Pernicious anemia (Addison-Biermer disease, B12 deficiency anemia)
A person's daily requirement for vitamin B12 is 1-5 mcg. It is satisfied due to the intake of the vitamin from food (meat, dairy products). In the stomach, under the action of enzymes, vitamin B12 is separated from food protein, but for absorption and absorption into the blood it must combine with a glycoprotein (Castle factor) or other binding factors. Absorption of cyanocobalamin into the bloodstream occurs in the middle and lower part of the ileum. Subsequent transport of vitamin B12 to tissues and hematopoietic cells is carried out by blood plasma proteins - transcobalamins 1, 2, 3.
The development of B12 deficiency anemia can be associated with two groups of factors: nutritional and endogenous. Nutritional reasons are due to insufficient intake of vitamin B12 from food. This can occur with fasting, vegetarianism, and diets excluding animal protein.
Endogenous causes mean a violation of the absorption of cyanocobalamin due to a deficiency of the internal Castle factor when it is sufficiently supplied from the outside. This mechanism for the development of pernicious anemia occurs in atrophic gastritis, a condition after gastrectomy, the formation of antibodies to the internal Castle factor or parietal cells of the stomach, and congenital absence of the factor.
Impaired absorption of cyanocobalamin in the intestine can occur with enteritis, chronic pancreatitis, celiac disease, Crohn's disease, diverticula of the small intestine, tumors of the jejunum (carcinoma, lymphoma). Increased consumption of cyanocobalamin may be associated with helminthiasis, in particular diphyllobothriasis. There are genetic forms of pernicious anemia.
Vitamin B12 absorption is impaired in patients who have undergone small intestinal resection with gastrointestinal anastomosis. Pernicious anemia can be associated with chronic alcoholism, the use of certain medications (colchicine, neomycin, oral contraceptives, etc.). Since the liver contains a sufficient reserve of cyanocobalamin (2.0-5.0 mg), pernicious anemia develops, as a rule, only 4-6 years after the supply or absorption of vitamin B12 is impaired.
In conditions of vitamin B12 deficiency, there is a deficiency of its coenzyme forms - methylcobalamin (participates in the normal course of erythropoiesis) and 5-deoxyadenosylcobalamin (participates in metabolic processes occurring in the central nervous system and peripheral nervous system). A lack of methylcobalamin disrupts the synthesis of essential amino acids and nucleic acids, which leads to a disorder in the formation and maturation of red blood cells (megaloblastic type of hematopoiesis). They take the form of megaloblasts and megalocytes, which do not perform an oxygen transport function and are quickly destroyed. In this regard, the number of red blood cells in the peripheral blood is significantly reduced, which leads to the development of anemic syndrome.
On the other hand, with a deficiency of the coenzyme 5-deoxyadenosylcobalamin, the metabolism of fatty acids is disrupted, resulting in the accumulation of toxic methylmalonic and propionic acids, which have a direct damaging effect on the neurons of the brain and spinal cord. In addition, myelin synthesis is disrupted, which is accompanied by degeneration of the myelin layer of nerve fibers - this causes damage to the nervous system in pernicious anemia.
Symptoms of anemia
Symptoms of B12 deficiency anemia
At the initial stage of development, symptoms may be erased or not bother you at all. As the syndrome develops, the following signs may appear:
- weight loss not associated with objective reasons;
- burning of the tongue and changes in taste sensations;
- increase in the size of the tongue, smoothing of the papillae, redness of the mucous membranes;
- alternating constipation and diarrhea;
- nausea;
- tingling in the arms and legs, numbness;
- gait disturbance;
- urinary disorders;
- decreased sex drive;
- decreased muscle tone;
- visual impairment;
- pallor, yellowness of the skin;
- graying of hair;
- cardiopalmus;
- dyspnea;
- vitiligo (spots on the skin), etc.
It is worth noting that disorders in the psychoemotional and cognitive spheres are not uncommon: deterioration of memory, attention and thinking, mood swings, tearfulness, irritability, depressive tendencies. An older person may develop dementia. The severity of neuropsychiatric symptoms does not depend on the severity of anemia, but is determined by how long it lasts and how quickly a person receives medical help.
Pathological anatomy
Deaths due to successful treatment of P. a. are extremely rare. Autopsies of those who died in the acute period of the disease reveal general anemia, yellowness of the skin, serous and mucous membranes, fatty degeneration of the myocardium, liver, and kidneys. The blood in the heart and large vessels is thin and watery. Due to pronounced hyperplasia of hematopoietic elements and the disappearance of fat, the bone marrow of flat bones, as well as the diaphyses and epiphyses of tubular bones, is very juicy, crimson-red in color. Atrophic changes in the gastrointestinal tract are characteristic. tract.
The papillae of the tongue, especially in the root area, are atrophic and smoothed. The mucous membrane of the tongue contains reddish areas of inflammation, most often located along the edges and at the tip, sometimes aphthous rashes, cracks (a picture of the so-called Gunter's glossitis). Similar changes can be observed in the mucous membrane of the gums, cheeks, soft palate, pharynx, and esophagus. Atrophy of the gastric mucosa is constantly detected, most pronounced in the fundus; the folds of the mucous membrane are smoothed or not defined, the wall of the stomach is thinned, in some cases there are polypous growths. Atrophic changes can also be observed in the intestinal mucosa. The size of the spleen is within or slightly larger than normal. The liver is slightly enlarged and rather dense. Due to the deposition of hemosiderin, the tissue of the spleen, liver, and sometimes kidneys on the section has a rusty tint. Lymph nodes are small and soft. In some cases, small foci of necrosis with softening are detected macroscopically in the spinal cord. Sometimes pinpoint hemorrhages are found in. serous and mucous membranes, in the skin.
Microscopic specimen of the gastric mucosa in pernicious anemia: 1 - atrophy of the glands, 2 - infiltration and sclerosis of the lamina propria of the mucous membrane; hematoxylin-eosin staining; X 70.
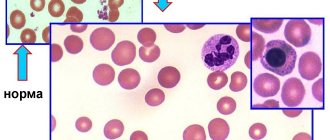
Microscopically, in the red bone marrow there is pronounced hyperplasia of the erythroid series of cells with the presence among them of a large number of megaloblasts - large cells with a delicate cellular structure of the nucleus with clearly visible nucleoli and a wide zone of basophilic or polychromatophilic cytoplasm. The number of leukocytopoiesis cells is slightly reduced. Megakaryocytes are present in sufficient or reduced numbers. There are pronounced dystrophic changes and breakdown of cells, especially of the erythroid series, and an abundance of erythro- and siderophages. In the gastric mucosa, a picture of atrophic gastritis is revealed; there is a significant decrease in the number of glands and glandular cells, especially parietal cells. The cells are reduced in size, pyknotic, flattened, as a result of which the lumen of the glands is expanded. The number of mucus-forming glandular cells increases, and areas of intestinal metaplasia of the surface epithelium are found. The stroma of the mucous membrane is sclerotic, infiltrated with lymphocytes, plasma cells, and single segmented neutrophilic granulocytes (Fig.). The changes are most pronounced in the fundus of the stomach, but their intensity can vary in different parts of the mucous membrane. Atrophic changes do not reverse during treatment with vitamin B12 and persist during the period of remission of the disease.
A biopsy of the mucous membrane of the small intestine reveals shortening of the intestinal villi, dystrophic changes in glandular cells with a decrease in mitotic figures in the crypts, and lymphoid-plasmacytic infiltration of the stroma. After treatment with vitamin B12, these changes may disappear. Along with atrophic changes, dystrophy of the nerve fibers of the tongue, nerve cells of the submucosal plexus (plexus submucosus, s. Meissneri) and the muscular-intestinal plexus (plexus myentericus, s. Auerbachi) is observed.
Characteristic are dystrophic changes in the posterior and lateral columns of the spinal cord, mainly in the cervical region, expressed in focal swelling followed by disintegration of myelin nerve fibers. The fusion of small lesions leads to the formation of large lesions. In some cases, dystrophic changes in the cranial (cranial, T.) and peripheral nerves are observed. There is hemosiderosis of the bone marrow, spleen, liver, lymph nodes, kidneys, expressed to varying degrees. Foci of extramedullary hematopoiesis are often found in the spleen and lymph nodes.
The role of vitamin B12 for human health
The most important task of cobalamin is to participate in the synthesis of nucleic acids in cells, for example, in the bone marrow, which is responsible for the production of blood cells. Its other important task is to participate in the production and proper development of red blood cells, that is, red blood cells. These processes are important for health, because our life and the proper functioning of the body depend on their proper functioning.
Vitamin B12 has a huge impact on the functioning of the nervous system: it is involved in the formation of neurotransmitters, which affect, for example, the ability to learn and remember, as well as appetite control, good mood and hormonal regulation.
Thus, vitamin B12 indirectly affects our mood, hormonal levels, ability to concentrate and mental balance. Other tasks of cobalamin are: strengthening the body's immunity, increasing energy levels, supporting the functioning of the skeleton and muscles, as well as a beneficial effect on the course of pregnancy. In addition, it supports the treatment of mental illness and some neoplastic diseases, AIDS, arthritis and multiple sclerosis.
The recommended daily dose of B12 for adults is 2 mcg; 2.2 mcg for pregnant women; 2.6 mcg for breastfeeding women; 0.3 mcg for infants and 0.05 mcg per kilogram of body weight for children, while the daily dose should not exceed 2 mcg.
B12 anemia: diagnosis
Before starting treatment, CELT hematologists prescribe comprehensive studies to the patient, which allow them to accurately diagnose “B12-deficiency anemia” and identify the causes of its development. In addition to the hematologist, specialists in neurology and gastroenterology take part in the process. Diagnostics is as follows:
- Vitamin deficiency is detected through biochemical analysis;
- A general analysis determines the deficiency of red blood cells, leukocytes and platelets;
- Stool analysis can detect excess fat content, helminth fragments;
- The Schilling test detects failures in vitamin absorption;
- Bone marrow histology and myelogram indicate an increase in the number of megaloblasts.
In order to identify the triggering factors for malabsorption of vitamin B12 deficiency anemia in the gastrointestinal tract, the patient is prescribed gastroscopy and radiography of the stomach, as well as examination of the large intestine using an x-ray contrast agent. Other instrumental methods will also help you obtain the necessary information:
- Ultrasound scanning of the abdominal organs;
- magnetic resonance imaging of the brain;
- encephalography.
Elimination of B12 deficiency and treatment of anemia
To compensate for vitamin B12 deficiency, intramuscular injections are prescribed. Treatment lasts at least six weeks. The dosage of the drug is determined based on test results. Be sure to monitor the effectiveness of treatment with blood tests 2-3 times a week.
The identified causes of anemia are eliminated if the diseases are amenable to drug or surgical treatment. If the deficiency is caused by nutritional reasons (poor nutrition), a diet with a high content of animal proteins is developed.
If the patient's chronic disease cannot be treated, maintenance therapy with injections is carried out on an ongoing basis to prevent the development of anemia. By controlling B12 levels, people live to a ripe old age. If life is threatened (severe anemia or anemic coma), blood transfusions are used.
Under no circumstances should you self-medicate or take B12 - an excess in the body can lead to thrombosis, disruption of the gastrointestinal tract, loss of vision, increased excitability, and heart failure.
For consultation, for examination with suspected B12 deficiency anemia, cobalamin deficiency, or for a preventive examination, contact a medical specialist in Anapa. You can make an appointment with specialists by phone.
Diagnosis
The diagnosis is established on the basis of a wedge, data, a characteristic blood picture and the results of a bone marrow punctate study.
Differential diagnosis
P. a. with other megaloblastic, in particular folate-deficiency, anemias are carried out on the basis of the Schilling test, which consists in the fact that the patient has P. a. radioactive vitamin B12 administered orally and at the same time parenterally non-radioactive vitamin B12 (1000 mcg) are determined in the urine only in minimal quantities, which indicates impaired absorption of vitamin B12, which is associated either with impaired secretion of the intrinsic gastric factor, or with impaired intestinal absorption of vitamin B12; in the latter case, taking intrinsic gastric factor concentrate does not improve the absorption of vitamin B12. P. a. differentiated from symptomatic megaloblastic (pernicious-like) anemia that occurs with stomach tumors, diverticula and tumors of the small and cecal intestines, as well as with agastric, anenteral and helminthic B12-deficiency anemia (see Anemia), in which megaloblastic anemia develops as a result of impaired secretion of internal gastric factor or absorption of vitamin B12 in the intestine. P. a. also differentiate with systemic diseases, for example, erythromyelosis (see Leukemia), which is characterized by bone marrow megaloblastosis with an increased content of vitamin B12 in the blood (up to 1000 ng/ml and above) and the absence of a therapeutic effect from the administration of vitamin B12 (so-called B12 -achrestic anemia).
Clinical picture
The clinical picture is manifested by symptoms of damage to the colon. tract, nervous system and hematopoietic tissue. Weakness, fatigue, palpitations, and shortness of breath during physical exertion gradually appear. Many of the patients have been complaining for a number of years of dyspeptic disorders resulting from gastric achylia, which can be detected several years before the development of anemia, while gastric juice does not contain internal gastric factor. In 1 - 2% of cases P. a. begins with the symptoms of angina pectoris.
As a rule, the disease occurs with exacerbations, followed by remissions. The appearance of the patient during an exacerbation of the process is characterized by pallor with a lemon-yellow tint to the skin and subicteric sclera. Patients are prone to obesity. The liver is usually enlarged and soft. Sometimes a dense spleen is palpable. The temperature is occasionally low-grade. Functional (anemic) heart murmurs are heard; on the ECG - a decrease in the T wave in all leads, widening of the gastric complex.
In some patients, Gunter's glossitis is detected: at first, inflammatory phenomena (“scalded” tongue) predominate, later atrophic phenomena (“varnished” tongue) predominate. Inflammatory-atrophic changes can spread to the gums, mucous membrane of the cheeks, soft palate, pharynx and esophagus; in the latter case, dysphagia occurs (Plahmmer-Vinson syndrome). These phenomena, except for achylia, disappear during the period of remission. Gastroscopy (see) reveals nested, less often total atrophy of the gastric mucosa.
Defeat c. n. With. clinically manifested by symptoms of spinal paralysis (spastic paraparesis with increased reflexes and clonus) and tabetic symptoms (paresthesia, girdle pain, decreased reflexes up to complete areflexia, impaired vibration and deep sensitivity, sensory ataxia, dysfunction of the pelvic organs). Less common are lesions of the cranial nerves, Ch. arr. visual, auditory, olfactory. Central scotoma (see) with loss of vision is typical, quickly recovering under the influence of treatment with vitamin B12.
During exacerbation of P. a. Hyperchromic anemia is observed in the blood; it is characterized by a decrease in the number of red blood cells, which are characterized by their saturation with hemoglobin, reaching a diameter of. 12-15 microns; the color index is 1.4-1.8. There are erythrocytes with remnants of nuclei (Jolly bodies), mitotic spindle (Cabot rings), with basophilic punctation, polychromatophils, poikilocytes, schizocytes, as well as nuclear forms of erythroid cells - megaloblasts. The number of leukocytes is reduced due to granulocytopenia; myelo- and metamyelocytes, giant rod- and segmented neutrophils containing up to 12 or more segments are found. Thrombocytopenia is noted, and giant plates (megathrombocytes) are found. The content of vitamin B12 in the blood is reduced with normal or increased levels of folate in erythroid cells (the so-called methyltetrahydrofolate block) and with increased serum iron levels. During the period of remission, the blood picture gradually normalizes.
In cases of mild P. a. in 80-90% of patients, according to M. P. Nevsky, asthenic disorders are observed (see Asthenic syndrome).
In some patients, emotional-hyperesthetic weakness, fatigue, absent-mindedness, instability of attention, a feeling of weakness, a depressed-tearful mood, and hyperesthesia predominate; in others - irritability, dissatisfaction, slight excitability, increased demands. Hypochondriacal statements in patients with P. a. (see Hypochondriacal syndrome) are often associated with real somatic disorders. In cases of irogredient current P. a., especially accompanied by symptoms of funicular myelosis (see), acute and prolonged psychoses occur, the frequency of which, according to a number of researchers, ranges from 4 to 10%. Psychosis is more common in women aged 40 to 60 years. The initial disorders are determined by asthenia, the duration of which in acute cases is weeks, and in protracted cases - months. Subsequently, during an acute course, delirium most often develops (see Delirious syndrome), less often - twilight stupefaction (see) or amentia (see Amentive syndrome). Worsening of mental disorders leads to the development of stupor and coma (see).
In psychoses with a prolonged course, asthenia is followed by affective disorders, most often in the form of depression (see Depressive syndromes). Anxious-agitated states with fragmentary delusions of persecution and accusation, verbal illusions (q.v.) and hallucinations (q.v.) predominate. In some cases, depression with fear occurs. Less common are manic states with euphoria and decreased criticism (see Manic syndromes). As the wedge becomes heavier, the picture develops into a hallucinatory-paranoid state (see Paranoid syndrome), with which pronounced tactile hallucinations may occur. Features of mental disorders in P. a. lies in the variability of their intensity and the replacement of some disorders by others over short periods of time. In cases where such a “flicker” of mental disorders is absent, prolonged psychosis is limited to one condition, resembling schizophrenia (see) or manic-depressive psychosis (see). Delirious states may occur in the late stages of prolonged psychosis. In some cases, their appearance is a sign of a possible fatal outcome associated with the underlying disease. Psychoses in cases of mild P. a. may be replaced by transient symptoms of a decrease in the level of personality, and in cases of severe course, the emergence of a psychoorganic syndrome of varying severity and manifestations is observed (see).
Severe complication of P. a. is Pernicious coma (coma perniciosum), which occurs as a result of rapid anemia, leading to hypoxia and ischemia of the brain (in particular, the region of the third ventricle). In this case, loss of consciousness, areflexia, drop in body temperature and blood pressure, shortness of breath, vomiting, and involuntary urination are observed.