Anemia
or
“anemia”
- a decrease in the concentration of hemoglobin in the blood below established standards, most often, with a simultaneous decrease in the total volume of red blood cells (red blood cells that carry oxygen). Anemia, as a secondary symptom, can accompany various diseases, causing the development of oxygen starvation of tissues. The patient experiences chronic fatigue and weakness, constant drowsiness and loss of strength, dizziness and shortness of breath.
Anemia in men and women
Anemia is one of the most common diseases among the adult population of the Earth today. Risk groups for developing anemia include:
- lovers of vegetarian cuisine.
- patients suffering from large blood losses due to the physiological characteristics of the body or a number of chronic diseases.
- pregnant women.
- professional athletes.
Anemia in men is diagnosed in the presence of malignant neoplasms or hidden bleeding of the gastrointestinal tract, peptic ulcer, hemorrhoids and other pathologies. A decrease in the level of hemoglobin in a woman’s blood can be associated with heavy menstruation, pregnancy and lactation, and a period of hormonal changes during menopause. Varying degrees of anemia also appear in children due to lack of adequate nutrition, impaired absorption of iron in the gastrointestinal tract, gastritis or parasitic diseases, limited exposure to fresh air and physical inactivity.
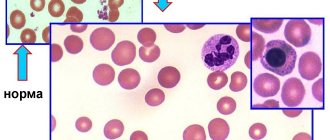
Norm and pathology
Here we should mention not only the normal levels of hemoglobin in the blood ( 120-130 g/l ), but also how red blood cells appear in our body in general. The main source of hematopoiesis, or hematopoiesis, is a certain precursor cell that can give rise to all the sprouts of red (erythrocytes) and white (leukocytes, platelets) blood. From this stem cell, erythrocyte precursors are formed, which, after several stages of differentiation, are transformed into reticulocytes (immature erythrocytes that retain the remains of the cell nucleus inside), and then into erythrocytes without cell nuclei.
Red blood cells are able to carry out their vital functions for 3-4 months, after which, when blood passes through the spleen, they are captured by its macrophages and digested. The spleen is also called the "graveyard of red blood cells."
When the number of red blood cells in the peripheral blood decreases, the causative, triggering factor can have an effect at any stage of differentiation of cellular elements . That is why it is important for the doctor to know what exactly could trigger the occurrence of anemia.
Principles of classification of anemia
There are several types of classifications of anemia, based on a number of signs - the cause of the disease, the mechanism of its development, stages, symptoms and other parameters. The following groups are distinguished:
Sign up for an anemia screening
Make an appointment
Classification of anemia by severity
The severity of anemia, determined by blood parameters depending on the age and gender of the patient, is conventionally divided into mild, moderate and severe. The mild form is characterized by a decrease in hemoglobin concentration to 90 g/l (the patient may experience general weakness and increased fatigue). The average degree is determined by the range from 70 to 90 g/l (patients complain of shortness of breath, tachycardia, headache, sleep disturbance, tinnitus, loss of appetite), and severe - below the limit of 70 g/l (the main danger of this condition is the development heart failure).
Myelodysplastic syndrome
Myelodysplastic syndromes (MDS) is a pathology of the Stobur cells of the cerebrospinal fluid, which leads to ineffective hematopoiesis and, as a result, to various combinations of anemia, neutropenia and thrombocytopenia. These syndromes are sometimes called pre-leukemic due to their nature and sometimes transform into acute leukemia. MDS in patients with less than 50 years of age rarely occurs, but in patients with more than 65 years of age, the frequency is 5%. To confirm the diagnosis, a bone marrow biopsy is required. This disease is characterized by the presence of chronic cytopenia, hyperplasia of the cerebrospinal fluid and morphological pathology of the progenitor cells in the cerebrospinal fluid.
The response to treatment with chemotherapy, immunosuppressants, growth factors (granulocyte-stimulating hormone and erythropoietin) is limited, and the survival rate of patients does not increase. Therefore, in older patients, treatment is alternated with blood transfusions and other symptomatic therapy.
Prepared by Bogdan Boris
Classification of anemia by color index
The color index determines the level of saturation of red blood cells with hemoglobin. It is calculated during a laboratory blood test using a special formula. Depending on the results obtained, there are:
Classification of anemia according to the mechanism of development of the pathological process
The following states are distinguished:
Iron-deficiency anemia
– the name indicates the cause of the pathology. Due to a deficiency of an important microelement, hemoglobin synthesis in the body is disrupted. The supply of oxygen to tissue cells, the stability of redox processes, and the functioning of the immune, nervous and cardiovascular systems depend on the level of iron. Clinical manifestations of iron deficiency anemia are dizziness, fainting, weakness and lethargy, shortness of breath with any exertion, palpitations. Pallor of the skin, brittle nails, thinning hair, and cracks in the corners of the lips are also typical for this disease.
Hemolytic anemia
occurs as a result of the accelerated destruction of erythrocytes (red blood cells) and the rapid accumulation of their breakdown products in the body. The main manifestations are an increased amount of indirect bilirubin in the blood. The patient experiences the development of anemic and icteric syndromes with an enlarged spleen and liver, as well as characteristic staining of feces and urine.
Posthemorrhagic anemia
– hematological changes that appear after acute or prolonged chronic blood loss as a result of external or internal bleeding (trauma, heavy menstruation, hemorrhagic diseases, gastrointestinal and pulmonary bleeding). The main manifestations of posthemorrhagic anemia are palpitations, shortness of breath, severe dizziness, darkening of the eyes, and lethargy. In severe cases - loss of consciousness.
Sideroblastic (sideroachrestic) anemia
occurs as a result of a violation of iron synthesis, causing its deficiency in red blood cells. Due to a failure in the processes of getting this microelement into the hemoglobin molecule, iron in the cells is replaced by sideroblasts (red blood cell precursor cells interspersed with iron in the form of a ring). This condition can be congenital or acquired. Experts believe that the main reason for the development of such anemia is a lack of the substance protoporphyrin. This organic component, combining with iron, turns into heme - part of the hemoglobin molecule. The main symptoms of the disease are disturbances in the functioning of the heart and blood vessels, indigestion, pale skin, dizziness, and memory loss. There is a danger of iron accumulation in various organs, which contributes to the occurrence of serious complications (liver cirrhosis, diabetes mellitus).
B12 deficiency anemia
– a disorder of hematopoiesis as a result of a lack of vitamin B12 in the human body. The main reasons for the development of such anemia are lack of adequate nutrition, impaired absorption of B12 due to inflammatory processes in the gastrointestinal tract, alcoholism, and hereditary predisposition. The pathology develops gradually, causing damage to the digestive organs and disturbances in the functioning of the nervous system.
Why does normochromic anemia develop?
This type of anemia is polyetiological, that is, there are many reasons that can lead to a decrease in the level of red blood cells and hemoglobin. The main reasons are as follows:
- Hemolysis. This is a condition accompanied by increased destruction of red blood cells due to mechanical, toxic, infectious or autoimmune effects on their cell membranes. In the peripheral blood, massive lysis of red blood cells occurs with a decrease in the amount of hemoglobin, as a result of which the transport function of the blood suffers. Such agents include viral and bacterial infections (influenza, whooping cough, typhoid, paratyphoid, measles, etc.), poisoning with toxins, poisons, heavy metals, as well as some systemic autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis, etc.).
- Aplastic syndrome. This is a severe clinical and hematological syndrome that occurs as a result of: damage to the body by salts of heavy metals, ionizing radiation, and drugs. It is characterized not only by normocytic anemia due to inhibition of red blood cell formation, but also by inhibition of all three lineages of hematopoiesis (leukocytes, platelets, red blood cells). This is called pancytopenia.
- Diseases of the urinary system. What is meant here is not so much inflammatory diseases of the lower urinary tract, but rather severe, chronic kidney diseases, especially with the development of chronic renal failure. The substance of the kidneys produces a factor that affects hematopoiesis, in particular, the formation of new red blood cells. This factor is called erythropoietin. In chronic diseases (chronic glomerulonephritis, diabetic nephropathy resulting in nephrosclerosis), a significant part of the kidney tissue is replaced by scar tissue, and therefore erythropoietin cannot be produced. Particularly severe anemia is observed in hemodialysis patients receiving renal replacement therapy through an artificial kidney device.
- Hemorrhagic syndrome. Normochromic normocytic anemia most often develops with blood loss. This can be any bleeding - both due to external mechanical damage and internal bleeding. Among the lesions of internal organs, gastrointestinal bleeding in stomach ulcers, Mallory-Weiss syndrome and cirrhosis of the liver, as well as uterine bleeding in women during menopause, are of particular importance. Often the development of anemia is facilitated by congenital and acquired disorders of the blood coagulation system (hemophilia, Werlhof's disease, etc.).
- Malignant neoplasms. The development of normochromic anemia can be affected by malignant tumors of the hematopoietic system (Hodgkin and non-Hodgkin lymphomas, leukemia), as well as tumors localized in any other organ. Gastric cancer especially often leads to the development of severe normochromic anemia. The pathogenesis of the development of anemia here comes down to the fact that the tumor releases toxins into the blood, which provoke inhibition of hematopoiesis and increased destruction of red blood cells in the peripheral blood.
- Inflammatory diseases. The concept of anemia of chronic inflammation is caused by the effect on the cell wall of red blood cells of pro-inflammatory proteins (cytokines) that circulate in the blood for a long time. That is why some of the red blood cells are gradually destroyed, and in addition, their life expectancy is significantly reduced. Also, pro-inflammatory proteins indirectly affect hemoglobin metabolism, which also leads to a decrease in its content in the body.
Cost of consultation for anemia?
| Name of service | Price, rub.) |
| Initial appointment with a cardiologist | 2000 rub. |
| Repeated appointment with a cardiologist | 1500 rub. |
| Primary appointment with a general practitioner | 2000 rub. |
| Repeated appointment with a general practitioner | 1500 rub. |
| Prescription of treatment (drawing up an individual treatment regimen) | 1500 - 3000 rub. |
All our services and prices
Diagnostic measures
To treat anemia, it is necessary to determine its type and cause of development. The main diagnostic method for this disease is laboratory blood tests (general and biochemical).
Changes that are observed in the general blood test:
small red blood cells (microcytosis).
Changes that are observed in the biochemical blood test:
In addition, a visual examination of the patient and a detailed history is required. Among the most common symptoms are pale skin and mucous membranes, cracks in the corners of the mouth, a “glossy” tongue, and an enlarged spleen.
To effectively correct the condition, instrumental examination methods may also be required:
computed tomography of the esophagus, stomach, duodenum. colonoscopy. Ultrasound of the liver, spleen, kidneys, genitals. X-rays of light.
Diagnosis of normochromic normocytic anemia
In addition to a clinical examination and history taking, the doctor must prescribe a general blood test. A mandatory diagnostic criterion is a decrease in hemoglobin (less than 130 g/l for males and less than 120 g/l for females) and a decrease in red blood cells (3.8 million/μl).
If necessary, for the purpose of differential diagnosis of normochromic anemia from other forms, determination of such biochemical and immunochemical parameters as:
- Serum iron (normal - Men: 12.5 - 32.2 µmol/l Women: 10.7 - 32.2 µmol/l), an indicator reflecting latent (hidden) iron deficiency with normal hemoglobin content in the blood, but with the presence of all clinical manifestations of anemia.
- The total iron-binding capacity of blood serum (the normal level of total iron binding capacity is 27.8 – 53.7 µmol/l). It increases with iron deficiency, decreases with normochromic and hyperchromic anemia.
- Transferrin is a protein circulating in the blood, the main function of which is the transport of iron from red blood cells to the cells of all internal organs (normal 2.0 - 3.6 g/l). In iron deficiency anemia, its content increases because the amount of “free”, unused protein increases, and in hemolytic anemia, its amount, on the contrary, decreases, because too much iron enters the peripheral blood, and all iron atoms are bound by transferrin, that is, free protein is very few.
- Ferritin is a protein whose main function is the deposition of iron atoms, normally found in the liver, spleen, muscles (normal - Men: 20 - 250 μg/l Women: 10 - 120 μg/l), with iron deficiency anemia its content in the blood decreases, and with normochromic anemia, on the contrary, increases.
In addition to blood tests, patients should undergo examination of other organs and systems:
- If diseases of the urinary system are suspected - ultrasound of the kidneys, general urine analysis, biochemical blood test with determination of urea and creatinine.
- If an oncological process is suspected, an examination plan is prescribed based on the localization of the presumptive diagnosis (from prostate-specific antigen or other tumor markers to computed tomography or magnetic resonance imaging of the corresponding organ).
- Rheumatic tests if an autoimmune process is suspected (determination of C-reactive protein, ESR, ASL-O, rheumatoid factor, etc.) followed by consultation with a rheumatologist.
- Bone marrow puncture for suspected aplastic or myelodysplastic syndromes.
- Search for the cause of bleeding in the hemorrhagic pathogenesis of normochromic anemia - fibrogastroscopy, studies of the reproductive system in women, colonoscopy, liver studies.
Treatment of anemia
The course of medical therapy is carried out on the basis of the diagnosis and includes the prescription of a special diet and medications, as well as, if necessary, surgical intervention to eliminate the causes of blood loss.
A balanced diet is of great importance for anemia. It compensates for the lack of iron and microelements involved in hematopoiesis. Nutritionists recommend eating foods rich in vitamin B12, folic acid and iron. The diet must contain meat, offal (liver, heart, tongue), fish, egg yolks, mushrooms, buckwheat, legumes, black currants, pomegranate, strawberries, nuts, apples, rose hip decoction, dried fruits. Vitamin C accelerates the absorption of iron by the body, while strong tea, coffee, and calcium hinder it. Strong alcoholic drinks are harmful to a patient with anemia.
Iron supplements are considered the most effective for combating anemia. They are better absorbed, increase hemoglobin levels faster, restore its reserves in the body, and eliminate weakness and fatigue. Based on blood test data for each patient, depending on a number of indicators (type of anemia, severity of the disease and the cause of its development, age of the patient), an individual daily dose, course duration, and preventive measures are calculated. In severe cases, intramuscular and intravenous administration of ampoule iron preparations in a hospital setting is possible to avoid adverse reactions and allergies.
It is advisable to take iron supplements one hour before meals or two hours after meals. Medicines should not be taken with tea or coffee. These drinks reduce iron absorption. You must use water or juice.
The prognosis for iron deficiency anemia is favorable in most cases. The patients' condition improves significantly, the body's resistance increases, sleep and appetite normalize. The basis for preventing anemia is a balanced diet. Do not get carried away with protein foods and sweets. There should be vegetables, herbs and fruits on the table all year round. Another rule is to maintain a healthy lifestyle, exercise, walks in the fresh air, proper rest and good sleep.
Sign up for an anemia screening
Make an appointment
Clinical manifestations of iron deficiency
The clinical manifestations of iron deficiency are diverse and can be reduced to two main syndromes: hypoxic and sideropenic. Hypoxic syndrome combines symptoms common to all anemia: pallor, increased heartbeat, tinnitus, headache, weakness. Sideropenic syndrome includes taste perversion, dry skin, changes in nails, hair loss, angular stomatitis, burning tongue, and dyspepsia. The variety of clinical symptoms of iron deficiency can be explained by a wide range of metabolic disorders, which are caused by dysfunction of iron-containing and iron-dependent enzymes [6, 8, 9, 26, 27].
Symptoms that are less associated with anemia, but may be a manifestation of iron deficiency, include neurotic reactions and neurasthenia, decreased performance, muscle weakness and general tolerance to physical activity, disorders of metabolic processes in the myocardium, peripheral circulation and microcirculation, low-grade fever [6] . Exotic symptoms of IDA include urgency to urinate/defecate, urinary incontinence due to weakening of the sphincter apparatus, and difficulty swallowing due to atrophic changes in the esophageal mucosa [5, 12]. According to modern data, restless legs syndrome (Willis-Ekbom disease) may be one of the most common clinical manifestations of iron deficiency [28, 29].
Anti-infective immunity disorders in patients with impaired micronutrient status and IDA are complex [30]. On the one hand, iron deficiency prevents the development of pathogenic microorganisms that require iron for their own growth and reproduction. On the other hand, iron deficiency indirectly leads to disruption of cellular resistance mechanisms and to infections (decreased microbicidal activity of granulocytes, impaired proliferation of lymphocytes). In general, the predisposition of patients with IDA to the development of infectious diseases is not as great as previously thought. Moreover, treatment of IDA with parenteral iron supplements increases the risk of developing infections, probably due to the availability of administered iron for the rapid growth of pathogenic microorganisms [7, 26].