Aplastic anemia is a serious disorder of the formation, development and maturation of blood cells. It is characterized by inhibition of the hematopoietic function of the bone marrow, which is manifested by a deficiency in the formation of white and red blood cells, as well as platelets. Sometimes there is a lack of formation of only red blood cells. The disease is considered one of the most severe disorders of hematopoiesis and, in the absence of adequate treatment, can cause death within several months. It affects male and female patients equally between the ages of ten and twenty-five or over fifty. According to medical statistics, two cases of pathology per one million people are diagnosed every year.
The Department of Hematology at CELT offers diagnosis and treatment of aplastic anemia in Moscow. Our multidisciplinary clinic was one of the first in the Russian Federation to begin operating in the market of paid medical services and has been successfully continuing it for the third decade. The hematology department receives consultations from leading domestic specialists, who have a modern diagnostic and treatment facility that allows them to accurately diagnose and carry out treatment in accordance with international standards. The cost of services is available in our price list, which we update regularly. To avoid misunderstandings, we ask you to check the numbers with our information line operators.
Aplastic anemia: etiology
According to origin, congenital and acquired anemia are distinguished. The first develops as a result of chromosomal mutations, the second - under the influence of chemicals, radiation, and infections. Experts believe that suppression of bone marrow hematopoiesis can be initiated by the appearance of cytotoxic T-lymphocytes in it and in the blood. They produce TNF (extracellular protein) and interferon “y”, which have a suppressive effect on hematopoietic germs. The reason for starting the mechanism may lie in:
- Exposure to ionizing radiation or chemicals in the form of aromatic compounds, arsenic, pesticides;
- Entering the body of infectious agents (causative agents of hepatitis “D”, “B”, cytomegalovirus, DNA-containing Epstein-Barr virus);
- Taking myelotoxic drugs while undergoing treatment with tranquilizers, anticonvulsants, antithyroid and antitumor drugs;
- Development of a number of autoimmune processes (systemic lupus erythematosus, connective tissue damage - Sjögren's syndrome).
In 50% of cases, the cause of the development of the pathology cannot be determined. This form of aplastic anemia is called idiopathic.
Prevention
Persons professionally associated with exposure to myelotoxic factors (sources of ionizing radiation, benzene production) should be under constant medical supervision. Carrying out cytostatic treatment for tumors and other diseases requires regular monitoring of blood composition and timely termination if there is a threat of hematopoietic hypoplasia. The use of potentially dangerous drugs, primarily chloramphenicol (see), should be limited to direct indications and be monitored by blood composition. Prevention of hemorrhages with already developed hemorrhage. includes hormonal suppression of the menstrual cycle in women with massive menorrhagia, replacement (if possible) of injection medications with oral ones, sparing the mucous membranes (excluding rough foods, replacing hard toothbrushes with cotton swabs). To prevent infectious complications in deep granulocytopenia (see Leukopenia), it is recommended to suppress intestinal autoflora with non-absorbable antibiotics; patients should be kept in aseptic or similar conditions, and personal hygiene should be monitored.
Classification of aplastic anemia
| Form of pathology | What is the difference? |
| By duration | |
| Acute | No more than one month |
| Subacute | From one month to six months |
| Chronic | More than six months |
| According to the severity of selective aplasia | |
| Moderate | Granulocytes less than 0.0x109/l, platelets less than 20.0x109/l. |
| Heavy | Granulocytes less than 0.5x109/l, platelets less than 20.0x109/l. According to diagnostic results, bone marrow cellularity is less than a third of normal. |
| Very heavy | Granulocytes more than 0.5x109/l, platelets more than 20.0x109/l. |
Aplastic anemia: symptoms
The disease begins acutely, it is accompanied by a feeling of severe weakness and fatigue. The patient's skin and visible mucous membranes look pale, and he himself suffers from the following clinical manifestations:
- noise in ears;
- the appearance of shortness of breath even with insignificant efforts;
- unpleasant tingling in the chest area.
When the number of platelets per unit volume of blood decreases, hemorrhagic syndrome appears:
- even after slight compression or shock to the skin, bruises and hemorrhages appear on it;
- a rash in the form of small dots can be seen on the body, arms and legs;
- bleeding gums are observed;
- spontaneous nosebleeds;
- heavy menstruation (in women).
A decrease in the number of leukocytes per unit volume of blood is characterized by the regular frequent development of infectious diseases of the skin and structures of the urinary system, inflammatory processes of the oral mucosa, and pneumonia.
The congenital form of anemia develops in children under ten years of age and is accompanied by a number of other disorders:
- underdevelopment of the skull and brain;
- reduction in the size and weight of the kidneys (hypoplasia);
- intense coloring of certain areas of the skin - hyperpigmentation;
- severe hearing loss and speech impairment due to it.
Pathological anatomy
At autopsy, signs of anemia and dystrophy of internal organs are found, abundant fat deposition in the subcutaneous tissue, epicardium, omentum, multiple hemorrhages in the skin, mucous membranes, serous tissues, and internal organs. Sometimes massive hemorrhages in the brain or heart muscle are noted, which are the direct cause of death. The bone marrow of flat bones is pale pink or yellowish in color, sometimes with dark red areas of hemorrhage. When the bone is compressed, a bloody fluid rich in fat drains from the cut surface. Areas of preserved hematopoietic tissue may be observed among the fatty bone marrow. The size of the spleen and lymph nodes is often reduced.
Rice. 1. Microscopic specimen of the liver (hypoplastic anemia): the arrow indicates the deposition of hemosiderin. Rice. 2. Microscopic specimen of a kidney (hypoplastic anemia): arrows indicate the deposition of hemosiderin in the tubular epithelium.
Microscopic examination of the bone marrow (see) reveals varying degrees of its devastation. In the case of aplasia, only small accumulations of lymphocytes, plasma cells and undifferentiated elements, single granulocytes and normoblasts are found in the fatty bone marrow. With hypoplasia, areas of hematopoietic tissue are found somewhat more often. Characteristic is the uneven distribution of foci of hematopoiesis not only in different parts of the skeleton, but also within the same bone. The structure of the bone tissue is often preserved. Both the early and late phases of the disease are characterized by the deposition of hemosiderin in the spleen, liver (Fig. 1) and bone marrow, less often in the kidneys (Fig. 2), lymph nodes.
Frequent complications of hypoplastic anemia include fibrinous-hemorrhagic pneumonia and necrotic changes in the mucous membranes and serous tissues, skin, and internal organs.
Aplastic anemia: diagnosis
Before starting treatment of the disease, CELT hematologists carry out a comprehensive diagnosis aimed at accurately making a diagnosis and identifying the etiological factor. It includes:
- examination by a hematologist;
- general and biochemical blood tests;
- collection of a bone marrow sample and its examination - sternal puncture.
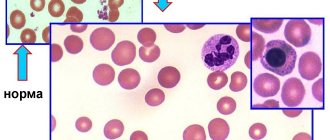
If the disease is present, the patient is diagnosed with a serious decrease in hemoglobin, up to a critical level of 20-30 g/l, and agranulocytosis is observed - a decrease in granular leukocytes and monocytes. The number of lymphocytes may be normal or reduced, platelets are always reduced, sometimes they are not detected at all. Erythrocyte sedimentation rate – increases to 4-60 mm/h. A study of a bone marrow sample reveals an increased content of adipose tissue - 90%, which includes elements of stroma and lymph, but hematogenous cells are present in very small quantities.
Story
In 1888, P. Ehrlich described a disease in a young woman, in which bleeding, fever, profound anemia and leukopenia developed acutely (platelets were not counted at that time); At the autopsy there were no signs of hematopoiesis in the bone marrow, which P. Ehrlich explained by the primary inhibition of its function. The term “aplastic anemia” was first proposed by Shoffard (A. M. Chauffard, 1904). Subsequently, aplastic anemia of the Ehrlich type was identified, in which, along with steadily progressing pancytopenia, often complicated by sepsis, pronounced hemorrhages and necrotic phenomena, histologically no signs of hematopoiesis were detected in the bone marrow; the disease was observed in persons aged 18 to 20 years. A similar disease called “hemorrhagic aleukia” was described by Frank (E. Frank, 1915). With the introduction into practice in 1927 by M.I. Arinkin of puncture examination of the bone marrow, it became possible to distinguish true hypoplastic anemia from pancytopenia caused by leukemic or metastatic lesions of the bone marrow. In the domestic literature, the first descriptions of G. a. under the name “clinical-hematological syndrome” belong to G.P. Khosroev (1913). G. a. the works of XX Vlados (1937), E. A. Kost (1952), I. A. Kassirsky and G. A. Alekseev (1962), F. E. Fainstein (1965), G. S. Mukhamedzyanova are devoted to the work of XX Vlados (1937), E. A. Kost (1952), I. A. Kassirsky and G. A. Alekseev (1962), (1970) and others.
The statistics have not been studied in detail. According to statistical data from Moscow prosecturas, the frequency of G. a. was in 1928-1932. 0.009%, in 1945-1950 0.13%, in 1951 - 1956 0.25%. In the USA (according to the state of California, 1967), the incidence of G. a. was 2 cases per 1 million people, or 1: 400,000 - 1: 700,000. A pronounced dependence of the incidence on gender, age and ethnicity has not been established.
Treatment of aplastic anemia
Treatment of idiopathic and other types of aplastic anemia is a very complex task that requires a comprehensive individual approach. When developing tactics, CELT specialists take into account the diagnostic results and the patient’s indications. The patient is placed in an isolation room with aseptic conditions, which eliminates the risk of developing infections and their complications. Drug therapy consists of taking:
- Glucocorticoids – in identifying autoimmune mechanisms and the formation of antibodies against one’s own blood cells;
- Cytostatics – in the absence of effect from treatment with glucocorticoids for autoimmune anemia;
- Cyclosporine “A” – to suppress the production of TNF and interferon “y”;
- Anabolic steroids – to stimulate hematopoietic function;
- Androgens – to stimulate the formation of red blood cells.
All patients with aplastic anemia receive transfusions of red blood cells and/or platelets, in volumes determined based on the clinical picture and peripheral blood parameters. In addition, the patient may be prescribed a splenectomy, a surgical procedure aimed at removing the spleen. Bone marrow transplantation can provide the most favorable prognosis. It consists of transplanting donor or own hematopoietic stem cells, previously removed from the iliac bones by puncture. Unfortunately, the procedure is not widely available due to the difficulty of selecting a compatible donor. If this is not possible, the patient is prescribed palliative therapy with cyclosporine A.
The hematology department of our clinic welcomes candidates, doctors and professors of medical sciences with over twenty-five years of practical and scientific experience. You can make an appointment with them online or by contacting our operators. Highly qualified specialists also work in the urology department. You can make an appointment with them for cystoscopy of the bladder.
At CELT you can consult a hematologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
By making an appointment with a hematologist, you can get a comprehensive consultation. The doctor is competent to treat various blood diseases, most of which can be identified in the early stages and prescribe timely treatment to cope with the disease quickly and easily.
Publications in the media
Aplastic anemia is a group of pathological conditions characterized by pancytopenia in the peripheral blood due to inhibition of the hematopoietic function of the bone marrow.
Classification • Congenital (Fanconi, Diamond-Blackfan anemia) • Acquired (the result of exposure to chemical, medicinal, infectious agents and ionizing radiation) • Idiopathic (the cause of the disease is unclear).
Etiology • Acquired anemia •• Infections (viral hepatitis, infectious mononucleosis, CMV, parvovirus, influenza) •• Lymphoproliferative disorders (thymoma, lymphoma, chronic lymphoblastic leukemia) •• Ionizing radiation •• Toxins and chemicals (benzene, insecticides, lead compounds etc.) •• Drugs, for example cytostatics, gold preparations, NSAIDs, anticonvulsants, antibiotics • Congenital anemia (Fanconi anemia). There are 4 complementation groups, i.e. at least 4 genes, mutation of any of which leads to the development of aplastic pancytopenia of 4 types (all r) •• Group A (type 1 Fanconi anemia, *227650, 20q13.2–q13.3, defects in the genes FA1, FA, F, r ) •• Group B (type 2, *227660, FA2 gene defect, r) •• Group C (type 3, *227645, 9q22.3, FACC gene defect, r) •• Group D (type 4, *227646, FA4, r gene defect).
Pathogenesis of aplastic anemia • Intrinsic defect of hematopoietic stem cells • Immune reaction to hematopoietic tissue • Impairment of the supportive function of the stromal environment in the bone marrow
Clinical picture
• Characteristic features of aplastic anemia •• General signs (shortness of breath, pallor of the skin and mucous membranes, tachycardia, weakness, systolic murmur at the apex of the heart, loss of body weight) •• Frequent addition of infectious-inflammatory and purulent-necrotic processes of various localization due to leukopenia ( neutropenia) •• Hemorrhagic syndrome: large and small hemorrhages (including in the retina), bleeding of various locations (menorrhagia, melena, nosebleeds) caused by thrombocytopenia. Features in children • The predominant age is 14–16 years • Anemia is usually preceded by an infectious disease (chicken pox, rubella, viral hepatitis) • The disease develops very quickly • In 70% of cases, treatment with cyclosporine can achieve complete clinical and hematological remission.
• Fanconi anemia. There are 2 types •• Classic (type I) ••• Short stature ••• Microcephaly ••• Skeletal deformities (absence or hypoplasia of the first metacarpal or radius) ••• Kidney and heart abnormalities ••• Hypospadias ••• Skin hyperpigmentation ••• Deafness •• Type 2 is characterized by the presence of minor developmental anomalies.
• Congenital aplastic anemia (Diamond–Blackfan syndrome) is an allelic variant of Fanconi anemia (*205900, r). It is distinguished from Fanconi anemia by the early onset of anemia (usually in the first months of life), the absence of neutropenia and thrombocytopenia.
According to severity, they distinguish between non-severe (granulocytes less than 1.5´109/l, platelets 100´109/l, megakaryocytes less than 80´109/l) and severe (in peripheral blood granulocytes less than 0.5´109/l, platelets less than 20´ 109/l; in bone tissue, the predominance of fibrous tissue is more than 60%).
LABORATORY RESEARCH
• Acquired anemia •• Pancytopenia •• Normochromic erythrocytes •• Prolonged bleeding time •• Marked decrease in reticulocyte content (regenerative anemia) •• Increased iron concentration in the blood serum (due to blood transfusions) •• Normal indicators of total serum iron-binding capacity (TIBC) •• Serum erythropoietin concentrations are usually increased in proportion to the degree of anemia •• Impaired liver function tests.
• Fanconi anemia •• Macrocytosis (as opposed to acquired aplastic anemia) •• Increased HbF levels •• Absence of pronounced pancytopenia until 3–8 years of age •• Chromosome fragility, repair defects, increased sensitivity of chromosomes to diepoxybutane, mitomycin and ultraviolet radiation are characteristic.
• Diamond–Blackfan anemia: macrocytosis, reticulocytopenia, elevated HbF.
Bone marrow puncture • Increased iron stores • Reduced number of cells •• Decreased number of megakaryocytes •• Decreased number of myelocytes •• Decreased number of erythroid precursors •• Replacement of normal hematopoietic tissue with adipose and fibrous tissue • Fanconi anemia - bone marrow puncture often shows no changes.
Instrumental studies • CT of the thymus region if thymoma is suspected • X-ray examination of the bones of the forearm (possibly detecting abnormalities in the development of the radius) and thumbs (constitutional anemia) • Ultrasound of the kidneys.
Differential diagnosis • Transient erythroblastopenia in children • Myelodysplastic syndrome • Paroxysmal nocturnal hemoglobinuria • Acute leukemia • Hairy cell leukemia • SLE • Disseminated infection • Hypersplenism • Anemia in hypothyroidism, hypopituitarism and liver diseases.
TREATMENT
Management tactics • Inpatient treatment in the hematology department. In case of neutropenia, isolation is indicated to prevent possible infection • Exclusion of causative factors • Study of the HLA antigen system of patients and their family members.
Bone marrow transplantation in patients with severe aplastic anemia, especially under the age of 30 years, is the method of choice (if an HLA-identical donor is available) • Transplantation from unrelated donors in case of ineffective treatment.
Conservative treatment
• Carried out in the absence of a donor for bone marrow transplantation •• Antithymocyte globulin. To identify hypersensitivity, a skin test is first necessary ••• Drug of choice for the treatment of elderly patients or in the absence of a donor for bone marrow transplantation ••• Course dose of 160 mg/kg, divided into 4 doses, during the first 4 days of treatment •• • The required dose of the drug is dissolved in 500 ml of 0.9% sodium chloride solution and administered intravenously over 4–6 hours ••• The development of an anaphylactic reaction is an absolute contraindication to further administration of the drug •• Cyclosporine ••• Initial dose - 5 mg/kg/day orally or 3 mg/kg intravenously. Next, doses are selected based on the concentration of cyclosporine in the blood, determined daily ••• If there is no effect within 120 days, the drug is discontinued •• Methylprednisolone - 2 mg/kg/day IV from days 1 to 14 of treatment, 1 mg/day kg - from 15 to 21 days •• Granulocyte colony-stimulating factor (for example, molgramostim) - if thymoglobulin or cyclosporine is ineffective ••• Initial dose - 5 mcg/kg/day subcutaneously until the granulocyte count increases to more than 1,000/μl ••• If there is no effect within 14 days, the dose is doubled •• Androgens are effective in some types of Fanconi anemia, acquired aplastic anemia, although cases of successful treatment are extremely rare. If there is no effect within 4–6 months, the drug is discontinued gradually.
• Maintenance therapy •• Oxygen therapy •• Sanitation of the oral cavity and other mucous membranes •• Transfusion of washed red blood cells through leukocyte filters; platelet mass •• Antibacterial therapy •• Hemostatics
• Complications of therapy • Hemorrhagic syndrome • Infectious complications • Hemosiderosis during blood transfusion • Heart failure • Renal failure • Toxic hepatitis • Anaphylactic shock and serum sickness (when using antithymocyte globulin) • Development of acute leukemia.
Surgical treatment • Thymectomy for thymoma.
Treatment outcomes • Complete clinical and hematological remission: Hb concentration above 110 g/l, platelets more than 100´109/l, granulocytes more than 1.5´109/l • Partial clinical and hematological remission: Hb concentration 90–110 g/l, platelets 30–100´109/l, granulocytes 0.5–1.5´109/l • Minimum hematological response: Hb level 80–90 g/l, platelets more than 10–30´109/l (without transfusions).
Course and prognosis • Acquired anemia. The course and prognosis are directly proportional to the patient's age. In the absence of timely and adequate therapy, 80% of patients die within 3 months from the manifestation of the disease. With the introduction of cyclosporine into clinical practice, the chances of prolonging the patient's life have increased. In case of proposed bone marrow transplantation, in order to avoid sensitization in the preoperative period, it is advisable to avoid transfusions of blood products (especially from relatives) • Fanconi anemia. Survival does not exceed 4 years with isolated replacement therapy. The prognosis is much better with the effectiveness of androgens or bone marrow transplantation.
Synonyms: For Fanconi anemia - Fanconi syndrome.
ICD-10 • D60 Acquired pure red cell aplasia [erythroblastopenia] • D61 Other aplastic anemias
Notes • Bone marrow aplasia is a congenital or acquired severe condition manifested by pancytopenia. The congenital form is combined with phenotypic and cytogenetic abnormalities, which facilitates diagnosis • Pancytopenia - a decrease in the number of red blood cells, leukocytes and platelets. Characterized by pallor and drowsiness, infections caused by neutropenia; hemorrhagic diathesis due to thrombocytopenia. For differential diagnosis, a bone marrow examination is necessary (aplasia [usually hypoplasia] of the bone marrow, displacement of bone marrow sprouts by blast cells, autoimmune destruction of blood cells - Evans syndrome) • Congenital and sometimes idiopathic types of anemia are called constitutional.