Phlegmon: what is it?
Cellulitis is an accumulation of purulent masses that affect fatty tissue and quickly spread to tendons, muscle and bone tissue.
Sometimes phlegmon is called erysipelas, but these diseases have significant differences.
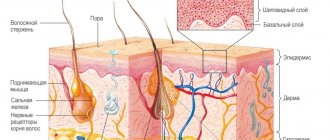
Phlegmon is a diffuse inflammation of the subcutaneous tissue. The affected area is red, hot, painful on palpation. Erysipelas is an acute inflammation of the skin.
Cellulitis is most often caused by group A streptococci and Staphylococcus aureus. Erysipelas is caused by group A streptococci and can spread to the subcutaneous tissue (phlegmonous erysipelas).
Why does phlegmon occur?
The causative agent of the inflammatory process in fatty tissue is Staphylococcus aureus, which enters the body through wounds and abrasions on the surface of the skin that were not promptly and correctly treated. In addition to Staphylococcus aureus, other pathogenic microorganisms, including streptococci, can provoke the accumulation of pus.
Depending on the virus that caused the inflammation, phlegmon can have a rapid incubation period (up to 1 day) or develop over a long period of time, over several weeks. The greatest danger to humans is erysipelas, caused by the penetration of anaerobic bacteria into the body, the life cycle of which takes place without the participation of oxygen. Ways of introducing pathogenic viruses are animal bites, injections with fish bones during cooking. Cellulitis has a chronic form when infected with diphtheria or paratyphoid bacillus. This type of purulent inflammation is rare.
submandibular phlegmon
What is phlegmon - an independent disease or a symptom? The accumulation of pus on fatty tissue can occur independently, but in some cases it is a consequence of other inflammatory processes. In certain situations, phlegmon develops due to the breakthrough of purulent foci in the oral cavity, when pus penetrates into the soft tissues during the rupture of an abscess or carbuncle (for example, phlegmon of the shoulder).
Not every person develops phlegmon when pricked with a fish bone or an animal bite. The state of the immune system plays an important role. Excessive consumption of alcoholic beverages, drugs, and the presence of chronic diseases (especially diabetes) are factors that increase the risk of an inflammatory process. People diagnosed with HIV, AIDS, tuberculosis, and diseases of the circulatory system are at risk.
Classification
The classification of phlegmon is based on several characteristics, according to which the following types of phlegmon are distinguished.
- Along the way: acute and chronic phlegmon.
- By location: superficial (the pathological process affects tissues up to the muscle layer) and deep (the pathological process affects tissues deeper than the muscle layer, fatty tissue).
- According to the nature of the exudate: serous-purulent phlegmon , purulent , purulent-hemorrhagic phlegmon and putrefactive .
- By localization: subcutaneous, intermuscular, subfascial, interorgan, organ, retroperitoneal, pelvic, phlegmon of the hand and foot, phlegmon of the neck, phlegmon of the maxillofacial region, phlegmon of the armpit, etc.
- By origin: primary (develops when the pathogen enters the tissues of the body directly) and secondary (occurs when pathogens migrate from other purulent areas).
Types of inflammation
Depending on how and why phlegmon arose, inflammation can be primary and secondary. The primary type of phlegmon is an independent disease that occurs due to the penetration of pathogenic microflora into the body, the development of which is accelerated against the background of a weak immune system. Secondary phlegmon occurs as a result of the spread of purulent masses through the soft tissues of internal organs due to a burst boil, abscess and other accumulations of purulent masses.
The incubation period, signs and possible complications depend on the type of soft tissue destruction. There are several types of phlegmon - serous, putrefactive, necrotic and purulent. This type of inflammatory process with the accumulation of purulent masses can spread throughout the body, forming on the muscles, in the abdominal cavity, between internal organs, and under the skin. There is phlegmon of the shoulder, foot, and neck.
Each erysipelas has its own name, depending on its location. It consists of two words - the prefix “para”, which means “about”, and the name of the organ in Latin, in the soft tissues of which inflammation has occurred. For example, phlegmon on the tissues of the rectum is paraproctitis, accumulation of pus between organs in the pelvis is parametritis. An abscess that occurs on soft tissues near the kidneys is paranephritis. The cause of phlegmon on the kidneys is untreated infectious diseases of the genitourinary system, which were accompanied by inflammatory processes.
In the absence of timely treatment in the early stages of the development of purulent inflammation, phlegmon can spread throughout the body, affecting the soft tissues of not only internal organs, but also the thighs, legs, perineum, upper and lower extremities.
How inflammation manifests itself
The symptomatic picture of phlegmon depends on its type. Chronic inflammation does not have pronounced signs in the first stages of development and does not particularly bother a person until the purulent masses have fully matured. In acute phlegmon, symptoms increase quickly, the incubation period lasts no more than a day:
- a sharp increase in temperature up to 40°C;
- fever and chills;
- Strong headache;
- prostration;
- constant feeling of thirst;
- enlarged lymph nodes;
- muscle pain;
- aching joints.
phlegmon of the leg.
The place where purulent masses accumulate, for example, if it is phlegmon of the shoulder, begins to rapidly swell and turn red. Any movement of the limb brings pain, at first slight, and with the development of inflammation the patient is no longer able to move his arm due to severe pain. Upon palpation, phlegmon is easily palpable. The accumulation of purulent masses is a solid, hot formation that does not have clear boundaries. The skin over the site of inflammation begins to become shiny.
As soon as the phlegmon matures, the inflammation bursts. Pus may come out in the form of a fistula (better known as a boil). The danger is erysipelas, when ruptured, the pus does not come to the surface of the skin, but penetrates deeper, spreading to the internal tissues of neighboring organs, causing destruction of the muscular system and bones. With internal infection, the patient experiences:
- severe weakness;
- blood pressure rises;
- shortness of breath, chills, internal heat occurs;
- the condition is rapidly deteriorating;
- pressure drops;
- the pulse is weakly palpable;
- headache increases;
- kidney function is impaired;
- the amount of urine decreases significantly.
In particularly severe conditions, the fingers on the upper and lower extremities turn blue, the skin becomes yellowish due to liver dysfunction.
Forms of inflammation
With the development of phlegmon, the inflammatory process goes through several stages of formation. The initial stage is serous. With serous phlegmon, fluid—exudate—forms and accumulates under the skin, and leukocytes penetrate into the cells of the adipose tissue. Fatty tissue takes the form of jelly, completely saturated with exudate. There is a gradual spread of inflammation to healthy areas of soft tissue. If treatment is not carried out at this stage, the phlegmon passes into the next stage, putrefactive or purulent. It depends on what type of pathogenic microflora led to inflammation.
The purulent form provokes histolysis (in which the tissues melt and fill with pus). Due to histolysis, fluid begins to accumulate and may be greenish, cloudy white or yellow. The purulent type of neoplasm can lead to ulcers and fistulas. Without timely treatment, inflammation of purulent masses spreads to healthy tissue, cartilage and bones. At this stage of development of the inflammatory process, the muscles become loose, completely surrounded by pus, and appear gray and dirty. There is no internal bleeding.
The putrefactive form of phlegmon is characterized by rapid infection of soft tissues, which begin to deteriorate, and an unpleasant odor emanates from them. The tissues become brownish or greenish, their consistency is slippery and loose. With further development of phlegmon, soft tissues turn into a solid liquid mass. The main symptom of the putrefactive form of inflammation is severe intoxication of the body with a rapid deterioration in the patient’s condition.
Necrotic phlegmon is the death of destroyed soft tissues that are completely affected by purulent masses. If the tissues do not melt on their own, the body begins to reject them. At this stage of development of phlegmon, the inflammatory process begins to localize, multiple foci of abscess are formed, which can be opened independently. If there is too much accumulation of purulent masses that are deep under the skin, it is necessary to surgically open them and install drainage.
Anaerobic is the most severe stage of phlegmon, in which purulent masses infect adjacent healthy tissues, leading to their death, and gas is released. The fabrics have a fetid odor and are dark gray in color. If you press on the phlegmon, you can hear a crunch with which gas bubbles burst. The skin surrounding the source of inflammation becomes soft and loose, there is no redness.
Possible complications
Cellulitis is an extremely dangerous condition of the body, which without proper treatment can lead to severe intoxication and death of large areas of soft tissue. Chronic phlegmon is characterized by the absence of pronounced symptoms. The slow growth of pathogenic microflora allows the body to fight inflammation. During an exacerbation, a thickening occurs under the skin caused by the accumulation of infiltrate, which becomes woody. The skin around the inflammation becomes bluish.
The development of phlegmon on the lymph nodes is especially dangerous. This condition is fraught with the development of blood clots and sepsis. If the inflammatory process has not been completely treated and a small amount of pus remains on the soft tissues, a repeated purulent abscess may occur. Cellulitis that occurs on the face can lead to purulent meningitis.
cellulitis of the century
With further development of phlegmon, during which healthy tissues are affected, purulent arthritis, pleurisy, and osteomyelitis may occur. The most severe complication is the development of purulent arteritis, in which inflammation of the walls of large blood vessels - arteries - occurs, as a result of which the vessel begins to stratify and disintegrate. This pathological process can lead to severe internal bleeding.
Therapy methods
Cellulitis is a dangerous disease that in advanced stages can cause severe internal bleeding. In some cases, when intoxication of the body occurs with dissection of the arteries, phlegmon can cause death. Before treating phlegmon, it is necessary to determine its type and stage of development. The main diagnostic methods are palpation of the inflamed area, studying the patient’s medical history, questioning him about complaints and symptoms. In some cases, a blood test is necessary, which will show the severity of the inflammatory process by the number of leukocytes in the biological material.
To date, the only method of treating phlegmon is a surgical operation, during which the inflammatory focus is opened and all the contents are taken out. To prevent the formation of a secondary abscess, the pus is thoroughly cleaned from the wound. Surgery can only be avoided if you consult a doctor in a timely manner, at the initial stage of phlegmon formation.
The early stage of a purulent inflammatory process is treated with heat compresses and special ointments that promote the formation of one focus for the pus to escape. Heating pads are used as thermal compresses, and mercury ointment is applied to the affected area of the skin (bandaging according to the Dubrovin method).
In some cases, an additional therapeutic method is used to speed up the process of pus coming out - UHF therapy. UHF is ultra-high frequency therapy, which involves exposing inflamed areas to a magnetic field. Using UHF therapy and applying mercury ointment simultaneously is strictly prohibited.
Removing cellulitis
A mature inflammatory focus, which begins to spread to adjacent healthy tissues, must be immediately removed surgically. The main indication for surgery is an increase in body temperature; in such cases, erysipelas must be removed in the initial stages. Incision of the lesion with pus with further installation of drainage helps to immediately reduce inflammation, relieve tissue swelling, and relieve symptoms of intoxication of the body.
The operation to open the phlegmon is carried out only using general anesthesia, with a cavity incision made in the skin. To completely extract the contents, the doctor needs to deeply dissect both the superficial and deep tissues. When all the pus is removed, the resulting cavity in which the abscess was located is thoroughly washed with special antiseptic solutions, and drainage is installed. It is a rubber tube that can have different diameters and lengths depending on the depth of the wound.
After removing the pus and installing drainage, the wound is covered with a bandage, onto which a hypertonic solution or ointments that dissolve with water and contain antibiotics (Levomekol, Levosin) are applied. It is not recommended to use ointments that have a Vaseline base and are intended to bring pus to the surface (Vishnevsky ointment, Tetracycline ointment) immediately after surgery, as they prevent the outflow of wound contents.
List of sources
- Fomichev E.V., Robustova T.G. Diagnosis and treatment of atypically current purulent-inflammatory diseases of the maxillofacial area. Russian dental journal. 2003; 4: 18-20.
- Purulent-inflammatory diseases of the head and neck. Etiology, pathogenesis, clinical picture, treatment. /Ed. MM. Solovyova, O.P. Bolshakova, D.V. Galetsky - M., MEDpress-inform., 2021.
- Abscesses, phlegmons of the head and neck. / Ed. Solovyova M.M., Bolshakova O.P. - St. Petersburg: KN, 1997.
- Fedorov V.D., Svetukhin A.A. Selected course of lectures on purulent surgery. M. 2007. 365 p.
- Gostshtsev V.K. Guide to purulent surgery. M.: Medicine, 1996, - 300 p.
Rehabilitation therapy and rehabilitation
After surgical opening of the phlegmon, ointments, antibiotics and therapeutic techniques are prescribed that help remove residual pus from the wound and quickly cleanse the skin. Among products with herbal ingredients, preference is given to sea buckthorn oil, rosehip extract and Troxevasin ointment. If the wound does not heal for a long time and the skin does not tighten, the patient is prescribed dermoplasty.
Dermoplasty is a skin graft that is performed in case of severe damage to the dermis during trauma and extensive surgery. When removing phlegmon, this operation is prescribed in the case of removal of extensive inflammatory foci in which soft tissue necrosis has begun. In addition to the use of local remedies that promote rapid recovery and healing of the wound, the patient is prescribed conservative treatment methods aimed at restoring the immune system, relieving intoxication and preventing re-inflammation.
Bed rest is mandatory throughout the entire rehabilitation period. The area of the body where surgery was performed should be in a slightly elevated position. If there is pain, painkillers are prescribed and injected into the muscle.
All patients who have undergone surgery to remove cellulitis must take a course of antibiotics. The medications are prescribed by the attending physician depending on the individual characteristics of the patient and the type of virus that provoked the inflammation. If anaerobic cellulitis has been removed, intramuscular injections of anti-gangrenous serum are prescribed. To restore and normalize the acid-base balance, a solution of methenamine is prescribed. To restore tone to the walls of blood vessels, calcium chloride in solution is used.
To relieve the effects of intoxication and restore the functioning of the heart muscle and circulatory system, adonylene and caffeine are prescribed. Patients need to adhere to proper nutrition, it is imperative to exclude fatty and fried foods, and it is not recommended to consume large amounts of flour. Be sure to drink plenty of plain water; fruit compotes and fruit drinks are allowed to restore the immune system. Antibiotics are used until the inflammatory process is completely removed.
Prevention methods
Cellulitis, like any other disease, can be prevented. It is especially important to follow preventive measures for people who are at risk, with medical diagnoses such as HIV, AIDS, tuberculosis, and diabetes. The main prevention is to prevent skin injuries.
If there are purulent foci in the body, especially in the oral cavity (caries, purulent abscesses on the gums), they must be treated in a timely manner, preventing further development and rupture of purulent foci. If the skin is injured, the cut sites must be immediately treated with antiseptic solutions. You need to be especially careful when preparing fish. A bone injection can lead to the development of erysipelas, which, against the background of a weakened immune system, carries the risk of phlegmon formation.
Considering the rapid development of purulent inflammation, it is necessary to consult a doctor immediately if the skin at the site of the cut becomes red within 24 hours, the area around the wound begins to swell, hurt, a fever appears, and the temperature rises.
Traditional medicine methods can only be used with the permission of the attending physician, with an accurately established diagnosis. As a rule, various decoctions based on medicinal herbs are used in the form of compresses during the rehabilitation period and only as an additional means for faster healing.
4.Treatment
It should be understood that outpatient treatment of phlegmon is impossible; this condition is too dangerous. There is no talk of self-medication, folk or any other non-medical “methods”; any delay poses a mortal risk. Hospitalization in a specialized hospital is required (a lesion in the oral cavity or facial structures requires hospitalization in the department of maxillofacial surgery). The intervention is performed under general anesthesia, with wide and deep access; its main purpose is drainage, i.e. ensuring free and most effective drainage of pus. Intensive antiseptic treatment is performed and powerful antibiotic therapy is prescribed; arbitrarily varying prescribed doses, canceling or adding medications at your own discretion is just as dangerous as self-medicating in the insane hope of “maybe.”
The patient should remain under observation and receive all necessary procedures (replacement of drains, lavage, irrigation, etc.) until the threat is considered minimal. Only under conditions of strict compliance with all medical prescriptions and strict adherence to aseptic oral hygiene measures can the prognosis be considered favorable: in most cases, complete recovery can be achieved.