Perthes disease (full name Legg-Calvé-Perthes disease) is a fairly common pathology of the hip joint in children aged 3 to 15 years and is an aseptic necrosis of the femoral head and impaired blood supply to the cartilage tissue of the joint. Necrosis is aseptic and not associated with infection. Perthes disease is more common in boys, but in girls the disease is more severe. As a rule, one joint is affected, but in a certain percentage of cases there is bilateral joint damage.
The causes of this disease are not fully understood, but certain mechanisms of pathogenesis have become clear in recent years.
First of all, a certain genetic determination is required (that is, the presence of myelodysplasia). Myelodysplasia means underdevelopment of the spinal cord. As a rule, myelodyspasia is moderate and manifests itself only as a disturbance in the development of innervation of the hip joint, which is manifested by various orthopedic diseases (including Perthes disease). Underdevelopment of innervation is accompanied by underdevelopment of the vascular network, which is responsible for the blood supply to the joint and a decrease in vascular tone. But for the development of aseptic necrosis, a complete cessation of blood flow to the head of the hip bone is necessary. Such conditions occur when a joint becomes inflamed or a joint is injured.
The inflammatory process in the joint can be reactive in nature to previous infections (acute respiratory infections, ENT diseases). As a rule, the symptoms of Perthes disease are associated with minor injuries or viral diseases, which is noted by the parents of patients. As a result of a combination of genetic underdevelopment of innervation and blood supply and in the presence of provoking factors (trauma or infection), the circulation of the femoral head is impaired, which leads to partial or complete necrosis of the area with impaired blood supply. First, necrosis occurs in the ossification core of the femoral head, then a compression fracture is possible in this part of the femur and then resorption of necrotic tissue and replacement of bone tissue with connective tissue, which in turn calcifies after some time. All this leads to shortening of the femoral neck, disruption of the structure of the acetabulum, and these anatomical disorders lead to disruption of the biomechanics of movements in the hip joint.
Causes
The disease is still being studied, since the main cause of its manifestation has not yet been identified.
There are such theories of the occurrence of pathology:
- Traumatic - the root cause is damage to the head of the hip bone and its displacement.
- Hormonal – the main trigger is hormonal imbalance at certain periods in children’s lives
- Infectious - a reaction to damage to the joint by viruses, infectious agents and the corresponding response of the immune system to their vital activity.
- Metabolic - a failure in the metabolism of various minerals (calcium, phosphorus), which take an active part in the formation of bone tissue.
- Genetic predisposition.
It is noted that the following groups of children are at risk:
- with weakened immunity;
- after suffering from rickets;
- with congenital myelodysplasia of the lumbar spinal cord;
- with frequent diseases of infectious and allergic origin;
- with nutritional deficiency.
The combination of several causes of the development of Perthes disease and the child being at risk increases the likelihood of developing the pathology.
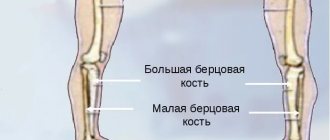
Osteochondropathy of the tibia
This pathology is a severe degenerative-dystrophic process in bone tissue due to disruption of its blood supply, structure and fatty degeneration of the bone marrow. The disease is classified as polyetiological, but there are a number of main factors that increase the risk of developing necrosis:
- Injuries and dysplasia.
- Toxic effects of drugs.
- Osteopenia.
- Osteoporosis.
- Rheumatoid arthritis.
- Cardiac ischemia.
The pathological condition is manifested by pain in the area of the hip joint and groin, which can radiate to the knee, lower back, and sacrum. As the disease progresses, the discomfort becomes permanent. The patient begins to limp, the affected limb loses its mobility due to muscle atrophy.
Diagnosis of aseptic necrosis of the tibia consists of plain radiography, MRI, CT, and soft tissue scintigraphy. Treatment is conservative: physiotherapy, medication, exercise therapy. Surgery is possible for serious degenerative changes.
Osteochondropathy of the fibula
The fibula is a tubular, thin and long part of the lower leg. It connects to the tibia and consists of a body and two ends. Serves as an external stabilizer of the ankle joint.
Degenerative-dystrophic lesions of the fibula often occur against the background of necrosis of the pelvic bones and are manifested by the following signs: widening of the joint space, decreased height of the epiphyses, and death of bone tissue.
The disease causes pain when moving and palpating the affected area. The pathology is characterized by a cyclical course. Its total duration takes from 2 to 4 years. The treatment is complex: medications, physiotherapy, exercise therapy, mineral complexes.
Osteochondropathy of the tibial tuberosity
Osgood-Schlatter disease is one of the common forms of avascular necrosis in children. Damage to the tibial tuberosity is diagnosed in patients 10-18 years old who are actively involved in sports. The disease can be either unilateral or with symmetrical damage to both limbs.
The main cause of the disorder is frequent injuries and increased physical activity. The degenerative-dystrophic process is manifested by the following symptoms:
- Swelling of the lesion.
- Local pain on palpation and flexion of the limb.
- Upon palpation, a hard bone growth is determined.
In the first stages, discomfort is periodic. As the pain progresses, it becomes persistent and intensifies when walking or squatting. Due to edema, there is a moderate deformity of the anterior proximal part of the leg. This is clearly visible from the side with the knee joint bent. The tuberosity can be an elastic or dense bone structure.
When making a diagnosis, radiological signs of pathology are taken into account. There is a change in the structure and contours of the tibial tuberosity - light areas alternate with dark and structureless ones, and a marginal cavity is formed. Differentiation is carried out with recurrent subluxation of the patella, tumors of cartilage tissue, avulsion fracture of the tibial tuberosity, osteomyelitis, and infrapatellar bursitis. Treatment consists of limiting flexion movements in the knee joints of the affected limb. Patients are prescribed painkillers, bone tissue and body strengthening medications. Physiotherapy is aimed at stimulating regenerative processes. Surgical intervention is performed extremely rarely, since there is a risk of damage to the growth zone and the development of synostosis. The disease lasts 1-1.5 years and ends with restoration of the bone structure. In advanced cases, deformation of the lesion may occur.
Symptoms
Symptoms vary depending on the stage of the pathology. There is a connection between progression after infections and inflammation in the throat and nasopharynx - sinusitis, sore throat.
Characteristic features:
- Pain when moving. Dull, not severe pain in the area of the affected joint, knee, or along the entire length of the limb.
- Changes in gait - lameness, dragging of the leg or falling on it.
- Swelling in the joint area.
- Motor limitation - in the affected area it is difficult to turn, bend, or turn outward.
- Low-grade fever.
- Autonomic symptoms: severe sweating of the foot, pallor of the skin, wrinkling, decreased pulse in the foot and toes, and hypothermia.
- Weakness of the gluteal muscles.
A laboratory blood test reveals an increase in lymphocytes and an increase in ESR with leukocytosis.
Severe pain and other signs that cause severe discomfort indicate deformation of the head of the bone and a fracture, and therefore require immediate treatment.
Do you still think that it is impossible to cure your joints?
Judging by the fact that you are now reading these lines, victory in the fight against inflammation of cartilage tissue is not yet on your side...
Have you already thought about inpatient treatment? This is understandable, because joint pain is a very dangerous symptom, which, if not treated in a timely manner, can result in limited mobility. Suspicious crunching, stiffness after a night's rest, the skin around the problem area is stretched, swelling in the sore spot... All these symptoms are familiar to you firsthand.
(function(w, d, n, s, t) { w = w || []; w.push(function() { Ya.Context.AdvManager.render({ blockId: 'RA-264775-2', renderTo : 'yandex_rtb_R-A-264775-2', async: true }); }); t = d.getElementsByTagName('script'); s = d.createElement('script'); s.type = 'text/javascript '; s.src = '//an.yandex.ru/system/context.js'; s.async = true; t.parentNode.insertBefore(s, t); })(this, this.document, 'yandexContextAsyncCallbacks '); var m5c73e28728432 = document.createElement('script'); m5c73e28728432.src='https://www.sustavbolit.ru/show/?' + Math.round(Math.random()*100000) + '=' + Math.round(Math.random()*100000) + '&' + Math.round(Math.random()*100000) + '= 7388&' + Math.round(Math.random()*100000) + '=' + document.title +'&' + Math.round(Math.random()*100000); function f5c73e28728432() { if(!self.medtizer) { self.medtizer = 7388; document.body.appendChild(m5c73e28728432); } else { setTimeout('f5c73e28728432()',200); } } f5c73e28728432(); window.RESOURCE_O1B2L3 = 'kalinom.ru';
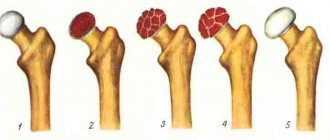
Classification
Aseptic necrosis, which is the mechanism of development of Perthes disease, consists of necrosis of bone tissue in the upper hemisphere of the head of the bone.
Necrotic process of non-infectious etiology - the lesion develops without pus and microorganisms.
The current classification has been in use since 1928. There are 5 stages of the disease:
- Stage 1 - primary subchondral-aseptic necrosis of the bone marrow and spongy substance of the femoral head;
- Stage 2 - impression syndrome - secondary depressed fracture of the head;
- Stage 3 - fragmentation - resorption of dead areas, accompanied by shortening of the bone;;
- Stage 4 - proliferation of connective tissue;
- Stage 5 - restoration of the structure of the spongy substance.
Gradual changes lead to deformation, shortening of the bone with the development of lameness and motor limitations. If left untreated, the disease leads to disability.
Prevention and prognosis
People who have been treated for Perthes syndrome are advised to avoid increased stress on the “affected” limb for the rest of their lives. The main contraindications are running, lifting weights, and jumping. Among the workouts, it is better to give preference to swimming and cycling. You should not choose a job that requires you to be on your feet for a long time.
In addition, you should perform a therapeutic set of exercises daily to develop the “problem” joint and strengthen the thigh muscles. At least once a year, it is recommended to undergo preventive treatment in orthopedic sanatoriums. With timely measures taken, the prognosis for patients with the pathology under study is favorable.
So, Perthes disease is classified as an osteochondropathy and is an aseptic necrosis of the head of the hip joint due to impaired blood supply to this joint. Pathology develops for various reasons (from congenital anomalies to complications of ARVI), and is treated with medication and surgery. The lack of timely treatment measures leads to deterioration in motor activity, shortening of the limb and, as a consequence, disability.
Diagnostics
To determine the disease and prescribe therapy, you must seek help from an orthopedist.
The main method that allows you to obtain complete information about the stage of the lesion and the location of the damage is an x-ray of the hip joint in different projections.
Diagnosis of stage 1 is difficult; at stages 2-5, changes are obvious. To complement the clinical picture at the initial stage of development of the disease, an ultrasound of the joint or CT may be needed.
What is Legg Calve Perthes disease?
Perthes disease is a degenerative pathology affecting the femur and hip joint (HJ), belonging to the group of osteochondropathy. The trigger for the development of the disease is a circulatory disorder in the hip joint, often against the background of deteriorating innervation. The joint tissues are constantly experiencing a deficiency of nutrients and oxygen. Because of this, some of the tissue begins to gradually die, which leads to the formation of an area of aseptic necrosis. This process is not accompanied by inflammation, including infectious origin.
Treatment
Initially, Legg-Calvé-Perthes disease requires removal of the load from the leg - cuff traction, movement on crutches, as well as the active use of physiotherapeutic techniques.
More serious manifestations require surgery with further rehabilitation.
Conservative treatment
Non-surgical treatment is aimed at reducing the load on the affected joint and stimulating the resorption of dying tissue, as well as maintaining muscle tone during the period of forced motor limitation.
Apply:
- plastering;
- application of immobilizing orthopedic structures;
- medicinal and non-medicinal methods of activating blood flow in the affected area.
The peculiarity of therapy is its duration - at least a year of treatment in a hospital setting.
Active load can be prescribed from the 4th stage, and from the 5th stage exercises are introduced to restore the functioning of the joint and muscles.
Surgical intervention
Surgery is rarely required - in especially advanced cases.
There are 3 types of surgical interventions:
- Joint endoprosthetics.
- Tunneling. It consists of drilling several channels in the femoral neck, which are subsequently filled with granulation tissue, densely permeated with blood vessels. This improves blood flow and eliminates the problem.
- Elimination of mutual pressure between joint surfaces (arising from cramps) and muscle contractures.
The rehabilitation period after surgery or treatment without surgery is aimed at preventing infection, tissue necrosis, and restoring the functioning of the joint and muscles.
Physiotherapy
At various stages of restoration of bone structure, joint and muscle function, various types of physiotherapeutic techniques are used.
Shown:
- Shock wave therapy effectively restores blood flow, relieves pain, and improves metabolic processes.
- Diathermy - heating with high-frequency currents is used to relieve pain, improve blood and lymph circulation, and activate the work of macrophages and leukocytes.
- Electrophoresis (with calcium and phosphorus) - improves blood flow and metabolic processes.
- Thermal procedures are aimed at increasing blood flow.
- Diet food. The diet includes foods rich in fat-soluble vitamins, protein, and calcium.
Loading the joint after treatment is possible only during a control ultrasound, CT scan or radiography.
List of sources
- Osteochondropathies of the hip joint. Shevtsov V.I. – M.: Medicine. 2007;
- Akhtyamov I.F., Abakarov AA, Beletsky AB Diseases of the hip joint in children. Diagnosis and surgical treatment. Kazan; 2008;
- Abalmasova E.A. Osteochondropathies. In the book: Pediatric arthrology. M.: Medicine; 1981;
- Gafarov Kh. Z. Treatment of children and adolescents with orthopedic diseases of the lower extremities. Kazan: Tatar book. publishing house, 1995;
- Osteochodropathy. Anashev T.S. - Guidelines. – 2004.
Forecasts
Perthes disease is not life-threatening, but advanced stages of joint damage can cause disability. The development of deforming arthrosis, lameness, and limited mobility is likely.
With complete relief from the disease, some restrictions remain for life, namely, you need to avoid:
- overloads;
- heavy physical work;
- sprains in the joint area;
- traumatic sports.
If discomfort in the joint area recurs, you should consult an orthopedist.
Legg-Calvé-Perthes disease can be successfully treated without the use of complex surgical operations if it is detected at the initial stage of development. To do this, it is necessary to promptly respond to symptoms - lameness, complaints of pain, and also be sure to consult with an orthopedist after injuries suffered by the child.
What are the outcomes of the disease?
The main circumstances for determining the outcome of Perthes disease are the age of children in the initial period of the pathological process, the location and size of necrosis in the head of the femur, timely diagnosis and correct implementation of therapeutic measures.
The prognosis of the disease is no less influenced by the conscientiousness of the child and his parents following the recommendations for further treatment given by the orthopedic doctor. The main ones are: eliminating excess physical activity (jumping, running, lifting weights, etc.) and reducing excess body weight throughout subsequent life. In this regard, the child is not allowed to participate in almost all types of sports and physical education at school - at best, he is allowed to attend a special group without passing the standards. The physical activity of such children should be manifested in the form of some acceptable types of exercise - swimming in the pool, therapeutic exercises to maintain a normal range of motion in the joint, exercise on an exercise bike and a sports bike. Otherwise, developing physical inactivity almost always leads to excess weight, which becomes a serious additional problem for the patient.
Osteochondropathy of the patella
Sinding-Larsen-Johanson disease is avascular necrosis of the patella. Most often, this pathology is detected in patients 10-15 years old. The disease is classified as polyetiological. The degenerative process may be associated with the rupture and separation of a section of bone tissue from the patella due to increased function of the quadriceps muscle.
Symptoms of pathology:
- Increasing pain in the knee joint.
- Swelling of the soft tissues of the affected area.
- Quadriceps muscle atrophy/strain.
In some cases, osteochondropathy of the patella occurs against the background of necrosis of the tibial tuberosity, that is, Osgood-Schlatter syndrome.
Various instrumental techniques are used for diagnosis. The radiograph reveals damage to the cortical layer of the anteroinferior part of the patella, fragmentation of its lower pole, and periostitis.
Treatment consists of a complex of conservative methods. Patients are recommended to unload the joint, physiotherapy, and massage. If the disease does not respond to conservative treatment, then surgery is performed to remove the affected bone.
Apophyseal osteochondropathy
Scheuermann-Mau disease is an aseptic necrosis of the apophyses, that is, the processes of the vertebral bodies. This form of the disease is most often diagnosed in patients during the period of intensive growth, that is, 11-18 years. The main cause of the pathology is congenital defects in the development of intervertebral discs, a violation of the strength of the endplates of the vertebral bodies. Risk factors include endocrine diseases, functional overload, and injuries. That is, disruption of the ossification process in the growth zone of the vertebral bodies leads to their necrosis and deformation.
Degenerative-dystrophic processes are typical for the VII, VIII, IX and X thoracic vertebrae. Damage to the thoracolumbar and lumbar regions is also possible. Symptoms of the disease depend on its stage.
The main signs of necrosis:
- In the first stage, pain is minimal. Possible asymmetry of the shoulder blades, slightly increased thoracic kyphosis, paravertebral asymmetry. At the level of pathological changes, the spinous processes protrude, palpation of which causes pain. It is also possible to limit the tilt of the body.
- The second stage is characterized by the appearance of ossification of the apophyses. Back pain occurs when walking or sitting for a long time, increased fatigue and muscle weakness of the legs and back. Increased thoracic kyphosis, deformity. Radicular syndrome develops with limited mobility of the vertebrae.
- The third stage is the fusion of the apophyses with the vertebral bodies. It is characterized by kyphosis and wedge-shaped deformation of the vertebral bodies, signs of spinal arthrosis with acute pain syndrome. Fixed kyphosis and lumbar lordosis cannot be corrected.
Diagnostics consists of a complex of instrumental and differential techniques. Treatment in most cases is conservative. Patients are prescribed general strengthening procedures, taking vitamins, and a gentle regime of work and rest. To develop correct posture, you need to choose a hard mattress; it is also possible to wear a special corset - a posture corrector.
Swimming, back massage, and physiotherapeutic procedures have a healing effect. In case of severe kyphosis with neurological complications, surgical intervention is performed. With timely treatment, the disease has a favorable prognosis.
The program usually includes
- orthopedic aid;
- individual physical therapy classes with an instructor;
- therapeutic medical massage;
- physiotherapy (electrophoresis, magnetic therapy, myostimulation, amplipulse therapy);
- osteopathic treatment and manual therapy;
- kinesio taping (according to indications);
- psychological assistance to the child and his family;
- drug therapy.
Kinesio taping
Amplipulse (SMT therapy)
Electrophoresis
Myostimulation (electrical stimulation)
If you need help, we are always ready to help!
Phone numbers for appointments +7 (812) 425-67-96 or +7 (921) 947-60-41.