- In which bronchi do malignant tumors occur?
- Classification of bronchial cancer
- Stages of bronchial cancer
- Causes of bronchial cancer
- Symptoms of bronchial cancer
- Methods for diagnosing bronchial cancer
- Treatment of bronchial cancer
- Surgical treatment of bronchopulmonary cancer
- Radiation therapy
- Chemotherapy
- Targeted therapy and immunotherapy
- Survival prognosis
“Bronchi cancer” is a term that is rarely used by doctors. In medicine, the more common concept is “bronchopulmonary cancer,” which combines malignant tumors of the lungs and bronchi. This approach to terminology arose due to the fact that the lung tissue and the bronchial tree are closely related, both in an anatomical and functional sense.
Some figures and facts regarding bronchial cancer:
- The disease most often occurs in older people. In more than half of cases, bronchial cancer is diagnosed after the age of 50 years. Another 25% of cases occur in the age group of 40–50 years.
- The main cause of malignant tumors of the bronchi is smoking. Up to 80% of patients are smokers.
- Most often, the tumor occurs in the upper parts of the bronchial tree, since they are better ventilated, and carcinogens contained in the inhaled air are more likely to lead to malignant transformation of cells.
In which bronchi do malignant tumors occur?
The air that a person inhales passes through the nose, pharynx, larynx, and trachea. At the level of the upper edge of the fifth thoracic vertebra, the trachea ends and divides into two main bronchi . This location is called the tracheal bifurcation . The main bronchi are the first order bronchi , they are divided into lobar (second order) , then into segmental (third order), subsegmental (fourth order), lobular, and finally into terminal (end) bronchioles.
All these branches together make up the bronchial tree . The walls of large and small bronchi are structured in the same way: on the inside they are lined with mucous membrane , under it there is a framework - fibrocartilaginous membrane , on the outside - the adventitial membrane.
Malignant tumors that originate from the mucous membrane are called cancer. They can occur in any part of the lung, but are most often found in the hilum - where the main bronchus enters the lung. In two thirds of cases, cancer develops in the bronchi of the first, second and third order.
Life expectancy for small cell lung cancer
Five-year survival rate - the number of patients who remain alive 5 years after their tumor is diagnosed - depends on the stage:
- Stage 1 – 31%.
- Stage 2 – 19%.
- The survival prognosis for stage 3 small cell lung cancer is 8%.
- The survival prognosis for stage 4 small cell lung cancer is 2%.
Yes, survival rates for small cell lung cancer are lower than for many other malignant tumors. But this is not a reason to give up. New drugs and treatment methods are emerging. Even if cancer cannot be defeated, doctors will do everything to prolong the patient’s life as much as possible.
Classification of bronchial cancer
The histological (based on the appearance of tumor cells under a microscope) classification of bronchopulmonary cancer includes four main types of tumors:
- Small cell cancer occurs mainly in smokers, is highly aggressive, spreads quickly and is difficult to treat. It accounts for about 12% of all cases of bronchopulmonary cancer.
- Squamous cell carcinoma , together with the next two types, combines into a group of non-small cell tumors , which account for more than 80% of all cases of lung cancer. The risk of developing squamous cell carcinoma is strongly associated with smoking.
- Adenocarcinoma is most common among women and nonsmokers. Unlike squamous cell carcinomas, adenocarcinomas are usually smaller in size and tend to grow in the peripheral parts of the lung. A separate subgroup of bronchoalveolar adenocarcinomas is distinguished.
- Large cell carcinoma consists of large, undifferentiated cells.
Depending on how much the tumor tissue has lost its normal features, poorly differentiated and highly differentiated tumors are distinguished. The first ones are more aggressive.
When choosing treatment, the location of the tumor foci is of great importance. Depending on this indicator, bronchopulmonary cancer is divided into two types:
- Central - the tumor is located in the bronchi of the 1st–3rd order (main lobar, segmental).
- Peripheral - the tumor is located in the smaller bronchi.
Write to an oncologist
Chemotherapy for small cell lung cancer
Chemotherapy is one of the main methods of treating small cell lung tumors:
- At a limited stage, chemotherapy and radiation therapy are usually prescribed simultaneously. This therapy is called chemoradiotherapy .
- In the advanced stage, only chemotherapy is used; radiation therapy is rarely used.
Combinations of platinum drugs (oxaliplatin, carboplatin) with etoposide and irinotecan are usually prescribed. Chemotherapy is administered for 1–3 days, followed by a “respite” of 3–4 weeks. This period is called a cycle. The course of treatment consists of 4–6 cycles.
After a course of chemotherapy, small cell lung cancer can recur. If a relapse occurs more than 6 months after completion of treatment, you can re-prescribe the drugs that were used previously. If a relapse occurs in less than six months, this indicates that the tumor has developed resistance to previous drugs - resistance . We need to select others.
Stages of bronchial cancer
Bronchopulmonary cancer is divided into stages depending on how far the tumor has spread in the body. In this case, they are guided by the generally accepted TNM classification. The letters in it mean:
- T—size of the primary lesion, degree of invasion into adjacent tissues.
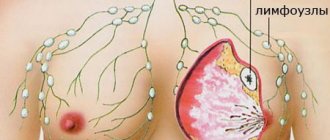
- N - damage to regional (close to the primary tumor) lymph nodes.
- M—presence of distant metastases.
Depending on these indicators, the stage of the tumor is determined, which is designated by Roman numerals I–IV.
Symptoms and signs
Signs of bronchial cancer at an early stage may be completely absent. A tumor can be diagnosed and seen accidentally during fluorography. Specialists from the Cancer Society in America suggest that people who have a long history of smoking regularly undergo computed tomography. With the help of periodic examinations, the presence of bronchial cancer can be determined in time. This kind of research is called screening.
The following symptoms of bronchial cancer are also noted:
- chronic persistent cough;
- presence of sputum with bloody discharge;
- there is shortness of breath while moving. This sign of bronchial cancer should alert a person;
- pain that occurs inside the chest.
A situation often occurs when there are symptoms of bronchial cancer, but it is not possible to recognize the disease. The clinical picture may resemble pleurisy, pneumonia, which proceeds sluggishly, etc. You should be careful about your own health. If there are signs of bronchial cancer that have been bothering a person for quite some time, you should immediately go to a specialist to be examined and treated.
Causes of bronchial cancer
A normal cell turns into a tumor cell when certain changes occur in its genes. It is impossible to say exactly why, in one case or another, genetic defects arose that led to malignant transformation. But there are known factors that significantly increase the risk of the disease. They are called risk factors .
The main risk factor for bronchopulmonary cancer is smoking. The likelihood that a person will be diagnosed with a malignant tumor directly depends on the length of smoking, the daily number of cigarettes smoked, the age at which the person started smoking, and the brand of cigarettes (tobacco quality, carcinogen content). Not only active but also passive smoking is dangerous. If someone constantly smokes in an apartment, the risk of lung cancer is increased for all its residents.
Other risk factors:
- Occupational hazards: workers in mines, factories producing cement, glass and fiberglass.
- Contact with chemicals, some volatile substances, asbestos.
- Air pollution with radon , a radioactive gas that is naturally released from the soil when uranium decays.
- It can accumulate indoors.
Etiology and risk factors
In 8 out of 10 cases, the cause of lung cancer is smoking, including passive smoking. But the disease is also found in non-smoking people. Risk factors include hereditary predisposition, regular exposure to volatile carcinogens, excessive chest radiation exposure, genetic disorders, certain viruses, alcohol abuse and malnutrition.
At risk:
- smokers over 40 years of age;
- alcoholics;
- patients with chronic obstructive pulmonary diseases;
- patients with oncological diseases of the upper respiratory tract and lungs in anamnesis;
- people with a family history;
- people who regularly come into contact with asbestos, radon, arsenic, dust;
- people with low social status.
Factors independent of a person include age over 50 years, endocrine disorders, and chronic lung diseases.
Symptoms of bronchial cancer
In the early stages, there are most often no symptoms. The tumor is diagnosed accidentally during an x-ray. Regular fluorography helps in early diagnosis. Experts from the American Cancer Society recommend that long-term smokers consider regular CT scans. Such periodic studies designed to diagnose cancer in early, asymptomatic stages are called screening .
Possible symptoms of bronchopulmonary cancer:
- Persistent chronic cough.
- Sputum mixed with blood.
- Dyspnea.
- Chest pain.
Even when symptoms appear, it is not always possible to recognize a malignant tumor immediately. The picture may resemble sluggish pneumonia, pleurisy, or another disease. It is important to be attentive to your health. If you experience any unusual symptoms, if they persist long enough, you should contact your doctor and get tested.
Book a consultation 24 hours a day
+7+7+78
Cancer cells produce various substances that enter the bloodstream and can cause pathological changes in the body. This leads to the so-called paraneoplastic syndrome . In lung and bronchial cancer, the tumor often affects the nervous system. This manifests itself in the form of disturbances in gait, balance, coordination of movements, swallowing, speech, memory, vision, sleep, etc.
Classification
The types of lung tumors are classified according to the location of the primary focus.
Central cancer is localized in the proximal (central) parts of the bronchial tree. The first signs of lung cancer (symptoms), which should alert you, in this case are clearly expressed:
- dry, prolonged cough that cannot be treated.
- hemoptysis begins with the addition of sputum.
- blockage of the bronchial lumen by tumor masses leads to shortness of breath even at rest. In some cases, the temperature may rise.
Photo 1 - Central cancer of the right lower lobe bronchus (1) with obstruction and metastases (2) to the bifurcation lymph nodes
Peripheral cancer gradually forms in the lateral parts of the lungs, slowly germinating and not detecting itself. This lung tumor may not produce symptoms for a long time; they appear with significant local spread, involvement of neighboring organs and structures, and invasion of the bronchi. Diagnosis of lung cancer of this type of localization is most often possible during a preventive examination (x-ray or computed tomography).
Photo 2 - Peripheral cancer (1) of the upper lobe of the right lung
Methods for diagnosing bronchial cancer
Usually the tumor is detected using x-rays. CT and MRI help to clarify its size, location, number of foci and their degree of invasion into surrounding tissues. Bronchoscopy is used - an endoscopic examination, during which a special instrument in the form of a long flexible hose - a bronchoscope - is inserted into the bronchial tree and the mucous membrane is examined.
During bronchoscopy, a biopsy can be performed: a fragment of a pathologically changed area of the mucous membrane can be obtained and sent to the laboratory for cytological and histological examination.
A biopsy can be performed in other ways: using a needle inserted into the lung through the chest wall, during thoracoscopy, or thoracentesis. You can also do a cytological examination of the sputum to look for cancer cells.
PET scanning helps detect small metastases. During this study, sugar with a special radioactive label is introduced into the body. The radiopharmaceutical accumulates in tumor cells and makes the lesions visible in pictures taken using a special device.
If necessary, the doctor may prescribe other diagnostic methods.
Surgical treatment of bronchopulmonary cancer
Surgical tumor removal is often the main treatment for local bronchial and lung cancer when there are no isolated metastases. The goal of radical surgery is to completely remove the tumor tissue. Depending on the size and location of the lesions, different types of surgical interventions are used:
- Removal of the entire lung - pneumonectomy .
- Removal of a lobe of the lung - lobectomy .
- Removal of a segment of the lung - segmental resection .
- Removal of the tumor with some surrounding healthy tissue - wedge resection .
- Removal of affected lymph nodes - dissection, lymphadenectomy .
The operation can be performed openly (through an incision) or endoscopically ( video-assisted thoracoscopic surgery , or VATS ).
Prognosis for a cure for cancer
The prognosis will depend on the neoplasm, its histological features, and the stage of bronchial and lung cancer. If radical surgery is performed at an early stage of the disease, it can give a positive result. This happens in most cases (80%). If a patient has an initial stage of bronchial squamous cell carcinoma, then in half of the situations the patients survive. When the disease is detected at the second stage, the survival rate is 25%. The survival rate in cases that are advanced or inoperable is 10%. If a person has been diagnosed with small cell cancer and the patient has undergone chemotherapy and radiation, then life expectancy is 15-55%. As for the last stage of bronchial cancer, the prognosis is not particularly favorable.
Radiation therapy
Radiation therapy for bronchial and lung cancer can be combined with surgery. Before surgery, the doctor may prescribe neoadjuvant radiation therapy (including in combination with chemotherapy), this helps to shrink the tumor and make it operable. After surgery, adjuvant chemotherapy is used to kill any remaining cancer cells and reduce the risk of recurrence.
If the tumor is inoperable, radiation therapy becomes the main treatment. For metastatic cancer, it helps fight pain and other symptoms.
How to make an appointment with an oncologist
If you suspect a serious illness, you should visit an oncologist. The oncology department uses modern treatment methods and the latest equipment, and employs experienced specialists. Therefore, effective treatment is guaranteed if you apply in a timely manner.
If you suspect oncology of the bronchi or lungs, you should visit an oncologist. He will study the clinical picture, symptoms of the disease, take into account important points, examine the patient and only then prescribe the correct treatment.
To make an appointment with a specialist, you can come to the clinic, which is located in the center of Moscow. If you are unable to come in person, you can sign up using a special form on the website or dial the phone number.
Chemotherapy
Chemotherapy drugs are drugs that destroy actively reproducing cells. Thus, their target in the body is primarily tumor cells, but healthy cells can also be affected, which is why chemotherapy is often accompanied by side effects. Modern doctors know how to reduce their risk and how to deal with them.
Like radiation therapy, chemotherapy for bronchial and lung cancer can be adjuvant, neoadjuvant, or can act as the main method of treatment. Different chemotherapy drugs with different mechanisms of action are used. Typically, your doctor will prescribe a combination of two or more drugs. Combinations are selected depending on the type and stage of the tumor.
Treatment
When choosing the treatment for this disease, the specialist takes into account certain points - the patient’s health, age, concomitant diseases, the presence of distant metastases, regional lymph nodes, what type of tumor, where it is located, at what stage the disease is, signs of bronchial cancer.
Surgery
Usually this type of treatment is the main one if there are no metastases (distant). Radical surgery is performed to completely remove the tumor. There are also several types of surgical treatment for bronchial cancer, it all depends on the lesions, their location, and size:
- pneumonectomy (the entire lung is removed);
- lobectomy (remove a certain part of the lung);
- segmental resection (a segment is removed);
- wedge resection (remove the tumor and some healthy tissue that surrounds it);
- lymph node dissection (lymph nodes that have been affected are removed).
Similar treatment of bronchial oncology is performed using the VATS technique or openly (initially an incision is created).
Radiation therapy
It can be performed in addition to surgery. Neoadjuvant therapy is sometimes prescribed before surgery begins. This makes it possible to make tumors in bronchial and lung cancer smaller and ensure its operability. After surgery, adjuvant chemotherapy is used to destroy any remaining cancer cells and reduce the chance of recurrence.
In case of inoperable tumor, treatment is carried out using radiation therapy. If bronchial cancer is metastatic, then this type of treatment helps relieve the patient of pain and other symptoms.
Chemotherapy
After studying the signs of bronchial cancer, the doctor prescribes medications that can destroy actively reproducing cells. First of all, chemotherapy drugs target cancer cells, but healthy ones are also affected. Therefore, in many cases, chemotherapy entails side effects. Doctors know well how to deal with side effects and reduce the risk of their occurrence.
Chemotherapy is also divided into neoadjuvant and adjuvant. It can be an addition to the main treatment or act as a separate treatment. For this purpose, different medications are used, which differ in their mechanism of action. Typically, a complex of several drugs is prescribed for the treatment of bronchial cancer. The complex can be different, it all depends on the tumor, its type, and the stage of the disease.
Immunotherapy, targeted therapy
These areas are considered quite young and modern in the treatment of bronchial cancer.
Targeted drugs are able to attack the target molecule. It is used by cancer cells to survive, to multiply without any control, to activate blood vessels and their growth. Compared to conventional chemotherapy drugs, targeted drugs act more specifically and are therefore considered safe for human health. However, some side effects are noted here too.
If we talk about immunotherapy drugs, in most cases monoclonal antibodies are used. They act as checkpoint inhibitors. We are talking about molecules that allow cancer cells to suppress the immune system and its work.
Such methods of treating cancer of the central bronchus of the lung are used in the last stages of the disease, when metastases are present in the body. In the last stages of the disease, a complication called pleurisy often occurs.
Targeted therapy and immunotherapy
Targeted therapy and immunotherapy are modern, youngest trends in cancer treatment, the emergence of which became possible thanks to the rapid development of molecular genetics in recent decades:
- Targeted drugs affect a specific target molecule that cancer cells use for survival, uncontrolled reproduction, and activation of blood vessel growth. They act more targeted and selective compared to classical chemotherapy drugs, and due to this they are safer, but still have some side effects.
- The most commonly used immunotherapy drugs checkpoint —molecules that cancer cells use to suppress the immune system.
Typically these treatments are used in later stages when there are metastases. Also, in the later stages, doctors have to deal with such a complication of bronchial and lung cancer as pleurisy.
| To main |
(Radiation Diagnostic News 2001 1-2: 11-15)
Central lung cancer.
Dzyuban V. P.
Research Institute of Oncology and Medical Radiology named after. N.N.Alexandrova, Minsk.
Lung cancer firmly occupies first place in the structure of morbidity and mortality from malignant neoplasms in most developed countries of the world.
In the Republic of Belarus, the incidence rate is steadily increasing from year to year, in 1998. it amounted to 44 people per 100,000 population. It is predominantly the male population that is affected; lung cancer accounts for 23% of the cancer incidence. The ratio of sick men and women in different age groups is from 7:1 to 13:1. The incidence figures look much more ominous when we look at age-specific incidence. In the age group of men 70-75 years old, the incidence of lung cancer reaches 500 people per 100,000, and the overall incidence of men aged 50 to 75 years is 317 people per 100,000. This means that in the specified age interval, 8 out of 100 men, or every twelfth, will develop lung cancer. It should also be remembered that in rural areas the incidence is 1.3-1.4 times higher than in the city.
In the structure of cancer mortality of the entire population, lung cancer constantly and firmly holds first place. Due to the fact that only 37% of patients are diagnosed in stages I and II of the disease, the one-year mortality rate from lung cancer remains very high, exceeding 60%. These figures emphasize the special social and medical significance of the problem of lung cancer.
An internationally recognized synonym for lung cancer is the term “bronchogenic cancer,” which indicates the source of the tumor – the bronchial epithelium, regardless of the caliber of the bronchus.
Currently, we call central cancer a tumor that affects the proximal, i.e. central sections of the bronchial tree, including subsegmental branches. The priority research method for central cancer is bronchoscopy: it allows you to directly visualize the tumor, determine the proximal limit of its spread and, most importantly, obtain material for morphological verification of the diagnosis. In connection with the development of bronchoscopic technology in recent decades, not only segmental bronchi, but also their subsegmental branches, i.e., have become accessible to inspection. bronchi of the 4th order. Accordingly, the distal border of the central cancer has shifted: it is a tumor that affects the main, intermediate, lobar, segmental and subsegmental bronchi. A tumor, the source of which is an even smaller bronchus, in the presence of a pronounced peribronchial node, is considered as peripheral cancer.
Among the variety of histological forms of lung cancer, from the point of view of a radiologist, it is advisable to distinguish 3 types:
1) Squamous cell carcinoma
- the most typical histological form in our republic (about 70% of all lung cancer), affecting mainly men, is a tumor with moderate growth rates, the usual stages of metastasis to the lymph nodes, with a tendency for distant metastasis to target organs, typical of lung cancer. It is squamous cell carcinoma that we are talking about when we consider the “classical” traditional X-ray diagnosis of lung cancer.
2) Adenocarcinoma
– a tumor “similar” in appearance to squamous cell carcinoma, which often has clinical and biological features that allow it to be called an “unpredictable” or “insidious” tumor. These features are as follows: a) The primary tumor is prone to infiltrative, branched growth, and therefore quickly spreads to the proximal parts of the bronchial tree, trachea, and the opposite side. Growing along the pulmonary vessels, the tumor quickly reaches the pericardium and heart chambers. In the case of peripheral cancer, there is a tendency to rapid invasion into the pleura and dissemination throughout the pleura. b) Early onset lymph node metastasis is often combined with normal size or slight enlargement of the affected lymph nodes. There is a violation of the typical phasing of damage to groups of lymph nodes; sometimes there are “jumps” of metastases from one group of lymph nodes to another, bypassing the intermediate ones between them. c) Adenocarcinoma is characterized by the rapid development of distant metastases, especially dissemination in the lungs and pleura. In this case, typical types of metastases may occur; a subtle picture of lymphangitis often develops in the lungs, and the first symptom of pleural damage is often effusion in the pleural cavity.
Thus, it is in cases with lung adenocarcinoma that radiologists most often make mistakes in diagnosing the locoregional state of the tumor. When establishing this histological form, one should be especially careful and purposefully look for minimal signs of local spread, lymphogenous and distant metastasis of cancer.
3). Undifferentiated cancer.
The majority of this group is small cell cancer, one of the most malignant tumors of the human body. From the point of view of radiodiagnosis, this form of cancer manifests itself with rapidly progressing lymphogenous metastasis. Against the background of massive conglomerates of lymph nodes, it is difficult to detect a primary tumor; due to the rapid development of the lesion, narrowing of the bronchi and impaired ventilation often do not have time to develop, and therefore difficulties arise in the differential diagnosis of undifferentiated cancer and mediastinal lymphoma. This tumor is also prone to rapid distant hematogenous metastasis to the brain, liver, kidneys, bones, and adrenal glands.
The radiological diagnostic algorithm for establishing lung cancer, determining its regional spread, lymphogenous and distant metastasis includes the following methods: 1. Fluorography 2. Radiography in 2 projections, fluoroscopy, radiopaque examination of the esophagus 3. Digital methods of X-ray diagnostics, primarily DFR -tomography 4. CT scan of the chest, if necessary CT scan of the abdominal cavity and brain 5. Ultrasound of the abdominal organs 6. Additionally, angiography (aortography, venocavagraphy, angiopulmonography), bone radiography, osteoscintigraphy, pulmonary perfusion scintigraphy, echocardioscopy can be used. 7. Bronchoscopy with biopsy and morphological methods for verifying the diagnosis are mandatory.
X-ray diagnosis of central lung cancer is based on the detection of a combination of three X-ray syndromes: 1. Syndrome of nodular formation in the root of the lung. 2. Syndrome of bronchial lumen obstruction. 3. Syndrome of impaired ventilation in the area drained by the affected bronchus.
Along with the three “classical” syndromes, we always strive to identify the fourth – regional lymphadenopathy syndrome, which characterizes metastatic lesions of regional lymph nodes. This syndrome is of fundamental importance not only for determining regional metastasis, but also from the point of view of differential diagnosis. In cases where the first three syndromes do not manifest themselves convincingly, or two of them are not expressed at all, the diagnosis cannot be formulated definitely. But when these “insufficient” signs are combined with regional enlargement of the lymph nodes, the diagnosis becomes almost absolute, since their combination practically does not occur in other diseases.
Before considering each syndrome separately, it is advisable to recall the forms of growth of central lung cancer. We adhere to a classification partially borrowed from bronchologists, which is based on the relationship of the tumor with the bronchial wall, that is, with the cartilaginous framework of the bronchus.
A tumor growing outside the bronchus is called peribronchial, while a tumor growing inside is called endobronchial. In turn, each of these forms can manifest itself as nodular or infiltrative growth. In the case of endobronchial cancer, nodular growth within the lumen of the bronchus is called exophytic, and infiltration of the mucosa and submucosal layer is called endophytic. Nodular growth of a tumor outside the bronchus is called so, and peribronchial tumor infiltration is called the creeping form of growth. An extreme expression of infiltrative growth with endobronchial damage to the bronchial tree over a large area, often with transition to the trachea and the opposite side, is considered as a separate form. This type of tumor is called branched.
In principle, most often we encounter a mixed form of growth of central cancer, when both endo- and peribronchial components are represented to varying degrees. In these cases, the peribronchial component always predominates (due to the larger space for its development than the small endobronchial volume), which forms the first of the radiological syndromes under consideration - the shadow of a tumor in the root of the lung.
The basis for diagnosing a node is fundamentally comparing the latter with the opposite side - for this it is enough to have a plain chest x-ray or even a good quality fluorogram.
The second thing that confirms or refutes the idea of a node at the root is a comparison with previous radiographs or fluorograms. Sometimes just a quick glance at the “old” and “fresh” fluorograms is enough to confidently make a diagnosis of lung cancer. This is why oncologists insist so persistently on providing a fluorographic archive when referring patients with suspected lung cancer. Conventional tomography helps clarify the shape, size, outline and structure of the tumor. CT, in addition, indicates the relationship of the tumor with the pulmonary vessels and mediastinal structures.
Signs of a nodule in the root of the lung are loss of structure and an increase in the intensity of the shadow of the root, expansion of its borders outward. The tumor node usually has large or small-lumpy outlines; as a rule, it is possible to identify areas with a radiant contour, which is especially characteristic of cancer. The tumor is located locally around the affected bronchi, it is necessary to differentiate it from the enlarged lymph nodes located in the immediate vicinity, which have clear outlines and convex, wavy contours, and the tumor is more or less blurry, blurry boundaries. However, in most cases, a single conglomerate of the tumor and metastatically affected enlarged lymph nodes is formed in the root of the lung, in which only by the appearance of the external outlines one can judge where the primary tumor is localized and where its metastases are. It should be noted that the tumor node with central cancer does not receive such a clear x-ray image as with peripheral cancer. This is due to the large number of shadows of the pulmonary vessels in the root, which veil and hide the shadow of the tumor itself. At the same time, when determining the size of the tumor, one should remember the contribution of normal anatomical elements to shadow formation and subtract their size from the total size of the root shadow. It is especially important to observe this principle when analyzing CT images without vascular contrast. We emphasize that without sufficient knowledge of the anatomy of the lung root and pulmonary vessels, one should not attempt to assess the extent of lung cancer based on CT data, which is always indicated when radiologically detected contact of the tumor with the mediastinal shadow.
Increased attention is paid to analyzing the structure of the tumor shadow in order to identify areas of decay in it. Tumor disintegration in central cancer is a relatively rare phenomenon, but potentially very dangerous for the patient due to the likelihood of developing fatal profuse pulmonary hemorrhage. Such patients should be considered as a surgical emergency, evaluated as quickly as possible, and urgently referred to thoracic oncological surgeons. Decay cavities in a tumor node are of two types: a) located on the periphery of the large peribronchial node; b) located centrally, being, as it were, a continuation of the affected bronchus and drained by it. It is this type of decay that is potentially most threatening with regard to bleeding.
In conclusion, we note that almost exclusively central squamous cell carcinomas undergo decay. The analysis of the following syndrome in central cancer—the study of the bronchial lumen—should be approached especially carefully. Detection of narrowing and breakage of the bronchi puts lung cancer in first place in the differential series, since in other lung diseases such changes are the exception and not the rule. Radiography usually does not give an idea of the state of the bronchial tree; one can rather guess than confidently judge the patency of the bronchi. The use of supervoltage modes and modern special screen-film systems (for example, Insight Thoracic) improves visualization of the bronchi, but does not replace our traditional method of longitudinal tomography. Only in cases of complete atelectasis of the lung against its background is the affected main bronchus so clearly visible that additional methods to the plain radiograph are not required. CT also allows reliable visualization of the bronchi, but the axial plane is not optimal for studying them, and subsequent multiplanar reconstruction leads to a significant deterioration in resolution along the longitudinal axis. The solution is the introduction of multi-slice spiral scanning, a feature of which is the isotropy of images (i.e., equal quality in all planes), but there are no such devices in the republic today.
In addition to traditional tomography in frontal and lateral projections, radiologists now have a new digital tomography technique in their arsenal. It made it possible to perform tomograms with the patient in an upright position and to select arbitrary oblique tomography projections for optimal alignment of the slice with the required bronchial plane. At the Research Institute of OMR, this technique has become the main one for x-ray visualization of the bronchi.
The nature of changes in the lumen of the bronchi provides important information not only for establishing the diagnosis of central cancer, but also for determining the form of its growth.
Amputation of the bronchial tube may occur - a complete absence of lumen in the usual place. In this case, there is often a protrusion into the lumen of a larger bronchus from the mouth of the amputated fragment of the exophytic component of the tumor in the form of a semicircular, semi-oval additional shadow. Most often we have to deal with a bronchial stump of various shapes - that is, a partially preserved bronchial lumen is found that has no further continuation.
The following stump shapes can be distinguished: semicircular, rectangular, trapezoidal, irregular, meniscoid.
All the changes in the bronchial lumen described above indicate the presence of an exophytic component of the tumor, which is very typical for lung cancer. Only the meniscoid shape of the stump requires serious differential diagnosis - it is more typical for benign bronchial tumors and special forms of cancer (mucoepidermoid and adenocystic or cylindroma) than for central bronchogenic cancer. A picture similar to exophytic cancer can be created by foreign bodies of the bronchi with granulations developing around them. If the foreign body is not calcified and there is no history of possible aspiration, only bronchoscopy can make the correct diagnosis.
Peribronchial tumor growth is indicated by conical or circular narrowing of the bronchial lumen. It is important that the clarity and evenness of the walls of the bronchi is maintained; sometimes their contour seems emphasized. A conical bronchial stump indicates the presence of a peribronchial component of the tumor, while an endobronchial component is not excluded. The most difficult thing to diagnose is infiltrative tumor growth along the walls of the bronchi - it manifests itself as thickening of the walls, increasing the intensity of their shadow, which is difficult to interpret against the background of the complex pattern of the vessels of the root. Endophytic growth is accompanied not only by a circular or conical narrowing of the bronchial lumen, but also by its deformation and unevenness; the walls appear finely lumpy, and in some places their clarity is lost. With peribronchial creeping growth, as already noted, the clarity and evenness of the walls, the uniformity of narrowing of the lumen must be documented, otherwise the nature of the growth should be considered mixed.
Impaired ventilation is the most common and pronounced syndrome, its manifestations predominant over other signs of central cancer. Its symptoms have been studied in the most detail, widely covered in the literature, and the priority of a number of scientific developments on this topic belongs to the Soviet radiology school.
According to classical concepts, a violation of ventilation in the parenchyma drained by a bronchus obstructed by a tumor goes through 3 stages - hypoventilation, valvular emphysema and atelectasis.
Valve emphysema, which develops when the bronchus is incompletely obstructed by an exophytic tumor, the elasticity of the walls of which is partially preserved, has the least clinical and diagnostic significance. On inhalation, air enters the lung tissue, and on exhalation, when the bronchus collapses, it cannot escape out. According to our observations, this short-lived condition, quickly replaced by atelectasis, is detected mainly retrospectively.
The term “hypoventilation” is used less and less by radiologists; it is more suitable for assessing the functional state of the lungs (for example, with ventilation pulmonary scintigraphy). It was replaced by the internationally recognized equivalent “dyselectasis”. This term denotes changes in a subsegment or larger anatomical unit of the lung, including a triad of signs: 1) volumetric decrease 2) decrease in pneumatization 3) thickening of the vascular pattern
Dyselectasis is characterized, on the one hand, by easy detection on survey photographs and nonspecificity, on the other. This condition often accompanies severe somatic and surgical diseases in bedridden patients. When identifying signs of dystelectasis at the stage of primary diagnosis, especially in the risk population - men who smoke after 40 years of age, the radiologist is obliged to tomographically examine the bronchus draining the altered zone of the lung, and if there is no clear image of its lumen, recommend bronchoscopy to exclude central cancer.
Note that distelectasis is not accompanied by inflammatory changes in the parenchyma. If the latter develops, this condition is called obstructive pneumonia or obstructive pulmonitis. X-ray, in addition to signs of dystelectasis, reveals peribronchovascular infiltration in the form of blurred and widened vascular shadows, as well as uneven infiltration of the pulmonary parenchyma. Against the background of such darkening, small or large foci of clearing are often observed due to abscess formation. The type of obstructive pneumonia is even less specific than distelectasis, and requires serious differential diagnosis, primarily with a large group of nonspecific pneumonia. Recently, it has become increasingly common to observe a protracted course and slow resolution of segmental and polysegmental pneumonia, in the late stage of which fibrous changes form and a volumetric decrease in the inflamed area develops. This kind of pneumonia, especially those occurring cyclically, with relapses, requires mandatory x-ray visualization of the corresponding bronchus and bronchoscopy. It is this group of protracted, recurrent “pneumonias” that is the source of advanced forms of lung cancer. Neither the development of abscess formation nor good positive dynamics during antibacterial therapy should be taken as reliable diagnostic criteria for rejecting the diagnosis of lung cancer.
Atelectasis develops when the bronchus is completely obstructed by a tumor and is characterized by complete resorption of air from the lung tissue and a sharp decrease in its volume. In addition to these direct signs, as with dyselectasis, secondary symptoms, to one degree or another accompanying atelectasis, are of great diagnostic importance. This is, first of all, a displacement of the interlobar pleura and its concavity towards a volumetric decrease. Displacement of the root of the lung towards atelectasis, the mediastinum towards the affected side, elevation of the dome of the diaphragm and narrowing of the intercostal spaces on the affected side, vicarious emphysema of the adjacent areas of the lung are also revealed. These signs are also nonspecific and indicate volumetric reduction of the lung. Inflammatory and destructive changes also often develop in atelectasis. It is not always possible to diagnose them; only in some cases cavities with gas and liquid levels develop. A sign of severe, extensive purulent destruction in atelectasis is the normal size of the lobe or even its volumetric increase - such cases require emergency surgical care.
When forming atelectasis of segments and lobes, certain rules are followed, knowledge of which facilitates topical orientation and shortens the diagnostic search. Firstly, any atelectatic area is displaced medially and is necessarily associated with the root of the lung. Secondly, the shadow of atelectasis shifts to where the segment or lobe was normally located before. Thirdly, all lobes and segments bordering the interlobar pleura necessarily retain clear outlines in certain projections. The areas that are not in contact with the pleura have a blurred outline in any projection. In addition to the medial direction, the lobes fall as follows: on the right, the upper one is up and forward, the middle one is forward, the lower one is downward and backward; on the left, the upper one is forward, the lower one is down and backward. Let us recall the segments bordering the interlobar pleura: on the right in the upper lobe - S2 and S3, in the lower - S6, S7, S8, on the left in the upper - S1-2, S4 and S5, in the lower - S6 and S8. Both segments of the middle lobe are limited by the interlobar pleura. During the formation of atelectasis, the interlobar pleura often significantly changes its position and is revealed in projections perpendicular to those in which it is normally visible. For example, with atelectasis of the middle lobe, the horizontal interlobar pleura is visible only in the lateral projection; with atelectasis S6 on both sides (especially often on the left), the oblique interlobar pleura is clearly visible in the direct projection.
The combination of atelectatic lobes and segments indicates an affected bronchus, but this relationship is not always fully observed. With severe stenosis of the bronchial lumen, there may be no signs of impaired ventilation of the lung tissue. Conversely, with a clearly visible lumen, distelectasis of the parenchyma can form. This option is especially typical for cancer B1-2 on the left, which often has peribronchial creeping growth and is accompanied by the symptom of “bronchus elongation.”
Some types of atelectasis are “hidden” in nature and their identification requires attentiveness, experience and compliance with examination techniques. First of all, this is atelectasis of the lower lobe on the left, which is “hidden” retrocardially and appears in the direct projection only as an additional paracardial contour. Sometimes the atelectatic middle lobe is not visible in the direct projection, but it is impossible not to notice it on the lateral image.
There are cases when, against the background of atelectasis, distelectasis or obstructive pneumonia, the lumens of small bronchi are determined over a large area. Detection of such an air bronchogram can be the cause of a fatal diagnostic error. This symptom is considered pathognomonic for inflammatory processes in the lungs, and is especially popular in CT diagnostics. However, for inflammatory processes, the following rule is strictly observed - the air bronchogram must be traced throughout, from the main, lobar bronchi to the small branches. If there are areas of interruption of the bronchial lumen, then first of all you should think about central cancer.
Complete atelectasis of a lobe or lung often does not allow one to determine the true size of the tumor node in the root. Due to their similar density, even non-contrast CT will not help in such cases, and only bolus-enhanced CT can sometimes differentiate atelectasis from tumor. Against the background of atelectasis, one should not try to look for the outlines of a tumor or lymph nodes, since the true contours in the lungs are formed not at the border of two tissues - air and airless (that is, soft tissue density).
When looking for enlarged intrathoracic lymph nodes, it is important to compare previous and subsequent X-ray and fluorograms. If you suspect the presence of lymphadenopathy in the roots or mediastinum, it is necessary to resort to median tomography in a direct projection. Its information content in relation to the lymph nodes of the roots of the lungs is especially great: the most important diagnostic criteria in this case are the expansion of the borders of the roots, their compaction, lack of structure and convexity of the outer borders; expansion, rounding of the spurs of large bronchi. These features are often more convincing than non-vascular CT findings. Let us recall the features of the anatomy of the right and left roots: on the right, the vessels are located outside and in front of the bronchi, on the left - outside and behind. The lymph nodes are also localized according to the course of the vessels, so in the lateral projection they should be looked for on the right - in front, and on the left - behind the main bronchi.
The Naruke map of intrathoracic lymph nodes used by surgeons includes 14 groups, but for a practical radiologist in a general medical network it is enough to remember 5 groups of mediastinal lymph nodes - the upper and lower paratracheal (or tracheobronchial) on the right, the aortic windows on the left, bifurcation and prevascular (on both sides), which usually manifest as darkening of the retrosternal space. An increase in the latter is relatively rare in metastatic lesions and requires differential diagnosis with malignant lymphomas.
When looking for enlarged lymph nodes, you need to have an idea of the stages of metastasis of lung cancer in various locations, despite frequent deviations from the given rules.
Cancer of the upper lobe on the right: root lymph nodes (upper pole) - right lower paratracheal - right upper paratracheal.
Cancer of the lower lobe on the right: root lymph nodes (middle, caudal part) - bifurcation - right lower paratracheal - right upper paratracheal.
In case of cancer of the middle lobe, the second stage after the root of the lung can be both bifurcation and lower paratracheal lymph nodes.
Cancer of the upper lobe on the left: lymph nodes of the root on the left (upper pole) - lymph nodes of the aortic window - right lower paratracheal - right upper paratracheal.
Cancer of the lower lobe on the left: lymph nodes of the entire left root - bifurcation - right lower paratracheal - right upper paratracheal.
Thus, there is a tendency for left-sided cancer to metastasize to the right side of the mediastinum and a general tendency for cancer of any localization to metastasize to the right paratracheal lymph nodes.
Like the lymph nodes in the roots of the lungs, metastatically affected mediastinal lymph nodes appear as homogeneous semicircular, semi-oval shadows of various sizes with clear, smooth wavy or coarsely tuberous contours, while the mediastinal shadow is expanded. CT is of leading importance in the diagnosis of metastatic lesions of the mediastinal lymph nodes, in which all groups of lymph nodes are visible according to the Naruke map; the size, fusion of individual lymph nodes into conglomerates, the condition of the surrounding tissue, and invasion of metastases into the structures of the mediastinum are determined. For the diagnosis of bifurcation metastases, contrast esophagography remains important, making it possible to identify a rigid depression of various shapes and depths in the subbronchial segment of the esophagus on an anterior-right, anterior or anterior-left (for left-sided cancer) radiograph.
With the development of the material and technical base of radiation diagnostics, one should expect a decrease in the role of traditional methods of X-ray examinations in lung cancer and their replacement with spiral computed tomography with bolus contrast enhancement, as has already happened in economically developed countries.