Emphysema is a lung disease in which the lung tissue becomes “overinflated” due to the gradual destruction of the alveoli. There is a lot of air, but this air does not participate in gas exchange. In bullous emphysema, air bubbles form in the lungs. These bubbles are called bullae and are filled with air.
- Bulla is an air bubble with a diameter of at least 1 cm and having a thin wall (no more than 1 mm).
- Single or multiple bullae constitute bullous emphysema and bullous pulmonary disease.
- Bullous emphysema and bullous pulmonary disease are different.
- 12% of people over 30 years of age have various bullous changes in the lungs.
Bullae arise when the structure of the alveoli and the partitions between them is destroyed. Alveoli are tiny sacs made up of a thin membrane. The process of respiration occurs in the alveoli - oxygen enters the blood, and carbon dioxide from the blood enters the exhaled air.
The process of forming bullae is similar to blowing soap bubbles, when small bubbles combine into large ones, and then even larger ones. The cause of destruction of the alveoli and interalveolar septa is COPD or congenital lung pathology.
Bullous emphysema is more common in patients with COPD against the background of panacinar and centrilobular emphysema of both lungs.
In bullous disease, there is lung tissue without emphysema, and there may be several or one bulla. In congenital syndromes such as Marfan and Ehlers–Danlos syndromes, primary bullous pulmonary disease is isolated
Diagnosis and treatment
The diagnosis is made by a therapist or pulmonologist. At the appointment, he will collect complaints, examine the patient, listen and tap the chest. For an accurate diagnosis, instrumental methods for examining the lungs (X-ray, CT, assessment of external respiratory function) will be prescribed.
In the treatment of pulmonary emphysema, lifestyle correction is of great importance: quitting smoking, changing jobs (if necessary), increasing immunity.
Oxygen therapy and breathing exercises have a positive effect on the lungs. It is extremely important to promptly and thoroughly treat the chronic lung disease that has led to emphysema. For this purpose, antibiotics and antiviral drugs in the acute stage, expectorants, etc. can be prescribed.
In some cases, the patient is indicated for surgery to remove bullae (swollen areas of lung tissue). The procedure is performed both using the classical method with opening the sternum, and using endoscopic equipment.
Classification
For convenience of description and classification, bullae can be single or multiple.
In case of multiple distribution, the following options are determined:
- several bullae within one (focal) lobe
- several bullae in several lobes (multifocal).
- bullae are observed in all lobes of the lungs and are called diffuse.
Bullae located near the pleura or scars in the lung tissue can reach large sizes. Such bullae occur in paraseptal emphysema; they are devoid of vessels and interalveolar septa. Another type of bulla is located superficially and may contain vessels and fragments of lung tissue. Such bullae lead to pneumothorax.
The third type of bullae is located deep in the lungs. These bullae are rich in blood vessels and contain a lot of lung tissue.
A special place is occupied by giant bullae - this is a super bulla that occupies more than 1/3 of the lung and compresses the surrounding lung tissue. Giant bullae are characteristic of the lungs of a person who smokes tobacco or marijuana.
Patients with bullous disease are younger than patients with bullous emphysema. This is mainly due to congenital deficiency of α1-antitrypsin, as well as congenital genetic diseases (Marfan syndrome, Ehlers–Danlos syndrome).
Prevention
Prevention of pulmonary emphysema involves minimizing factors influencing the development of the disease:
- to give up smoking;
- prevention and timely treatment of lung diseases;
- eliminating exposure to harmful substances on the lungs;
- general strengthening of the immune system.
It is extremely important to start treatment as early as possible, that is, even at the stage of development of the primary disease. Therefore, if you are sick, you should not postpone going to the doctor.
Medical experts warn that lung diseases should not be self-medicated. If you suspect that you or your loved ones have pulmonary emphysema, consult a doctor as soon as possible so that a specialist can make the correct diagnosis and prescribe adequate treatment.
Emphysema. New treatment methods.
Emphysema is a condition in which the air sacs in the lungs (alveoli) are partially destroyed, leading to a decrease in the total surface area of the lung tissue and resulting in progressive shortness of breath.
Causes of emphysema:
- smoking tobacco and/or smoking marijuana
- air pollution, including tobacco smoke (so-called “passive smoking”)
- occupational hazards (inhalation of dust and harmful substances at work: miners, grinders, welders, etc.)
- insufficiency of alpha-1-antitrypsin (this substance “protects” the alveoli from destruction). In this case, emphysema usually occurs before the age of 40.
Emphysema most often occurs in smokers as part of chronic obstructive pulmonary disease (COPD).
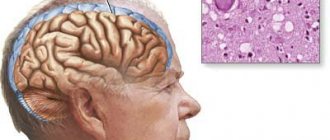
What happens with emphysema?
The lungs of a healthy person consist of air passages (trachea, bronchi and bronchioles) and air sacs (alveoli). The easiest way to imagine the structure of the lungs is in the form of a tree with large branches (trachea and bronchi), which continuously branch and turn into small branches (bronchioles). At the ends of the bronchioles there are hollow air sacs called alveoli (like bunches of grapes).
The alveoli have a very thin wall (0.5 micrometers) and are enveloped in a network of small vessels (capillaries). It is through the thin wall of the alveoli that oxygen enters the blood, and carbon dioxide enters the bronchioles and is removed from the body. The lungs can also be imagined as a very finely porous sponge. Thus, the total number of alveoli in both human lungs is 600-700 million. The diameter of one alveoli is 280 micrometers (for comparison, the thickness of a human hair is about 100 micrometers). The total surface area of the alveoli varies from 40 m² when exhaling to 120 m² when inhaling. This is a huge area! It is this feature that helps the lungs quite easily “extract” oxygen from the air and deliver it to the blood.
As emphysema progresses, the fine-porous sponge turns into a large-porous sponge. The walls of neighboring alveoli are destroyed, the alveolar sacs become larger. Thus, the diameter of one alveoli increases, but ultimately the total number of alveoli decreases, thereby reducing the total surface area of the lung tissue.
The lungs can no longer effectively “extract” oxygen from the air, so shortness of breath appears and progresses. No existing medications can restore normal alveolar structure or increase the total surface area of the lungs, which is why shortness of breath due to emphysema is so difficult to treat. One of the effective ways to reduce shortness of breath is to increase the concentration of oxygen in the inhaled air from 21% to 90%, then it will be easier for the lungs to “extract” it from the air.
Symptoms of emphysema.
The main symptom of emphysema is shortness of breath. The biggest challenge to making an early diagnosis is that shortness of breath develops gradually, very slowly. Even when you already have emphysema, you will not yet feel shortness of breath and will not consult a doctor in a timely manner. At first, shortness of breath worries only during severe physical exertion, and as the disease progresses, it occurs with minimal effort (talking, washing, dressing, etc.) or even at rest. Many patients unconsciously limit their physical activity, adapting to shortness of breath until it completely disrupts their lifestyle. Unfortunately, only then does the incentive arise to go to the doctor.
Later other signs may appear:
- weight loss
- change in the shape of the chest (“barrel chest”)
- cyanosis (bluish discoloration of the skin and mucous membranes)
- swelling in the lower extremities (not everyone experiences it)
Since emphysema most often occurs as part of a specific disease, symptoms of the underlying disease are observed in parallel with the progression of shortness of breath. For example, with COPD it is a cough.
Complications of emphysema.
In the presence of emphysema, the following often occur:
- giant bullae. Bullae are areas of the lung that are filled with air but do not participate in gas exchange. Essentially, these are large but useless air sacs in the lungs
- pneumothorax (collapse of the lung, most often due to ruptured bullae)
- chronic cor pulmonale (thickening of the wall and expansion of the cavity of the right half of the heart).
Diagnosis of emphysema.
If you experience shortness of breath, be sure to consult a doctor. No experienced and competent doctor will attribute your shortness of breath to age-related features or excess body weight until he conducts a full examination.
Minimum examination plan:
- patient examination
- complete blood count (to rule out anemia as a cause of shortness of breath)
- spirometry (pulmonary function test)
- electrocardiography (ECG, to exclude shortness of breath associated with heart disease)
- X-ray of the chest organs.
In many cases, additional examination is required to confirm the diagnosis:
- body plethysmography (a very accurate test of lung function)
- echocardiography (to exclude or confirm a complication of emphysema such as chronic cor pulmonale, or to exclude other heart diseases that cause shortness of breath)
- computed tomography of the lungs. Computed tomography of the lungs is the most accurate method for diagnosing emphysema. Because This study allows you to very accurately assess the structure of the lung tissue, measure its density and identify complications of emphysema (bullas).
- pulse oximetry (to determine blood oxygen saturation; with emphysema it may decrease)
- blood gas test (to detect hypoxemia - low oxygen content in the blood).
Treatment of emphysema.
Treatment of emphysema consists of two components - conservative and surgical.
Conservative treatment:
- Quitting smoking will help stop lung damage. This is the most effective method of treatment. If you are regularly treated with medications, but continue to smoke, the effect of treatment will be so insignificant that you will not even feel it. In the presence of occupational hazards, rational employment is very important to avoid contact with harmful vapors, gases, and dust.
- Treatment of the underlying disease. Emphysema is an essential component of COPD. Treatment of COPD is discussed in a separate article. In case of alpha-1-antitrypsin deficiency, injections of a drug containing this substance are prescribed (not registered in Russia).
- Long-term oxygen therapy. Many people with severe emphysema experience hypoxemia (low oxygen in the blood) due to ineffective lung function. The only way to eliminate it is long-term oxygen therapy using an oxygen concentrator. Treatment should be carried out indefinitely, daily for at least 15-18 hours a day. Long-term oxygen therapy for emphysema as part of COPD can reduce shortness of breath, increase physical activity, improve sleep, and most importantly, prolong life by 5-10 years or wait for a lung transplant.
Surgery:
- Lung volume reduction surgery. Most often it is performed when emphysema is predominantly localized in the upper lobes of the lungs. The essence of the operation is to remove altered areas of the lungs (parts of the upper lobes of the lungs), which allows relatively unchanged lung tissue to function normally. The operation reduces shortness of breath, but does not affect the prognosis and life expectancy of the patient.
- Bullectomy (removal of a giant bulla). After removing a bulla (or several bullae), space in the chest is “freed” for relatively unchanged areas of the lung, which allows them to function more efficiently.
- Lung transplantation.
A radical method of treating severe pulmonary emphysema, which has become available in Russia. Surgical treatment is performed only if conservative treatment is ineffective.
Call us right now and get quality advice regarding the choice of equipment!
Reasons for the development of the disease
The reasons for the development are loss of tissue elasticity and strength, increased pulmonary pressure. Impaired tissue elasticity and strength may occur as a result of the following:
- Congenital abnormal structure of lung tissue.
- Hormonal imbalance is a failure between the levels of estrogen and androgens.
- Atmospheric pollution - inhalation of smoke, small coal particles, toxins. Nitrogen and sulfur oxides, emissions from thermal power plants, and products of decay and fuel processing are dangerous. All this leads to respiratory failure.
- Congenital alpha-1 antitrypsin deficiency - proteolytic enzymes cease to perform their functions and begin to destroy the alveolar walls.
- Age - as a result of poor circulation, susceptibility to toxins in the air increases.
- Infections - when pulmonary diseases occur, activation of lymphocytes and macrophages occurs. As a result, the protein shell of the alveolar walls dissolves.
Increased pulmonary pressure may develop in the following cases:
- professional activities, such as playing wind instruments;
- COPD, in which the patency of bronchioles deteriorates;
- entry of foreign objects into the bronchi is an acute form of pathology.
For what reason the bullous form develops, scientists do not know for sure. There are a number of theories that have not yet been proven - vascular, mechanical, infectious, genetic, enzymatic, obstructive.
Recommendations for air travel
Pneumothorax is a complication of bullous transformation of the lungs. Air travel poses a certain risk for these patients because at an altitude of 2.5 km, the cavities in the lungs containing air can increase by 38-40%. This expansion can lead to bulla rupture and pneumothorax.
To be fair, episodes of pneumothorax during air travel are rare and there are no categorical bans on flying patients with bullae in the lungs.
If pneumothorax occurs 7-14 days before the flight, air travel should be postponed.
Questions and answers
How is pulmonary emphysema treated?
Patients with emphysema are prescribed a conservative course of treatment, which allows them to cope with symptoms, ensure normal functioning of the respiratory tract and eliminate possible complications. The duration of treatment depends on the severity of the patient's condition and the symptomatic picture. It is possible to adjust the previously chosen tactics in the direction of adding or eliminating some of the medications taken.
Is there a cure for emphysema?
We can talk about the chances of curing the disease only on the basis of research results and timely seeking medical help. In the early stages, it is possible to almost completely eliminate the signs of pathology and return the patient to the ability to breathe fully. In advanced cases with numerous complications, it will not be possible to cope with the disease without consequences.
What is the main symptom of emphysema?
The disease is indicated by shortness of breath after physical exertion or without it (in the later stages), as well as a cough with a large volume of sputum with purulent or mucous contents. Other symptoms - wheezing and whistling, protrusion of the chest, puffiness and swelling of the face - may vary depending on the nature of the pathology.
About emphysema
Emphysema is a very common form of nonspecific lung disease.
With pulmonary emphysema, there is a pathological increase in the air spaces of the pulmonary bronchioles. In addition, the alveolar walls change without restoration. Emphysema, along with diseases such as chronic obstructive bronchitis and bronchial asthma, belongs to the group of chronic obstructive pulmonary diseases (COPD).
All such diseases are accompanied by a violation of bronchial obstruction, with which the clinical picture is similar. In recent years, the incidence of pulmonary emphysema has been continuously increasing, especially among the elderly.
Pathogenesis
The key point in pathogenesis is the destruction of lung tissue fibers, which is caused by an imbalance in the proteolysis-antiproteolysis systems. Some researchers believe that fibroblast dysfunction also plays a role. With alpha-antitrypsin deficiency, the activity of neutrophil elastase increases, which breaks down collagen and elastin, causing the destruction of respiratory tissue.
The destruction of the alveolar walls and supporting structures leads to the formation of greatly expanded air spaces. Researchers believe that the absence of a tissue frame in the lower respiratory tract leads to their narrowing due to dynamic collapse during exhalation at the level of small lung volumes. Also, the destruction of the alveolar-capillary membrane reduces the diffusion capacity of the lungs by reducing the respiratory surface area.
Medicines
Photo: forumdaily.com
Medications used include bronchodilators. These include β2-agonists and anticholinergic drugs. The principle of action of β2-agonists is to relax the smooth muscles of the bronchi due to the stimulating effect on β2-adrenergic receptors. Short-acting drugs, the effect of which does not exceed 6 hours, include salbutamol. This drug is used to relieve an attack of bronchial obstruction. In other cases, preference is given to drugs with long-acting effects (formoterol, salmeterol). Their use can reduce the severity of shortness of breath and improve the quality of life.
A representative of anticholinergic drugs is Atrovent. This drug has a good bronchodilator effect and, due to its weak systemic effect on the body, causes virtually no side effects. Only some people report a bitter metallic taste in their mouth.
In case of progression of the condition, when bronchodilators do not cope with the task, glucocorticosteroids are prescribed, which can be used in inhalation form, as well as in injections and tablets. Budesonide is a representative of inhaled glucocorticosteroids. Long-term use of the drug can cause some side effects. The most common symptoms are sore throat, dry or irritated mouth, and cough; candidiasis of the oral mucosa is much less common. Prednisolone is used in tablet and injection forms. This drug has more side effects, as it acts systemically on the body. Therefore, the prescription of glucocorticosteroids is considered in each individual case, and in no case is the starting therapy.
Methylxanthines (aminophylline, theophylline) have a dubious effect. Their purpose still causes numerous disputes between various specialists. It is believed that methylxanthines can only reduce the number of exacerbations of bronchial obstruction, but do not affect the improvement of lung function. Therefore, it is recommended to use these drugs exclusively in combination with bronchodilators, but not to prescribe them as monotherapy.
Risk group
The disease risk group is compiled taking into account the most common causes of its development. According to WHO, centrilobular emphysema occurs in 78% of cases in people over 50 years of age. More often, the pathology is observed in heavy smokers and people who have suffered from chronic diseases of the respiratory system for a long time. Paraseptal and centrilobular emphysema are common pathologies in people with chronic lung diseases.
People whose activities involve contact with chemicals often get sick. Builders and workers in hazardous industries are susceptible to the development of pathology.
Due to the abnormal development of connective and pulmonary tissue, patients suffering from autoimmune diseases and pathologies of the endocrine system are also at risk.
Our specialists
Chikina Svetlana Yurievna
Candidate of Medical Sciences, pulmonologist of the highest category. Official doctor, expert at Russian congresses on pulmonology.
30 years of experience
Kuleshov Andrey Vladimirovich
Chief physician, candidate of medical sciences, pulmonologist, somnologist, member of the European Respiratory Society (ERS).
Experience 26 years
Meshcheryakova Natalya Nikolaevna
Candidate of Medical Sciences, pulmonologist of the highest category, associate professor of the Department of Pulmonology named after. N.I. Pirogov.
Experience 26 years
Nikitina Natalia Vladimirovna
Deputy chief physician, pulmonologist, allergist of the highest category. Full member of the European Academy of Allergy and Immunology.
Experience 15 years
Symptoms of emphysema
Symptoms of pulmonary emphysema are expressed in a vivid way and, first of all, shortness of breath. A very severe form of shortness of breath can occur with primary emphysema; it is shortness of breath, in the absence of such a symptom as cough, that indicates the onset of the development of pulmonary emphysema .
A person suffering from primary pulmonary emphysema has an extremely large volume of ventilation at rest, and during physical activity (even minimal) the patient experiences heaviness. Such a patient will have to intensively “puff” (cover his mouth when exhaling and puff out his cheeks) to increase intrabronchial pressure and increase the volume of ventilation.
With secondary pulmonary emphysema, serious disturbances occur in the gas composition of the blood. In the same way, with two types of pulmonary emphysema, the respiratory excursion decreases, the chest takes on a barrel-shaped shape. The supraclavicular areas bulge, a percussion sound occurs, and the mobility of the diaphragm and its location decrease. The x-ray clearly shows increased transparency of the pulmonary fields.
Bullae in the lungs on CT
Bullae in the lungs on CT are visualized as distinct, relatively darker, bubble-like areas of lung tissue, resembling holes or large pores of a sponge. The denser the tissue, the lighter it appears on CT scans—so, for example, bones are white, but airy lung tissue is a relatively uniform graphite gray color.
Using a CT scan of the lungs, a radiologist can accurately determine the diameter of the bullae, their number, and find out whether there are signs of emphysema, bronchiectasis or other diffuse pulmonary diseases.