the development of hygroma are the following:
- High physical activity. Hygromas often appear in people who work out in the gym.
- Performing monotonous movements. As a rule, these are high loads on the joint associated with a person’s professional activities. For example, typists, assembly line workers and others are affected by the disease.
- Inflammatory diseases. In addition to inflammatory diseases of the joints, these are metabolic disorders, autoimmune and infectious pathologies that affect the joints.
- Injuries and previous surgeries. Hygromas often form after injuries or operations on the hand.
Work associated with increased stress on the joints increases the risk of hygroma. Photo: undrey/freepik.com
Puncture
Hygroma puncture is a quick and safe way to get rid of it. Also, a puncture can be considered as a diagnostic procedure: if you get a gel, it means it’s definitely a hygroma. The probability of relapse after puncture is about 80-90%. Injecting any medications into its cavity does not reduce the likelihood of relapse. It is worth remembering that the entry of steroid hormones (they are sometimes used in the hope of influencing the possible return of hygroma) into the subcutaneous fat or articular cartilage can cause very serious irreversible destruction of these structures.
Prognosis and prevention
No one is safe from hygroma. This tumor can appear even in the absence of the above factors. No specific methods of prevention have been developed for synovial cysts. At the same time, some recommendations can reduce the likelihood of hygroma. These include:
- avoiding injuries and hypothermia of joints;
- timely treatment of inflammatory diseases of the musculoskeletal system (in particular, arthritis, arthrosis and others);
- compliance with safety precautions when playing sports (never neglect warming up before the main workout);
- give your joints rest while working;
- follow the principles of a healthy lifestyle.
Risk factors for the formation of hand hygroma
A retrospective analysis of the medical history of patients with hygroma of the hand made it possible to identify factors that significantly increase the likelihood of this pathology occurring. The most pronounced include the following:
- Professional sports that require heavy loads on the upper limbs;
- Employment in professions involving heavy physical labor: Machinist;
- Loader;
- Masseur;
- Seamstress;
- Hairdresser;
- Storekeeper;
It is very important to reduce the impact of the traumatic factor on the hand to a minimum. To do this, you must follow safety precautions, take regular breaks and use special wrist bandages. If painful sensations, small hygromas, or inflammatory phenomena appear, it is extremely important to immediately seek qualified medical help.
Appearance of hand hygroma
It is quite simple to initially determine the presence of hand hygroma, based on its appearance. The formation is in most cases a spherical protrusion, localized in the area of the carpometacarpal joint. The size of the hygroma can vary from a few millimeters, which are slightly noticeable against the surface of the skin, to 5-6 centimeters.
It is important to note that the presence or absence of changes in the skin depends on the size of the hygroma. With small cysts, the skin has a natural color, and in the case of a large hygroma, the skin over it may have a pale or reddish color, which is associated with a reactive inflammatory process in the area of formation.