Causes of development of lateral neck cyst
A lateral neck cyst or branchiogenic tumor (the name of the disease comes from the Greek word “kystis” - bubble) refers to congenital benign tumor formations, which is a consequence of pathological embryonic development of the fetus. Long-term studies indicate a direct connection with abnormal intrauterine development of the fetus in the early stages of pregnancy.
Already from the fourth week of pregnancy, the formation of the gill apparatus in the embryo occurs, consisting of 5 pairs of cavities or “gill pockets”, gill slits and arches connecting them, involved in the development and formation of the structures of the child’s head and neck. With normal anatomical development of the fetus, the gill pouches gradually become overgrown, but in some cases, they persist and form various types of cysts (lateral, median).
Etiology of the median neck cyst, its clinical manifestations
Cysts in the cervical region are a hollow tumor-like formation enclosed in a capsule located on the anterior surface of the neck. Inside they are filled with liquid or a mass of mushy consistency. The prerequisites for their formation are laid in the fourth to eighth week of embryonic development. Often the problem is combined with a congenital fistula. It also happens that it appears later due to suppuration of the cystic formation.
Most often, median cysts (MCs) are detected in pediatric patients between four and fourteen years of age. They are located between the visceral arches and normally should have disappeared as the fetus developed. This does not happen if there are anatomical anomalies in the development of the arches. The formation of a cyst occurs when the thyroid rudiment moves from the area of formation to the place of its further development: on the anterior cervical surface.
MC accounts for 40% of all cystic formations in the cervical region. At the appointment, the doctor discovers a dense formation with a diameter of up to 20 mm, having clear boundaries, fused to the hyoid bone, and characterized by slight mobility. Sometimes it is localized in the root lingual area: in this case, it is invisible from the outside, but manifests its presence by raising the tongue, speech disorders and difficulties with the act of swallowing.
Purulent processes of KS develop in 60%; they are accompanied by the following symptoms:
- Increasing formation in size;
- Increased pain;
- Swelling and redness of the skin;
- Formation of a fistula when opening an abscess;
The fistula can open directly on the neck or in the oral cavity between the root and body of the tongue, or on its front surface.
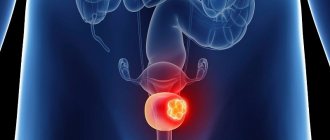
Signs and symptoms of lateral neck cyst
The lateral neck cyst is a painless, round-shaped formation with clear boundaries, having a dense and elastic consistency, which is located in the area of the so-called “carotid triangle of the neck.” As a rule, the skin over the lateral cyst is quite mobile and does not change the color of the skin. Clinical practice shows that lateral cysts can reach significant sizes, which leads to compression in the area of the larynx and trachea and causes not only dysphagia, impaired respiratory function, but also a disorder in human speech. Usually, the presence of a lateral neck cyst does not pose a health risk, but nevertheless, due to the latent form of the disease, a cervical cyst can develop into a malignant tumor.
The early stage of development of a cervical cyst can be extremely difficult to detect. This is due to the fact that there are quite a few other diseases that have similar symptoms. However, there are parameters for the symptoms of the presence of a lateral neck cyst, which manifest themselves as a result of various infectious inflammatory processes or trauma:
- the appearance of a small swelling in the area of the carotid artery; — violation of the swallowing process of food; - pain due to pressure on the neurovascular bundle; - sensation of an elastic, painless neoplasm of a mobile nature upon palpation; - enlarged lymph nodes in the neck; - displacement of the larynx; - impaired breathing and diction, the presence of stridor (a whistling sound when breathing); - suppuration with the formation of an abscess in case of infection of the cyst.
Treatment
Treatment of B. to. and fistulas is only surgical. The operation is performed under endotracheal anesthesia. Special preparation is usually not required.
B.'s excision is performed through a transverse incision. The cyst is carefully dissected (without opening) from the fascial sheath of large vessels. Then the connective tissue cord going deep into the neck is completely isolated. In some cases, this requires the use of an additional incision along the edge of the lower jaw (see below). After removal of the cyst, the wound is sutured in layers.
Rice. 2. Operation of excision of a branchiogenic fistula of the neck (top left - oval skin incision, including the fistulous tract): 1 - through an additional incision at the angle of the lower jaw, the mobilized part of the fistulous tract is removed; 2 - a probe was inserted into the lumen (at the bottom of the figure), through which separation was carried out, and the fistula tract was bandaged.
The operation of excision of a branchiogenic fistula begins with an oval excision of the external opening (Fig. 2). Then the fistula tract is isolated, carefully separating it from the dense adhesions with the sheaths of large vessels of the neck. To facilitate further manipulations, an additional incision is made at the angle of the lower jaw (above the projection of the fistula), where the mobilized part of the fistula tract is removed.
Then a button-shaped probe is inserted into the lumen of the fistula, along which the fistula tract is separated as close as possible to the pharynx, tied with catgut thread and cut off. In case of wide, complete fistulas, their proximal part is turned inside the pharyngeal cavity using a probe, cut off, and the resulting hole is sutured. The wound is sutured tightly.
In the postoperative period, broad-spectrum antibiotics and physiotherapeutic procedures (UHF currents) are prescribed for 5-6 days. The sutures are removed on the 8-9th day. Children need clinical observation for 6-12 months, since relapses may occur if the operation is not radically performed.
Bibliography:
Abrikosov A. Particular pathological anatomy, p. 81, M., 1947; Bairov G. A. Congenital cysts and fistulas of the neck, in the book: Surgery of developmental defects in children, ed. G. A. Bairova, p. 94, D., 1968; Vsiglovsky R.I. About lateral (so-called branchial) fistulas and cysts of the neck, Proceedings of the 7th Congress of Russian Surgeons, p. 191, St. Petersburg, 1908; Lurie T. M. and Molokov S. A. To the surgical treatment of congenital fistulas and cysts of the neck, Surgery, No. 3, p. 63, 1961, bibliogr.; Orlov V. S. On the method of surgical treatment of lateral fistulas of the neck, Vestn, hir., t. 101, No. 10, p. 118, 1968; he, On the method of fistulography for congenital lateral fistulas of the neck of great length, in the same place, t. 100, No. 2, p. 28; Bhaskar S.N. a. Bernier JL Histogenesis of branchial cysts, Amer. J. Path., v. 35, p. 407, 1959; Сaffey J. Pediatric X-ray diagnosis, Chicago, 1967; Kaufmann E. Lehrbuch der speziellen pathologischen, Anatomie, Bd 2, T. 3, S. 1488, B., 1960; Little JW a. Rickies NH The histogenesis of the branchial cyst, Amer. J. Path., v. 50, p. 533, 1967; Meyer HW Congenital cysts and fistulae of the neck, Ann. Surg., v. 95, p. 226, 1932.
G. A. Bairov; I. M. Vertkin (pat. an.), G. M. Zemtsov (rent.).
Diagnosis of lateral neck cyst
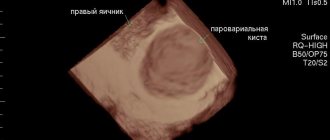
To confirm the diagnosis of “ lateral neck cyst ,” a differential approach to medical examination is required using modern diagnostic equipment - computed tomography, ultrasound, and, if necessary, puncture.
As a rule, the diagnosis of a lateral neck cyst is performed if the patient has a complication in which a noticeable increase in the size of the cyst, phlegmon or a characteristic abscess is already observed. When diagnosing a neck cyst, it is very important to exclude other diseases in the neck area that have similar manifestations and similar symptoms. A branchiogenic cyst can be differentiated from the following neck diseases: neck lipoma, lymphosarcoma, lymphangioma, neck teratoma, lymphadenitis, including the nonspecific tuberculous form, glomus tumor (vagus nerve), branchiogenic carcinoma, metastases from thyroid cancer.
Diagnosis of a lateral neck cyst consists of the following steps:
- complete collection of medical history, including hereditary factors; — external examination with palpation of the neck and lymph nodes; — computed tomography of the neck with contrast to clarify the size of the tumor, its location, type of fistula, contents of the cavity; — Ultrasound of the neck; — cyst puncture (according to indications); - fistulogram or staining of the fistula tract.
Diagnostics
Before proceeding with surgical treatment of a cyst on the neck, it is very important to undergo diagnostics. First of all, the doctor will take a medical history: find out how long ago you noticed the cyst, what symptoms bother you. Then the doctor will examine the neck and palpate the tumor.
Additionally, the following types of diagnostics may be prescribed:
- Puncture of the cyst to collect exudate - this is necessary for histological examination;
- Ultrasound examination of the neck - it is used in case of insufficient data or if any complications are suspected, CT or MRI may be additionally prescribed.
If surgical intervention is necessary, additional studies are prescribed to exclude contraindications to surgery: general and detailed blood and urine tests, fluorography, electrocardiogram, etc.
Treatment of lateral neck cyst
Treatment of a lateral (branchiogenic) cyst is carried out only surgically. To avoid complications, the development of inflammatory processes and suppuration, surgery to remove the cyst should be performed as early as possible. Nowadays, operations for radical dissection of the cyst are not complex surgical interventions, but require high professionalism, attention and experience, since the remaining particles of the neoplasm epithelium can subsequently cause a relapse with subsequent surgical treatment.
These operations are performed under endotracheal anesthesia (tracheal intubation), the duration of the operation is from 30 minutes to one hour, depending on the location of the tumor, the age of the patient and the complexity of the case. At the end of the operation, the patient is given antibacterial and anti-inflammatory treatment. Physiotherapeutic procedures and UHF. Five to seven days after surgery, the sutures are removed. To exclude relapse, the patient is under clinical observation for one year.
After operation
As a rule, after surgery, the patient is required to remain in a hospital setting for 1-2 days under the close supervision of medical workers. If the patient feels well and there are no complications, the patient is discharged home. The rehabilitation period is 2-3 weeks. During this time, it is prohibited to take hot baths, visit the bathhouse, sauna, etc. To exclude complications, the doctor may prescribe antibacterial or anti-inflammatory therapy. A month after the operation, a control ultrasound is required.
Take care of yourself - consult a doctor at the first suspicion of a neck cyst! The doctor will determine treatment tactics and give recommendations for observation and lifestyle. Be healthy!
Features of the development of cervical cysts and treatment in childhood
Lateral neck cysts in newborns and young children occur in a latent form and are not expressed by clinical symptoms until a provoking factor appears - trauma to the child, the appearance of a respiratory infection or other inflammatory processes. Sometimes hormonal changes in the body can become such a factor.
Clinical practice shows that in children the formation of a lateral cyst is always preceded by acute respiratory infections, influenza and other diseases of the upper respiratory tract. There is a connection between the tumor and the lymphatic tract, during which microbes of a pathogenic nature penetrate into the internal cavity of the cystic formation, causing suppuration.
In childhood, surgical treatment of a lateral cyst is carried out from three years of age outside the acute stage. But in case of serious complications leading to a threat to life, surgical intervention is indicated at an early age of the child.
Median neck cyst, median neck fistula, lateral neck cyst and lateral neck fistula in children.
Author: Ph.D. Stepanenko N.S.
Cysts and fistulas of the neck in children are usually represented by several types of congenital anomalies or space-occupying formations of a benign nature. Pathology of the development of the Thyroglossal duct is a median cyst of the neck or a median fistula of the neck. Anomaly in the development of branchial arches – branchiogenic fistulas and cysts – lateral neck cyst and lateral neck fistula. Median neck cyst, median neck fistula, lateral neck cyst, lateral neck fistula are congenital developmental anomalies that require surgical treatment.
- Anomalies of the branchial apparatus (lateral neck cyst, lateral neck fistula in children).
Anomalies of the bronchial apparatus include heterogeneous groups of congenital pathology resulting from incomplete intrauterine cleavage of the pharyngeal slits and pouches. Fistulas, cysts, sinuses and cartilaginous remnants are clinical manifestations of remnants of the embryoanal branchial arches.
All these anomalies appear immediately after birth, but many of them do not manifest themselves clinically for a long time. Spontaneous mucous discharge from the external opening is often the first sign of a lateral neck fistula in a child. The first clinical manifestation of a lateral cyst and lateral neck fistula in children may also be infection of the cyst or fistula tract, as a consequence of the fact that thick mucus is not able to drain spontaneously on its own, and bacteria begin to actively multiply in it.
Diagnosis of lateral cyst and lateral fistula of the neck in children.
The most common sign of a neck fistula is mucous discharge from a small hole, which can be located anywhere along the anterior edge of the sternocleidomastoid muscle, as well as on the face and subclavian region.
Although there are methods for probing the fistula tract with the introduction of dyes and radiopaque substances, however, from our point of view, their use is not justified, especially in young children. The information content and reliability of these methods for diagnosing a lateral cyst and lateral fistula of the neck in children is low, but it causes painful discomfort to the child and can cause the fistula to become infected. Anamnesis, a detailed examination and knowledge of the embryology of this pathology are quite sufficient for diagnosis and proper treatment.
Treatment of lateral cyst and lateral neck fistula in children is only surgical.
The goal of treatment for this anomaly is complete excision of the cyst and/or fistulous tract to the base and ligation at the base. From a technical point of view, the results of treatment of lateral cyst and lateral neck fistula in children are always better if the formation is removed before it becomes infected (easier to remove, less cosmetic defect after surgery and lower likelihood of recurrence). If at the time of treatment there is an ongoing inflammatory process, then the focus is drained and antibacterial therapy and local treatment are prescribed. Only after the inflammatory process has subsided is surgery performed. Surgical intervention after an inflammatory process or against the background of chronic inflammation of the lateral cyst and lateral fistula of the neck in children is more complex, due to the adhesive process and the disappearance of normal anatomical landmarks, which, according to statistics, leads to an increase in the% of relapse. That is why surgical intervention for a lateral cyst and lateral fistula of the neck in children is not contraindicated at an early age and indications for surgery are formed from the moment of detection, in order to perform surgical intervention before the occurrence of inflammatory complications.
The operation is performed under general anesthesia and usually requires endotracheal intubation. The surgeon uses 3-4x optical magnification, which makes it possible to visualize absolutely all structures even in infants and avoid damage to the nerves and perform radical removal of the fistulous tract to the base.
A bordering incision is made around the fistula opening. Next, complete isolation of its course, bandaging and cutting it off at the base. It is very important to avoid rupture of the fistula and complete removal of its tissue, which is necessary to prevent relapse. In some cases, when the fistula is long, two incisions are required.
- Thyroglossal cysts (median neck cysts, median neck fistulas in children).
The embryogenesis of thyroid cysts (median neck cyst, median neck fistula) is directly related to the development of the thyroid gland, hyoid bone and tongue. The development of the diverticular rudiment of the thyroid gland occurs in the area of the future blind foramen of the tongue, between the 4th and 7th weeks of gestation. As the tongue develops, the thyroid diverticulum descends into the pretracheal space onto the neck, but continues to be associated with the foramen cecum. At the same time, the hyoid bone arises from the 2nd branchial arch. As a result of these several simultaneous processes, the thyroglossal duct may appear anterior or posterior to the hyoid bone, but most often passes through it. Normally, the duct disappears by the time the thyroid gland reaches the surface of the neck. Cysts can appear anywhere along the path of migration of the thyroglossal duct to the neck, if the process of its descent for some reason stops and the duct is not obliterated.
Detection of thyroglossal duct cysts (median neck cyst, median neck fistula in children) is sometimes more difficult than anomalies of the branchial apparatus. They are located deep, in the thickness of the soft tissues of the neck. As a rule, they are discovered at an older age, since due to the pronounced subcutaneous fat in infants, identifying a median cyst in the neck of the cyst is very difficult. Connecting to the oral cavity through the blind foramen, median cysts in children can become infected with microbial flora from the oral cavity. Some children may experience an unpleasant taste in the mouth due to spontaneous drainage of the cyst contents into the oral cavity. As in the first case, examination, anamnesis and palpation are sufficient to establish a diagnosis. Sometimes, in more complex cases, ultrasound can be used.
Differential diagnosis of a median neck cyst in children is carried out with adenopathy, cystic hygroma, tumors of the lymphatic tissue, disease of the thyroid and parathyroid glands.
Treatment. Treatment of median neck cyst and fistula in children is only surgical. Surgery is indicated to prevent infection, as well as a small possible risk of malignancy of the cyst (1%). In some cases, surgery is indicated due to negative sensations in the area of the cyst, pain, or a sharp increase in the volume of the median neck cyst in a child. The inflammatory process often occurs in children against the background of ARVI, which also causes earlier surgical intervention, that is, before the child starts attending kindergarten and school.
Surgery for a median neck cyst in a child is performed under endotracheal anesthesia. An incision is made along a fold of skin on the neck, at the border with the area of the diaphragm of the oral cavity. That is, the highest point on the neck, which allows you to achieve an ideal cosmetic result - such a seam is practically invisible. The cyst tissue is very different from other tissues, but may be closely related to them. In 1920, Sistrunk proposed excising the central part of the hyoid bone along with the cyst as a necessary component of the intervention aimed at preventing relapse. Further studies confirmed the need for partial resection of the hyoid bone. It is in this variant that surgery is currently performed for a median cyst of the neck in a child. After removing the head of the hyoid bone, the muscles are brought together and sutured with non-absorbable sutures. Sometimes it is necessary to install a safety drain.
Complications and relapse rates. The main difficulty of surgical intervention for a median cyst of the neck and a median fistula of the neck is the localization of the pathology. The neck is the most anatomically complex area, with a huge number of vessels and nerves running from the head to the entire body. All surgical interventions on the neck are performed using optical magnification, with a clear view of the anatomy of the neck and submandibular region. An infrequent but serious complication is bleeding from the wound surface, which can lead to the formation of a hematoma and compression of the respiratory tract. To prevent this, careful hemostasis and installation of safety drainage are necessary. Cases of damage to the cartilage of the larynx, thyroid gland and nerves have also been described.
The recurrence rate of median neck cyst in children averages 2-8%. In the department of Children's City Clinical Hospital No. 13 named after. Filatov, we achieved a reduction in the percentage of relapse to 1.5%, which is a very good result. Relapses are more common in children after repeated surgery and against the background of an inflammatory process. It usually appears during the first year after surgery. Basically, relapse of the median neck cyst and median neck fistula is associated with incomplete removal of pathological tissue, inadequate resection of the head of the hyoid bone. In rare cases, there are several fistula ducts, the detection of which is very difficult. Relapses after the second operation occur much more often, from 25% to 30%.
3. Dermoid and epidermoid cysts of the neck.
From an embryological point of view, dermoid cysts are ectodermal elements located under the skin. Dermoids contain sebaceous glands, hair follicles, connective tissue and papillae. Inside the cystic cavity of both dermoids and ectodermoids there is sebaceous content. Most often, dermoid cysts in children are located on the face, but they can also be located on the neck. These cysts may be mistaken for midline cysts of the neck. However, the dermoid is located more superficially and is not connected to the hyoid bone or other cervical structures.
The treatment of choice is their excision.
Surgical video:
Webinar on neck cysts:
Prognosis for treatment of lateral neck cyst
The prognosis of a lateral neck cyst depends on the following factors:
- general health of the patient; - age; - the size of the cyst and its localization in relation to important organs and large vessels; — duration of cyst development; - forms of cysts - inflammation, suppuration; - contents of the cavity - pus or exudate; - type of fistula; - presence or absence of chronic diseases.
In general, the prognosis for treatment of a lateral neck cyst can be considered favorable. The risk of a lateral cyst degenerating into a malignant form is extremely low.
Preoperative period:
Removal of a neck cyst is performed under general anesthesia . In order to identify possible contraindications to anesthesia before surgery, the patient undergoes a simple preoperative examination. Standard preoperative examination includes clinical and biochemical blood tests, blood clotting tests, determination of blood group and Rh factor, blood tests for hepatitis B and C, HIV, syphilis; general urinalysis, ECG. On the day of surgery, the patient is examined by an anesthesiologist.
Is there a way to prevent branchiogenic cervical cysts?
Unfortunately, there are no preventive measures to prevent the development of this disease due to its nature of abnormal intrauterine conception. Most likely, this is a question for geneticists dealing with the problems of the etiology and pathogenesis of congenital anomalies of embryonic development. But, if a lateral cyst is nevertheless identified, then dynamic observation is recommended for children up to three years of age with periodic examinations every 3 months. Children should undergo regular medical examinations with a mandatory examination by an ENT doctor who can monitor the development of the tumor and eliminate various risks and complications.
Types of neoplasms
Damage to the skin as a result of cell proliferation forms compactions of various types and sizes: from a pea to a walnut. Depending on the nature of the pathology of the formation, there are:
- benign;
- malignant;
- borderline (precancerous).
The formations cause physical and aesthetic discomfort to the child, but the main danger is their degeneration from a benign tumor to a malignant one. Only a doctor can determine the nature of the formation under the skin.
In this regard, we note that in addition to the otolaryngologist, solving problems of this kind may involve visiting other highly specialized specialists. Depending on the etiology and nature of the seals, treatment can be carried out by a dermatologist, surgeon, endocrinologist and oncologist. If necessary, the ENT doctor will refer the patient to the appropriate specialist.
Clinical case in the larynx department of the Federal State Budgetary Institution National Medical Research Center of the Federal Medical and Biological Agency of Russia
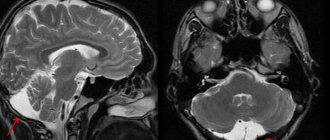
Patient M. , 26 years old, on June 20, 2016, sought medical help from specialists from the Department of Laryngeal Diseases of the Federal State Budgetary Institution National Medical Research Center for Medical and Biology of the Federal Medical and Biological Agency of Russia with a complaint about the presence of a mass on the right side of the neck. According to the patient, the formation appeared in September 2015, and gradual growth was noted. After an MRI examination and ultrasound of the neck, a diagnosis of “lateral neck cyst” . On the right side of the neck, the contours of the cyst are visualized from the mastoid process of the temporal bone to the clavicle; upon palpation it is dense, the surface is smooth.
View of the patient's neck before surgery | MRI images of patient M. | |
On June 21, 2016, the patient underwent removal of a benign neck tumor.
Surgery to remove a lateral cyst in patient M. | ||
Size of removed tumor: 20 cm by 6 cm
In the postoperative period, patient M. received antibacterial therapy, the suture was removed on the 7th day.
She was discharged on June 29, 2016 with improvement.
Photo of the patient immediately after surgery | Photo of the patient upon discharge |
Fibromas, papillomas, atheromas, etc.
Removal of fibromas, papillomas, and atheromas is performed either surgically - through a minimal skin incision, or using a laser.
In some cases, a combination of surgical and laser treatments is required. During surgical removal of the formation, a cosmetic intradermal suture is applied, after which the scar is almost invisible.
Duration of the operation: half an hour. Pain relief: local anesthesia. Immediately after the procedure, you can begin your normal daily routine. Removal of sutures (in case of surgical removal) 7 days after surgery.