Quick Transition Treatment of Addison's Disease
Addison's disease (hypocorticism, chronic adrenal insufficiency) is a rare disease characterized by insufficient production of the glucocorticoid hormone cortisol and the mineralocorticoid hormone aldosterone by the adrenal glands.
Most often, hypocortisolism, which affects both men and women, occurs at the age of 30-50, but the onset (first clinical manifestation) of the disease can be observed at any age.
The worldwide prevalence of Addison's disease is 40-60 patients diagnosed with AD per 1 million people.
General information
Addison's disease is a chronic failure of the adrenal cortex, manifested in a decrease or cessation of the secretion of hormones - mineralocorticoids and glucocorticoids ( aldosterone , cortisol , cortisone , corticosterone , deoxycorticosterone and other corticosteroids).
A deficiency of mineralocorticoid hormones leads to increased sodium excretion and decreased potassium excretion, mainly in urine, but also in sweat and saliva, while electrolyte imbalance causes severe dehydration, plasma hypertonicity, acidosis , decreased circulating blood volume, hypotension and even circulatory collapse . However, if the pathology is caused by decreased ACTH , electrolyte levels remain normal or moderately altered. Whereas a lack of glucocorticoids causes the following symptoms of Addison's disease: changes in insulin and impaired carbohydrate, protein and fat metabolism. As a result, carbohydrates necessary for life are formed from proteins, blood sugar levels decrease, glycogen deposited in the liver are depleted, which is expressed in general, muscle, and including myocardial weakness. Patients' resistance to viruses and infections, injuries and various types of stress . As failure develops, cardiac output decreases and circulatory failure occurs.
If the level of plasma cortisol is reduced, then ACTH synthesis is stimulated and the level of β-lipotropic hormone , which has melanocyte-stimulating activity, which, together with tropin, produces hyperpigmentation . People not only have bronze skin, but also mucous membranes. This means that secondary failure resulting from functional disorders of the pituitary gland does not manifest itself in the form of hyperpigmentation.
This endocrine disorder is quite rare - 4-6 people per 100 thousand in statistics from different countries. It was first described by the English physician, the father of endocrinology, Thomas Addison back in 1855 in the book “On the Constitutional and Local Consequences of Diseases of the Adrenal Cortex.”
Thomas Addison and his book
CONDITION ASSESSMENT
Diagnosis in any situations related to adrenal dysfunction is complicated by the complex structure of their cortex and the deep location of the organ. Standard ultrasound is performed, but is not informative enough. To establish Addison's disease and develop a treatment program, additional study is necessary:
- blood composition (for hormones);
- urine composition (daily volume);
- peritoneal structures on x-ray;
- output flow through venous catheterization;
- structures of the gland cortex on CT.
Additionally, scintigraphy, PET, and MRI can be performed. Against the background of the pronounced clinical picture of Addison's disease, the listed manipulations have not so much a recognition function, but rather help to determine the complex of disorders that the pathology provoked and the activity of its development in order to competently build treatment. To determine the schedule of remissions and relapses, regular monitoring is carried out.
Pathogenesis
There are many mechanisms of damage to the adrenal cortex, causing insufficiency in the production of hormones - hypocorticism , or their complete absence - acorticism . These include:
- autoimmune reactions (in 85% of cases) - antibodies to the adrenal cortex are synthesized in the body - immunoglobulins M , lymphoid infiltration, fibrosis and atrophy of functioning glandular cells occur;
- infections – introduced into the adrenal glands hematogenously, most often causing caseous necrosis and calcification;
- underdevelopment ( hypoplasia );
- oncology;
- genetic defects and diseases, such as hemochromatosis ;
- injuries;
- poisoning;
- impaired sensitivity or synthesis of adrenocorticotropic hormone (ACTH) as a result of ischemia, radiation, etc.
The structure of the adrenal glands
Hormones of the adrenal cortex and their significance
Hormones produced in the morphofunctional cortical layer of the adrenal glands are corticosteroids . Among them, the most active and important are:
- Cortisol is a glucocorticoid synthesized in the zona fasciculata of the cortex. Its main function is the regulation of carbohydrate metabolism, stimulation of gluconeogenesis and participation in the development of stress reactions. The conservation of energy resources is realized through the binding of cortisol to liver receptors and other target cells, which causes activation of glucose , its storage in the form of glycogen against the background of a decrease in catabolic processes in the muscles.
- Cortisone is a glucocorticoid, second in importance after cortisol, which can stimulate the synthesis of carbohydrates and proteins, inhibit the immune system, and increase the body's resistance to stressful situations.
- Aldosterone is the main human mineralocorticoid, synthesized in the zona glomerulosa of the cortex, under its action tissues are able to retain water and chlorides, sodium reabsorption and potassium excretion are enhanced, a shift towards alkalosis occurs, blood pressure and circulating blood volumes increase.
- Corticosterone is a less significant mineralocorticoid hormone; it also has glucocorticoid activity, although half that of cortisol, which is realized primarily in stimulating liver gluconeogenesis.
- Deoxycorticosterone is a minor, low-active mineralocorticosteroid hormone that can regulate water-salt metabolism and increase the strength and endurance of striated muscles.
Etiology
Addison's disease occurs as a result of destructive processes of various origins in the adrenal cortex. The most common cause of primary damage to the adrenal cortex is tuberculosis (50-85% of cases), which develops as a result of hematogenous dissemination; Patients with Addison's disease usually exhibit specific changes in the lungs and other organs. Sometimes there are cases of isolated damage to the adrenal glands.
The cause of Addison's disease can also be hemorrhages in the adrenal glands, vascular thrombosis, syphilis, bilateral tumors or metastases of cancer in the adrenal glands, amyloid, purulent inflammation of the adrenal glands, lymphogranulomatosis, histoplasmosis. Addison's disease can also develop as a result of autoimmune damage to the adrenal glands, which is confirmed by an increase in the titer of circulating autoantibodies to adrenal tissue. In some cases, the disease may be caused by disorders in the hypothalamic-pituitary system, leading to a decrease in the secretion of ACTH or corticotropin-releasing factor. Rarely occurring familial forms of Addison's disease associated with atrophy of the adrenal cortex are hereditary in nature and are detected in homozygotes as a result of an autosomal recessive mutation.
Classification
Depending on the mechanism of development of Addison's or otherwise bronze disease, the following are distinguished:
- primary insufficiency of the adrenal cortex - the basis of the pathology is damage to the glandular structures directly;
- secondary failure - as a result of a violation of the hypothalamic-pituitary system , which normally should stimulate the adrenal cortex.
Acute adrenal insufficiency is called hypoadrenal or Addison's crisis .
Features of Addisonian crisis
Addisonian crisis develops suddenly and can threaten a person’s life. Low concentrations of hormones (cortisol, aldosterone) in the bloodstream lead to loss of consciousness or psychosis, confusion, delirium, fever , severe vomiting and diarrhea , mineral and water imbalances, pain in the legs, lower back, abdomen, low blood pressure and even cause shock .
Treatment
How to treat Addison's syndrome? Patients with Addison's syndrome require constant use of corticosteroids. In most cases, the administration of glucocorticoids alone is sufficient for full compensation; sometimes additional prescription of mineralocorticoids is required. Hydrocortisone (cortisol) is the drug of choice and is prescribed at 30 mg per day (15-20 mg early in the morning and 5-10 mg at noon). Cortisone is usually used in a daily dose of 40-50 mg. Other synthetic glucocorticoids (prednisolone, dexamethasone, triamcinolone, etc.) are less desirable because they do not have a mineralocorticoid effect. In case of severe mineralocorticoid deficiency, additionally recommended are DOXA (5 mg once a day intramuscularly), deoxycorticosterone trimethyl acetate (1 ml of a 2.5% solution parenterally once every 2-3 weeks) or fluorohydrocortisone/cortinef (0.05-0 .1 mg per day).
Excess mineralocorticoids are fraught with edema, headache, increased blood pressure, hypokalemic alkalosis and muscle weakness. In these cases, it is necessary to discontinue mineralocorticoids and prescribe potassium chloride.
In addition, patients are recommended to take increased amounts of table salt and ascorbic acid.
Pregnancy and normal childbirth are possible in women suffering from CNN. Typically, during pregnancy, the need for mineralocorticoids decreases due to increased secretion of progesterone. However, glucocorticoid intake must be increased, and in some cases parenteral hydrocortisone is required. During labor, glucocorticoids are administered intravenously.
For infectious diseases of mild or moderate severity, the dose of glucocorticoids is doubled or tripled. If the disease occurs with vomiting, as well as when symptoms of adrenal crisis appear, intensive care of the patient in a hospital is necessary. Surgical interventions in patients with congenital insufficiency are performed under the condition of intravenous administration of hydrocortisone (100-200 mg, depending on the type of operation). In the postoperative period, loading doses of glucocorticoids are reduced quickly - 2-3 days after the elimination of the stressful situation.
Causes
Addison's disease and adrenal hypofunction can develop as a result of such processes and pathologies as:
- tuberculous, syphilitic, brucellosis lesions;
- purulent inflammation;
- decreased sensitivity or ACTH deficiency;
- taking exogenous corticosteroids, which provokes adrenal atrophy;
- development of non-hormone-producing tumors;
- congenital dysfunction;
- sarcoidosis;
- amyloidosis;
- drug therapy, for example, chlodatin , etomidate , spironolactone , ketoconazole , as well as barbiturates, steroidogenesis blockers.
Possible complications and consequences
The most dangerous complication of Addison's disease is the development of Addisonian crisis, a life-threatening condition.
The reasons for its occurrence may be:
- stress (surgery, emotional stress, trauma, acute infectious diseases);
- removal of both adrenal glands without adequate hormone replacement therapy;
- bilateral adrenal vein thrombosis;
- bilateral embolism of the adrenal arteries;
- bilateral hemorrhage in the adrenal tissue.
Symptoms of Addison's disease
The symptoms of Addison's disease are most acute under stress, when the sympathetic-adrenal system is depleted and the body experiences an increased need for glucocorticoids. The pathology develops slowly and may not be noticed for several months or even years, while it progresses, and the patient experiences:
- chronic fatigue;
- muscle weakness;
- increased irritability, anxiety, restlessness, tension and short temper;
- depressive disorder;
- thirst and need to drink plenty of fluids;
- strong heartbeat and development of tachycardia ;
- changes in taste in favor of salty and sour;
- flushes of nausea, dysphagia (impaired swallowing), digestive system disorders - vomiting, diarrhea, abdominal pain;
- loses weight and loses appetite;
- dehydration and excessive urine production ( polyuria );
- tetany, paralysis, tremors and convulsions , especially after consuming dairy products and the phosphates that accumulate as a result;
- paresthesia and deterioration of sensitivity of the limbs;
- decreased levels of glucose in the bloodstream ( hypoglycemia );
- decrease in the amount of circulating blood ( hypovolemia ).
In addition, arterial and, quite often, orthostatic hypotension develops. In women, from the reproductive system, adrenal depletion causes disruption of the menstrual cycle; in men, erectile dysfunction .
Important! One of the most specific manifestations of the disease described by Addison is hyperpigmentation of the skin of those areas that are exposed to solar radiation or greater friction. Dark spots - melasma - appear all over the body and even on the gums, which is why the pathology is also known as bronze disease. Only 10% of patients do not have this symptom and this pathology is called “White Addison” .
Another pathology is known, described by Addison and manifested in the form of yellowness of the integument - Addison-Birmer anemia , develops with a deficiency of vitamin B12 and is also called pernicious anemia or malignant anemia .
Addison-Birmer disease: symptoms and features
The pathology is based on atrophy of the gastric mucosa and cessation of secretion of Castle factor . Most often occurs in older people and people over 40 years of age. In addition to the autoimmune mechanism, the cause may be strict vegetarianism , cancer, helminthiasis, gastrectomy and enteritis .
Symptoms of Addison-Beermer disease include burning of the tongue, sensitivity, dryness and inflammation of the mucous membranes, fatigue, dizziness, migraines , shortness of breath , increased heart rate, daytime drowsiness and nighttime insomnia . At the same time, dyspeptic disorders are added - anorexia , diarrhea . Very often, patients seek medical help with significant anemia.
Addison-Biermer anemia is treated with injections of vitamin B12 , and is also aimed at normalizing hemoglobin .
Publications in the media
Addison's disease (bronze disease, chronic adrenal insufficiency) is a chronic insufficiency of the adrenal cortex that occurs when they are damaged bilaterally, leading to a decrease (or complete cessation) of the secretion of GC and mineralocorticoids. Addison's disease occurs when more than 90% of the adrenal tissue is affected. In 80% of cases, the cause of the disease is an autoimmune process, followed by tuberculosis in frequency. As a syndrome, chronic adrenal insufficiency is present in a variety of inherited diseases. Statistical data. In the United States, it is approximately 4–6:100,000. Idiopathic autoimmune Addison's disease affects women more often than men.
Etiology and pathogenesis. 80% of cases are autoimmune damage to the adrenal cortex, 10% are adrenal tuberculosis. Other, more rare causes: • Iatrogenic causes (bilateral adrenalectomy, consequences of long-term GC therapy) • Fungal diseases (histoplasmosis, blastomycosis, coccidioidomycosis) • Sarcoidosis • Hemorrhages into the adrenal glands • Tumors • Amyloidosis • Acquired immunodeficiency syndrome (AIDS) - due to CMV and other infectious lesions of the adrenal glands • Syphilis • Adrenoleukodystrophy. It is accompanied by an increase in the level of ACTH, together with a-melanocyte-stimulating hormone, causing hyperpigmentation of the skin and mucous membranes - a hallmark of Addison's disease, for which reason it is also called bronze disease.
Secondary adrenal insufficiency is caused by pituitary insufficiency (ACTH deficiency); unlike primary, it is never accompanied by hyperpigmentation.
Genetic aspects. Manifestations of Addison's disease are observed in a number of inherited conditions • Adrenoleukodystrophy • Congenital Addison's disease (103230, Â): skin hyperpigmentation, hypernatriuria, hypokaliuria • Familial hypoadrenocorticism (*240200, r): vomiting, skin pigmentation, seizures, vascular collapse, hypoglycemia, hyponatremia , hyperkalemia • Familial adrenal hypoplasia (*300200, Xp21.3–p21.2, DAX1, r gene defects) • GK receptor defects (*138040, 5q31, GRL gene, Â; also *202200 [MC2R gene defect, 18p11 .2, r]): no response to ACTH, arterial hypertension; severe arterial hypertension and hypokalemic alkalosis in homozygotes • Glycerol kinase deficiency (307030) • Allgrove's syndrome (syndrome 3A [from: Adrenal insufficiency, Achalasia, Alacrimia], *231550, r): Addison's disease, achalasia, alacrimia; the adrenal glands lack the zona reticularis • Autoimmune polyglandular syndrome.
Risk factors • Adrenal insufficiency of an autoimmune nature in relatives (first or second degree) • Treatment with GC for a long time, as well as severe infections, injuries or surgical interventions.
Clinical manifestations. The clinical picture consists of signs of GC and mineralocorticoid deficiency. The predominance of certain manifestations is determined by the duration of the disease.
• Hyperpigmentation of the skin and mucous membranes (in primary failure) often precedes other clinical manifestations by months or years. The simultaneous presence of vitiligo due to autoimmune destruction of melanocytes is possible.
• General symptoms: severe weakness (primarily muscle), fatigue, weight loss, poor appetite.
• Arterial hypotension, especially orthostatic, is accompanied by dizziness and sometimes syncope episodes. Also, due to hypotension, patients note poor tolerance to cold.
• Signs of gastrointestinal damage: nausea, vomiting, episodic diarrhea.
• Possible mental disorders (depression, psychosis).
• Strengthening gustatory, olfactory, auditory sensitivity; An irresistible desire for salty food may appear.
Adrenal (adrenal) crises. They are based on a sudden deficiency of GC and mineralocorticoids due to an increase in the need for them or a sudden decrease in their production against the background of pre-existing chronic adrenal insufficiency. Causes • Stress (25% of cases): acute infectious disease, trauma, surgery, emotional stress and other stressful effects; adrenal crises in these situations are provoked by the lack of an adequate increase in doses of hormone replacement therapy. In addition, it should be borne in mind that when prescribing inducers of microsomal liver enzymes (for example, rifampicin), the dose of hormones must be adjusted • Bilateral hemorrhage in the adrenal glands - see Waterhouse-Friderichsen syndrome • Bilateral embolism of the adrenal arteries or thrombosis of the adrenal veins (for example, during radiocontrast studies) • Bilateral adrenalectomy without adequate replacement therapy.
Manifestations: arterial hypotension, abdominal pain, vomiting and disturbances of consciousness. Laboratory changes - hypoglycemia, hyponatremia, hyperkalemia, metabolic acidosis.
Concomitant pathology • Diabetes • Thyrotoxicosis • Thyroiditis • Hypoparathyroidism • B12-deficiency anemia • Ovarian dysfunction • Hypercalcemia • Chronic candidiasis.
Laboratory data. Diagnosis of chronic adrenal insufficiency comes down to identifying insufficient functional capabilities of the adrenal cortex (increase the synthesis of cortisol in response to stimulating influences).
• Short test with ACTH. The content of cortisol in the blood serum is determined before and 30 minutes after the intravenous administration of corticotropin (0.25 mg). If the patient does not have Addison's disease, the serum cortisol concentration increases by at least 7 mcg% (reaching 18 mcg% or more), and after 30-60 minutes reaches 20 mcg% or more. In Addison's disease, the concentration increases slightly or does not change.
• Standard ACTH test (more accurate). ACTH (25–40 units) is administered intravenously over 8 hours. The day before the study and on the day of the study, the content of free cortisol (or 17-hydroxycorticosteroids) in 24-hour urine is determined. The concentration of cortisol in the blood serum is also determined immediately before the administration of ACTH and after 6–8 hours. To prevent the development of adrenal insufficiency in the patient, dexamethasone (0.5 mg every 6 hours) is administered during the test. Normally, urinary excretion of corticosteroids increases 3–5 times, and the concentration of cortisol in the blood serum increases to 15–40 μg%. In Addison's disease, the increase is slight (or absent)
Additionally: • Hyponatremia (less than 130 mmol/l) • Hyperkalemia (more than 5 mmol/l) • Increased blood urea nitrogen • Hypoglycemia • Decreased cortisol, increased renin levels (radioimmunoassay) • Increased ACTH levels (in case of secondary deficiency - decreased ) • Decreased concentration of 17-hydroxycorticosteroids in urine • Moderate neutropenia and eosinophilia.
Instrumental data • CT scan of the abdominal cavity •• Small size of the adrenal glands (atrophy or a consequence of long-term tuberculosis) •• Enlargement of the adrenal glands (early stage of tuberculosis or other potentially curable diseases) • X-ray of the abdominal organs: may reveal calcification of the adrenal glands • X-ray of the chest: identification of possible adrenal calcification and reduction in heart size • ECG: low-voltage QRS complex with nonspecific changes in the T wave and ST segment; sometimes changes characteristic of hyperkalemia.
Diagnostic tactics. Characteristic clinical manifestations (hyperpigmentation in combination with arterial hypotension and other signs) suggest a diagnosis. To confirm it, it is necessary to consistently conduct laboratory and instrumental examinations.
Differential diagnosis • Myopathies • Hypoglycemia due to other causes • Syndrome of inappropriate secretion of antidiuretic hormone (ADH) • Salt-wasting form of adrenogenital syndrome • Heavy metal poisoning • Hemochromatosis • Anorexia nervosa • Sprue • Hyperparathyroidism.
TREATMENT
Lead tactics. Treatment of adrenal insufficiency using gluco- and mineralocorticoid replacement therapy. Appropriate treatment of the underlying disease (eg, tuberculosis). Emergency treatment of adrenal crisis.
The mode is outpatient, in case of adrenal crisis - emergency hospitalization.
Diet. A sufficient amount of proteins, fats, carbohydrates and vitamins, especially C and B1 (rosehip decoction, black currant, yeast are recommended). Table salt is consumed in increased quantities (20 g/day). The content of potassium salts is reduced to 1.5–2 g/day. The diet reduces the content of potatoes, peas, beans, beans, dried fruits, coffee, cocoa, chocolate, nuts, and mushrooms. Vegetables, meat, and fish must be consumed boiled. The diet is divided; a light dinner (a glass of milk) is recommended before bedtime to prevent a hypoglycemic state in the morning.
Drug therapy. The goal of pharmacotherapy is to reduce the incidence of complications and mortality.
• Treatment of chronic adrenal insufficiency is replacement therapy with GCs and mineralocorticoids. Hydrocortisone and fludrocortisone are used •• Hydrocortisone 10 mg in the morning and 5 mg orally daily after lunch (adults up to 20–30 mg/day) •• Fludrocortisone 0.1–0.2 mg orally 1 time per day. With the development of arterial hypertension, its dose should be reduced. In acute illness or after a minor injury, the dose of steroid hormones is doubled until you feel better. During surgical treatment, before and (if necessary) after surgery, the dose of steroid hormones is adjusted. In case of liver diseases, as well as in elderly patients, the dose of drugs should be reduced.
• Treatment of adrenal crisis 1) Emergency provision of venous access with intravenous infusion of 0.9% sodium chloride solution until dehydration and hyponatremia are eliminated. 2) Hydrocortisone - 100 mg immediately IV over 5 minutes, then infusion of 300 mg over 24 hours (100 mg in the first 2 hours); On the second day, 150 mg is usually administered, on the third - 75 mg. Clinical improvement (assessed primarily by blood pressure recovery) usually occurs after 4–6 hours of infusion. If there is no improvement, the diagnosis should be reconsidered. 3) Identification and elimination of the provoking factor. 4) During rehydration, hyperthermia and psychotic reactions often develop • For hyperthermia (against the background of normal blood pressure), antipyretics are prescribed, for example, acetylsalicylic acid 500 mg every 30 minutes until the body temperature decreases • If psychotic reactions develop after the first 12 hours of treatment, the dose of hydrocortisone should be reduced to the minimum effective.
Long-term observation. Lifelong medical supervision is indicated to constantly monitor the adequacy of the therapy and to exclude an overdose of hormones taken. The adequacy of therapy is assessed using the following parameters: blood pressure, heart rate, concentration of electrolytes in the blood plasma, plasma renin content, appetite, physical activity, fasting blood glucose concentration.
The patient must be provided with complete information about the clinical manifestations of adrenal crisis, incl. and early, in order to be able to timely increase the dose of hormones taken and prevent the development of serious symptoms • If nausea and vomiting prevent the intake of drugs orally, the patient should seek medical help for parenteral therapy • During surgical interventions, it is necessary to adjust the dose of steroid hormones • Should be avoided infectious diseases.
Complications • Adrenal (adrenal) crisis • Hyperkalemic periodic paralysis (rare) • Reactive psychoses.
Forecast. Favorable with adequate therapy. Life expectancy is close to normal.
Age characteristics • Children: •• Diagnosis is more difficult •• Develops in siblings (siblings) •• Doses of hydrocortisone and fludrocortisone should be lower than in adults • Elderly. Adrenal crisis occurs more often.
ICD-10 • E27.2 Addison's crisis • E27.1 Primary adrenal insufficiency • A18.7+ Adrenal tuberculosis (E35.1*)
Note. Addisonism - symptoms of Addison's disease without damage to the adrenal cortex.
Application. Alacrimia - lack of tear production, discomfort in the eye area; leads to the development of xerophthalmia, clouding of the cornea. A congenital form is known (*103420), the result of hypoplasia of the lacrimal gland. Alacrimia also accompanies Lesch-Nyen syndrome and ectodermal anhydrotic dysplasia. ICD-10. H04.1 Other diseases of the lacrimal gland.
Tests and diagnostics
To confirm Addison's disease you need to do:
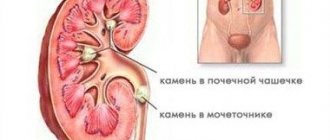
- ultrasound examination of the adrenal glands to identify lesions, for example in tuberculosis ;
- blood test to determine the level of adrenal hormones (cortisol), ACTH, glucose, potassium, sodium, renin ;
- CT scan of the adrenal glands, which allows you to detect adrenal infarction, reduction in size, tumor metastases, amyloidosis;
- MRI of the brain to study the hypothalamic-pituitary region and detect destructive, tumor or granulomatous processes.
The basis for diagnosing Addisonian crisis is:
- a decrease in sodium concentration in the bloodstream below 130 mmol/l, excretion in urine - less than 10 g per day;
- an increase in potassium concentration in the bloodstream over 5 mmol/l;
- a drop in the ratio of sodium to potassium ions to 20 units (normally 32);
- low glucose levels;
- development of acidosis;
- high concentrations of urea , residual nitrogen in blood plasma tests.
Flow
The course of Addison's disease is chronic, progressive, with exacerbations during incoming diseases (infections), forced surgical interventions, injuries, etc. Sometimes quite long periods of some improvement are observed.
On average, the disease lasts 2-3 years, and sometimes drags on for a longer period (up to 10 years). However, fast-flowing, acute forms are also known.
Untreated patients usually die from cachexia. Often, death is associated with some kind of infectious disease, which occurs non-reactively (without fever, without changes in the blood picture) and which patients with bronze disease usually tolerate very hard. Along with severe forms, milder forms are also known, when the symptoms of Addison's disease are much less pronounced. In these cases, they do not talk about Addison's disease, but about Addisonism.
Diet for adrenal insufficiency
Diet 15 table
- Efficacy: therapeutic effect after 2 weeks
- Timing: constantly
- Cost of food: 1600-1800 rubles per week
In addition to the fact that the patient needs to avoid hypothermia and stressful situations, a diet rich in carbohydrates is recommended. You need to add foods with a high amount of ascorbic acid (black currants, citrus fruits, rosehip decoction) and an additional 15-20 g of table salt per day to your diet.
To prevent hyperkalemia, it is better to limit the consumption of potassium-rich dried apricots, raisins, legumes, and potatoes.
Diagnosis
The diagnosis is based on the characteristic clinical picture and laboratory tests. Skin pigmentation in Addison's disease must be differentiated from sun tanning, combined with hypotonic syndrome, with skin pigmentation in toxic diffuse goiter, hemochromatosis, pellagra, acanthosis, pruritic dermatoses, chronic malaria, scleroderma, and salt-wasting form of nephritis. Pigmentation of the oral mucosa is also observed in chronic poisoning with arsenic, silver nitrate, mercury, and lead.
Prevention
Prevention of Addison's disease consists mainly in correct and timely treatment of tuberculosis (see) and other diseases that are etiological factors of Addison's disease.
Bibliography:
Baranov V. G. Diseases of the endocrine system and metabolism, L., 1955; Zefirova G.S. Addison's disease, M., 1963, bibliogr.; Soffer L., Dorfman R. and Gebrilav A. Human adrenal glands, trans. from English, p. 207, M., 1966; Shereshevsky N. A. Clinical endocrinology, p. 185, M., 1946; Addison T. On the constitutional and local effects of disease of the suprarenal capsules, L., 1855; Brenner O. Addison's disease with atrophy of the cortex of the suprarenale, Quart. J. Med., v. 22, p. 121, 1928-1929; Guttman PH Addison's disease, Arch. Path., v. 10, p. 742, 895, 1930; Hall R., Anderson J. a. Smart GA Fundamentals of clinical endocrinology, L., 1969; Human adrenal cortex, ed. by AR Currie ao, Baltimore, 1062; K & das I. Die latente Addisonische Krankheit, Z. gee. inn. Med., S. 140, 1970; Paschkis K. E.. Ra-koff AE a. Gantarow A. Clinical endocrinology, NY, 1958; Textbook of endocrinology, ed. by R. Y. Williams, Philadelphia - L., 1963.
G. S. Zefirova; V. B. Zairatyants (pat. an.).