Gastric acidity is a characteristic of the concentration of hydrochloric acid in gastric juice. This acid is produced by special parietal cells from the glands of the stomach. The main functions of hydrochloric acid are the digestion of protein foods, antibacterial action, stimulation of the pancreas, activation of digestive enzymes. And most importantly, hydrochloric acid contributes to the normal processing of food and its further movement into the duodenum.
Low acidity, as well as high acidity, absolutely equally causes the body a feeling of discomfort in the stomach area and leads to serious chronic diseases of the gastrointestinal tract.
Liquids with respect to their acidity are considered: neutral at pH = 7, acidic at pH < 7, alkaline at pH > 7.
The maximum theoretically possible acidity in the stomach is 0.86 pH.
The minimum theoretically possible acidity in the stomach is 8.3 pH. Normal acidity in the lumen of the body of the stomach on an empty stomach is 1.5–2.0 pH.
In addition, at different times of the day and in different parts of the stomach, acidity levels vary.
1.General information
Every adult has heard about such a functional indicator of the digestive system as acidity. And not only adults: a school chemistry course includes information about the pH value, acid-base balance, as well as litmus paper and phenolphthalein as indicators of acidity.
The pH value of the gastric environment should normally be significantly shifted to the acidic side: if approximately seven is considered a neutral value, then the pH of gastric juice is 1.5-2.5. This is one of the evolutionary protective measures that, to some extent, prevents the introduction and reproduction of numerous infectious pathogens that enter the body in large quantities with food. In addition, a strongly acidic environment is provided as a normative condition for food processing in such a complex biochemical synthesizer as our digestive (digestive) system.
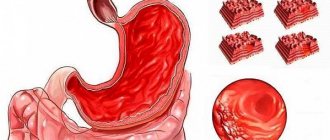
However, acid has an aggressive and destructive effect not only on pathogenic microorganisms and food products; it can also corrode its own mucous membrane lining the inner surface of the stomach. Therefore, it is necessary, firstly, precise control and constant “adjustment” of the acidity level, and secondly, physicochemical protection of one’s own tissues. The regulatory function is ensured by the fact that the stomach produces, along with hydrochloric acid, special mucus with an alkaline pH reaction, which, as necessary, neutralizes excess acid and acts as a surface protector for the gastric walls.
Any deviations from the natural pH level for the stomach, if they are persistent or chronic, are dangerous. So, low acidity, i.e. рh>5, leads to the development of antacid gastritis and is considered a precancerous condition. Increased acidity in recent decades has become a real scourge of modern man.
Excessive “acidification” of the gastric environment (acidosis, ph
A must read! Help with treatment and hospitalization!
Consequences
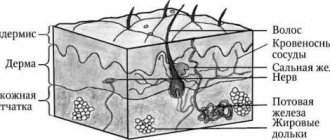
Due to the excess hydrochloric acid content in the stomach and the resulting indigestion, the patient may experience a sharp loss of body weight. A deficiency of nutrients, vitamins and minerals leads to brittle hair and nails, deterioration in the appearance of the skin - it becomes gray, dull, dehydrated, loses tone and becomes vulnerable to mites. Teeth are also subject to negative effects.
A more serious complication of increased gastric pH is the occurrence of gastritis and peptic ulcers. However, the development of these diseases most often requires the presence of additional negative factors (Helicobacter pylori infection, unhealthy lifestyle, unhealthy diet).
Opportunities for quickly eliminating symptoms and normalizing the level of stomach acidity allow us to make favorable prognoses for patients who are attentive to their health and follow the doctor’s recommendations.
2. Reasons
There are so many possible reasons for a persistent increase in acidity that they are usually divided into two large groups: endogenous and exogenous (internal and external, respectively).
The most common endogenous factors include:
- hereditary predisposition;
- chronic infections and/or presence of parasites;
- persistent hypoxia (lack of oxygen supply to tissues and organs);
- metabolic (metabolic) disorders;
- hypovitaminosis, deficiency of microelements, amino acids, etc.
Main exogenous factors:
- smoking and drinking alcohol, especially strong drinks;
- distortions in the daily diet (infatuation with spicy, fatty, spicy, over-salted, too hot and other dishes that irritate the mucous membranes of the gastrointestinal tract);
- long-term or amateur use of medications without prior consultation and supervision of a gastroenterologist;
- work in some hazardous industries, which involve, in particular, constant contact with nitrates;
- physical inactivity, sedentary lifestyle, haphazard eating with long breaks and a predominance of sandwiches, fast food, sour juices, coffee, carbonated drinks and similar “stomach killers.”
Visit our Gastroenterology page
Prevention of gastritis
To prevent gastritis, you should adhere to a healthy lifestyle: stop smoking, do not abuse alcohol, avoid stress and engage in any type of physical activity. It is especially important to monitor your diet. It must be complete and balanced. Try to include less junk food in your diet, do not skip meals, make sure that your body fully receives the necessary substances: proteins, fats, carbohydrates, minerals, micro- and macroelements, vitamins.
You can make an appointment with a gastroenterologist at the Naedine Clinic by phone in Kirov: (8332) 32-7777 or through the form on the website
3. Symptoms and diagnosis
A classic companion to high acidity is a specific baking, burning sensation in the esophagus, which we call heartburn. Heartburn can be so intense that the attack ends in vomiting. Most often, heartburn is caused by the so-called. reflux, i.e. reverse reflux of stomach contents up the esophagus, which should not happen under any circumstances with normal peristalsis, secretory activity and sphincter function: the walls of the esophagus do not have the same mucous-alkaline protection against acid that the stomach is equipped with.
In addition to heartburn, almost all patients complain of heaviness, abdominal pain of various types (dull, aching, pulling, “twisting”) and with various irradiations. Painful discomfort is usually associated with eating: when the stomach is full, the acid, so to speak, finds a new field of activity, but after 1-2 hours the pain returns.
It should be understood that a violation of the acid-base balance is a guarantee of complex, multifactorial digestive disorders (dyspepsia inevitably develops: constipation, diarrhea, nausea, vomiting, appetite disorders) and, therefore, metabolism. The walls of the stomach and the duodenum closest to it, from constant contact with an aggressive acidic environment, are covered first with superficial erosions, and then with ulcers that corrode the submucosal, deeper and therefore unprotected cell layers. A special “ulcerative type” of a patient suffering from gastroduodenitis or peptic ulcer disease itself is a thin, emaciated person with unhealthy skin and problem hair, a sallow complexion, dull and ever-tired eyes, a sarcastic, doomed mood (though many of them do not consider necessary to make at least some adjustments to your lifestyle). However, if the syndrome of high acidity and the associated erosive gastritis, duodenitis, colitis, peptic ulcer continue to remain, as they say in medicine, untreated, the situation can quickly become life-threatening: massive bleeding can begin at any moment or a perforation of the walls of the stomach or intestines can occur. , which leads to peritonitis, sepsis and other deadly complications.
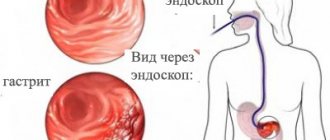
The diagnostic standard in modern gastroenterology is fibrogastroduodenoscopy (FGDS) - examination of the upper gastrointestinal tract from the inside. For this purpose, today we use not the ever-memorable “hoses” or “rubber tubes”, which served as a nightmare for many generations of patients, but high-tech, thin, flexible and very “smart” endoscopes, interfaced with a computer, equipped with a backlit video camera and the necessary manipulators (which allows “on the spot” to select material for biopsy, deliver the necessary treatment solutions, measure the pH level in various zones, etc.). The discomfort from such a procedure today is, perhaps, more of a psychological nature than physiological: the sensitivity of the pharynx and the gag reflex are suppressed by reliable irrigating anesthetics, and the procedure itself lasts only a few minutes - but the whole “picture” from the upper parts of the esophagus to the internal space of the duodenum is displayed in high resolution, stored on disk and provides invaluable information about the real state of affairs.
If necessary, radiography, tomographic and ultrasound examinations, and a set of laboratory tests are also prescribed.
About our clinic Chistye Prudy metro station Medintercom page!
Folk remedies
The patient can feel better with the help of infusions and decoctions based on medicinal herbs for high stomach acidity.
- A decoction based on mint, fennel herb and caraway seeds. It is necessary to take all the ingredients in equal proportions, pour boiling water over them and consume 100 ml 2 times a day before meals.
- Chamomile tea. It is enough to pour 150 ml of boiling water 1 tbsp. l. chamomile herbs purchased at a pharmacy. Leave for half an hour. Take before meals. This tea stabilizes digestion.
- A decoction of St. John's wort herb. Mix 50 g of herb with a glass of boiling water. Consume strictly before meals.
- Mint decoction. To prepare the product you will need a glass of mint and 500 ml of boiling water. Bring the resulting mixture to a boil over low heat and cook for 10 minutes, then leave the broth for half an hour. It should be taken at least 6 times a day, half a glass. The decoction has a calming effect on the gastric mucosa and enhances metabolism.
It is not recommended to use ginger, plantain and rosehip during treatment. They contain substances that irritate the gastric mucosa.
4.Treatment
To a certain extent (and only with the agreement of a gastroenterologist!) acidity can be controlled by yourself by drinking, for example, bicarbonate mineral waters. However, self-medication, in particular, “quenching acid with soda” still practiced by the population, is in itself dangerous, since a violent acid-base reaction with the formation of salt and water occurs in vivo in a somewhat more complex manner and differs from school chemical experiments in vitro.
The therapeutic regimen, of course, is selected on a strictly individual basis, taking into account diagnostic examination data and a number of other factors. The main directions, as a rule, are the prescription of antacids (acid-neutralizing) and coating agents, antihistamines, proton pump inhibitors (omeprazole, etc.); sometimes, strictly according to indications, anti-inflammatory, antispasmodic and/or antibiotic drugs are prescribed. You will need a special diet and the maximum possible elimination of all the factors of increased acidity described above (it is unnecessary to even discuss the need for immediate and complete abandonment of suicidal habits). At the first signs of a persistent increase in acidity, it is very important to contact a gastroenterologist for consultation, examination and treatment as quickly as possible, without waiting for the development of truly severe complications and without wasting time on all sorts of “proven old-fashioned methods”, which are sometimes more dangerous than the disease itself.
How to reduce stomach acidity?
Treatment for high acid levels involves the use of the following medications:
- Proton pump blockers. These include Omeprazole and Lansoprazole.
- Histamine blockers. Doctors often prescribe Ranitidine and Famotidine. They normalize digestion and reduce the amount of acid.
- Antiacid drugs. The most effective are Almagel and Maalox. They are prescribed for inflammation of the stomach and to normalize the level of hydrochloric acid secretion.
- To eliminate stomach pain, experts prescribe Motilium or Domidon.
A well-known remedy for neutralizing hydrochloric acid is baking soda. However, experts recommend not to abuse it during treatment.
Preventive measures
Since gastritis is now diagnosed not only in adults, but also in children, prevention should begin as early as possible. First of all, you should normalize your diet:
When the first symptoms of inflammation of the gastric mucosa appear, it is important to minimize (or better yet eliminate) the consumption of chocolate, coffee, spicy and fried foods.
Gastroenterologists recommend regularly checking for parasitic infestations. When they are detected, it is important to carry out timely treatment, because they often attack the digestive system.
Dangerous Kiss
– Why does chronic gastritis often worsen in the fall? After all, we eat approximately the same throughout the year.
- Not at all. In the summer, we often go on picnics, where we not only overeat on barbecue, but also indulge in alcohol. Add to this poorly washed food and food infections - and the stage is ready for an autumn aggravation. In addition, during the off-season the immune system often weakens, which can also lead to exacerbation. After all, microbes cannot be discounted as the cause of gastritis.
Fast food is not to blame, diets are of no use. The main myths about gastritis Read more
– If gastritis is often caused by microbes, does that mean you can become infected with it?
- Yes. The discoverer of Helicobacter pylori, Australian scientist Barry Marshall , conducted an experiment on himself by drinking a solution containing a culture of this bacterium and fell ill with gastritis. The bacterium can also be transmitted from person to person through dirty hands, shared utensils, or kissing.