Bone cysts can develop in children and adults. Pathogenic factors may include traumatic effects, inflammatory processes, necrotization due to hypoxia and ischemia in some vascular pathologies. Adolescents whose bodies produce excess amounts of hormones are at risk. Under their negative influence, partial softening of the bone tissue of the tubular bones occurs. In this regard, even a minor bruise in boys and girls aged 12–15 years can provoke the development of an internal cavity at the base of the femur, tibia, and humerus.
In adults, a bone cyst can be located at the base of the vertebrae, leading to narrowing of the spinal canal and compression of the spinal cord structures. This pathology accompanies all degenerative dystrophic processes. Thus, with osteochondrosis, degeneration occurs not only of the fibrous ring of the intervertebral disc. The subchondral endplates suffer from dehydration and dysfunction. They are simultaneously responsible for partial blood supply to the cartilage tissue of the synovial membrane of the joint and for providing nutrition to the bone structure. The subchondral endplate is dotted with blood capillary vessels. If it is subjected to constant compression, its sclerotic destruction begins. As a result, the underlying periosteum and bone tissue do not receive enough oxygen and nutrients. Ischemia, neurosis, destruction and activation of the action of lysozymes (enzymes that destroy and utilize bone tissue) begin.
Before treating a bone cyst, it is necessary to study all possible causes of its formation. After this, the doctor will be able to develop an individual treatment plan that will completely restore the functionality of the damaged limb or spinal column.
If you need treatment for a bone cyst, you can make an appointment with an orthopedist or vertebrologist at our manual therapy clinic in Moscow. The initial consultation is provided completely free of charge for all patients. Call the administrator and agree on a time convenient for your visit.
Causes of bone cyst
The main causes of bone cysts are the processes of destruction of healthy tissue by lysosomal enzymes, which are drawn into areas of accumulation of necrotic tissue, capillary blood, pus and leukocyte mass. Lysosomal enzymes are responsible for the timely “disposal” of damaged tissues and their removal from the source of accumulation. Then the process of filling the resulting cavity with healthy tissue begins. This happens in most cases.
But sometimes there is a malfunction in the mechanism. After cleansing the lesion with lysosomal enzymes, it is not filled with healthy cells of authentic tissue. A cavity remains. There is an effusion of lymphatic and intercellular fluid into it. Secondary aseptic inflammation may occur, internal pressure increases, a repeated process of tissue breakdown starts, etc.
The main reasons for the formation of bone cysts in children and adults are the following negative factors:
- metabolic disorders, including overweight, obesity, slow metabolism;
- hormonal disorders and endocrine diseases associated with excess or decreased production of hormones of the thyroid gland, pituitary gland, adrenal glands, ovaries, etc.;
- disruption of the process of calcium absorption due to vitamin D deficiency or chronic inflammatory processes in the large intestine;
- calcium deficiency in the diet;
- impaired blood supply to the spinal column, upper and lower extremities (varicose veins, atherosclerosis, diabetic angiopathy, obliterating endarteritis, etc.);
- traumatic effects (impacts, bruises of soft tissues and periosteum, fractures, cracks, sprains of ligaments and tendons, etc.);
- disruption of the processes of bone tissue formation with areas of structural decomposition;
- excessive physical activity;
- penetration into bone tissue of infectious agents causing tuberculosis, syphilis, osteomyelitis and a number of other serious diseases;
- aseptic bone necrosis;
- purulent forms of arthritis.
Provocative causes of the development of a bone cyst can be other diseases of the musculoskeletal system, as a result of which motor activity is disrupted and muscle fiber tone is reduced. Pathology often accompanies decreased immunity and a deficiency of certain vitamins and minerals in the human diet.
conclusions
Since no single protocol has been developed for the choice of treatment method for children and adolescents with tumors and tumor-like diseases, the course of which was complicated by pathological fractures, each case requires a differentiated approach to treatment and depends on the nature, location of the fracture, as well as the age of the patient and the nosological affiliation of the underlying disease, which must be confirmed morphologically.
Information about authors
For contacts:
Snetkov A.I. — email
Aneurysmal and solitary bone cyst
All bone cysts are divided into solitary and aneurysmal. Each form can manifest itself in eccentric or central localization. Aneurysmal bone cysts most often affect the pelvic bones and bases of the vertebral bodies. It can be diagnosed in girls and boys aged 12–15 years. In adult patients, such cavities can only be diagnosed if they were not treated in childhood.
The main reason for the appearance of an aneurysmal bone cyst is traumatic exposure. The development mechanism is as follows:
- an extensive soft tissue hematoma occurs in the area of injury;
- primary inflammation begins, as a result of which the blood supply to the damaged area increases;
- lysozymes, enzymes, and mast cells are drawn into the focus;
- they start the process of softening and destruction of damaged tissues;
- after cleansing the lesion, the process of filling it with a collagen frame begins;
- subsequently, trabeculae of bone tissue are built into this frame;
- with an excessive amount of lysosomal enzymes and prolonged inflammation, this mechanism is disrupted and a cavity remains in the area of the source of destruction and decay.
It gives pronounced clinical symptoms. At the initial stage, there is pain that interferes with the mobility of the limb. In the area where the cyst develops, swelling and redness of the skin occurs. The venous pattern intensifies. Palpation is sharply painful. When taking an x-ray, a cavity filled with liquid or pneumatized is visible. For differential diagnosis, a puncture is performed to collect the internal contents.
When an aneurysmal bone cyst is located in the spinal column, clinical signs of spinal canal stenosis may occur. Also, this neoplasm can compress the radicular nerves, provoking the appearance of severe radiculitis, numbness of the lower or upper extremities, stiffness and overstrain of the muscular frame of the back. If an aneurysmal bone cyst forms in the spinal canal area, the patient is advised to undergo emergency surgery followed by plastic surgery of the removed portion of the vertebral body.
A solitary bone cyst has a single-chamber structure. It most often occurs in the area of the tubular bones of the upper and lower extremities. It is diagnosed mainly in boys aged 14–16 years. It may be a consequence of osteomyelitis or another inflammatory disease suffered in early childhood.
The initial stage of formation of a solitary bone cyst does not give any clinical symptoms. The first sign of trouble is often a bone fracture in the place where the hidden cavity has formed. During an X-ray examination, the doctor discovers a bone cyst.
In the absence of fractures, lameness, shortening of the limb, increased fatigue of muscle tissue, and pain in the area where the cyst is located may be observed. If such symptoms appear, you should consult a doctor promptly. Treatment of fractures in the area of a solitary bone cyst is long-term, it can take up to 6-9 months. Therefore, it is important to begin treatment in advance, avoiding damage to the integrity of the tubular bone.
results
The results of treatment were monitored over a period of 1 to 9 years. The effectiveness of treatment was assessed taking into account oncological and orthopedic criteria. The effectiveness criteria were the absence of complaints, relapse of the disease, signs of consolidation of the pathological fracture, and function of the operated limb.
All patients underwent safe osteoplastic surgery, only in 1 case no surgical treatment was performed, since repair of the pathological focus was recorded after healing of the fracture against the background of the cyst. The period of immobilization in a plaster cast was 6 weeks. In situations with other patients, surgical treatment was necessary. Considering the absence of displacement or the presence of slight displacement of bone fragments and the nosological affiliation of the underlying disease, fixation with plaster casts in 21 cases was the first stage of treatment. Fixation mainly lasted 1 month from the moment of injury, thereby consolidating the fracture, which ensured the creation of more favorable conditions for surgical treatment. In case of significant displacement, the first stage was trephine biopsy to verify the diagnosis and closed reposition to eliminate gross displacement. After which the affected limb was fixed with a plaster cast or a skeletal traction system was applied. After morphological verification of the diagnosis, patients underwent open reduction of the fracture, removal of pathological tissue, alloplasty and, if necessary, metal osteosynthesis. Patients operated on without metal osteosynthesis were treated with unloading and fixation of the affected limb with a plaster cast for 3 months from the date of surgery. Next, the plaster cast was removed and the development of movements in the joints of the operated limb began. Full weight-bearing was recommended 4 months after surgery. The use of bone osteosynthesis made it possible to abandon the use of external immobilization and begin early activation of the patient, to begin early development of movements in the joints of the operated limb, which in turn helped to reduce the length of hospital treatment and facilitate patient care.
In the presence of a metal fixator, the development of movements in the joints of the affected limb began 1 week after the operation, and full load - after 1 month. In the postoperative period, dynamic observation of all patients who received surgical treatment in the department was carried out. Control radiographs were taken 3, 6, 9 and 12 months after surgery. Consolidation of fractures was observed 2.5–3 months after surgery. The timing of non-organotypic reconstruction of grafts depended on a number of factors: the volume of the post-resection defect, the number, type and type of grafts and nosology of the disease. Autografts were reconstructed most quickly in a period of 8 to 12 months. With the isolated use of Perfoost grafts, the period of reconstruction took on average from 12 to 14 months. In cases of massive alloplasty with extensive bone resections, when superficially demineralized allo-implants were combined with cortical frozen implants, the reconstruction period increased to 18 months.
The timing of removal of metal structures depended on the nosology of the pathological process. In fibrous and osteofibrous dysplasia, taking into account the nature of the disease, metal structures were left in place to prevent the occurrence of deformities and pathological fractures in the long-term postoperative period. In other cases, the metal structures were removed 1.5–2 years after the operation.
The following complications were recorded between 3 and 6 months. In case of bone cysts: in 5 cases - relapse of the underlying disease, in 2 - shortening of the damaged segment, 1 case each - joint contractures and neurological disorders; with fibrous dysplasia: in 1 patient - shortening of the damaged segment; with non-osteogenic fibroma: 2 – joint contractures. In the long-term postoperative period (9–18 months) with fibrous dysplasia, migration of metal structures was noted in 2 cases.
Bone cyst of the knee joint: femur and tibia
A primary bone cyst of the knee joint can form at any age. The cause is trauma, inflammation, ischemia due to vascular pathology or impaired innervation. In adults, due to traumatic and inflammatory effects, a bone cyst of the femur is more often formed, which can manifest itself as local pain and a gradual increase in the volume of the lower thigh.
In children under the age of 15 years, a bone cyst of the tibia predominates - in this case, an increase in volume becomes noticeable in the upper part of the lower leg.
For diagnosis, an x-ray and puncture of the hidden cavity are used. During the diagnostic procedure, it is possible to remove excess fluid and restore normal osmotic pressure. This brings temporary relief to the patient’s condition and reduces the risk of violating the integrity of the thin walls of the bone cyst.
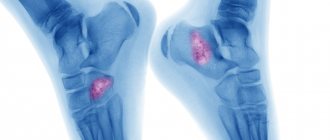
Bone cyst of the calcaneus
In children, a bone cyst of the calcaneus is practically undetectable. In an adult, this pathology may be associated with shock wave therapy to treat plantar fasciitis or heel spurs. Violation of the rules for using this technique can provoke pathological decay of tissue in the thickness of the heel bone. Subsequently, this entails the formation of a cavity filled with lymphatic fluid and serous substrate. In some cases, aseptic necrosis of the calcaneus develops with local multiple cystic cavities.
If, after shock wave therapy, severe pain persists, the skin is hyperemic and swollen, then you should immediately consult an orthopedic doctor.
A comment
The information presented in the article is fundamentally new; The work is well structured, illustrated and argued. In conclusion, we can once again clarify the details of the separate lesion of the cyst of the odontoid bone and the CII body, indicating the features of the embryogenesis of the cyst. These technical details will improve the perception of the article by the magazine's readers.
The article is undoubtedly of practical interest and can be recommended for publication in a specialized neurosurgical journal.
A.Yu. Mushkin
(Saint Petersburg)
Vertebral bone cysts in children
Various forms of bone cysts in children may be caused by congenital anomalies in the development of trabeculae. A vertebral bone cyst in early infancy can appear against the background of hemangioma, during trauma, during the development of rickets, etc.
It is very difficult to suspect the development of such pathologies. If at the age of 10–15 years a child can identify the cause of his anxiety and indicate where and what hurts him, then an infant can express his emotions only by crying. Therefore, it is important to pay attention to changes in the baby’s behavior. If he is capricious and refuses to lie on his back, then it is better to show him to specialists. A late visit to a neurologist with the development of a vertebral bone cyst in the area of the spinal canal can lead to the development of convulsive syndrome in the baby, paralysis of the lower and upper extremities, severe forms of flaccid paresis, etc.
A comment
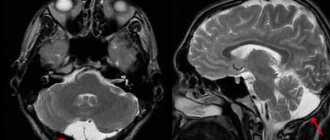
The paper presents in detail two clinical cases of bone cysts in the clivus and axis.
Undoubtedly, the work is of scientific and practical interest, especially since the world literature does not describe such clinical observations of bone cysts localized in the area of the base of the skull and the craniovertebral joint.
These are rare, very interesting, from the point of view of clinicians, cases, which makes them very indicative. In addition, we were shown well-executed operations.
I consider it necessary to publish this work in the journal “Problems of Neurosurgery” as it is novel and contains information useful for colleagues.
A.O. Thickness
(Moscow)
Bone cyst of the humerus in adults
Solitary and aneurysmal bone cysts in adults can form under the influence of negative factors. These could be injuries. But in most cases, a bone cyst of the humerus develops against the background of cervical osteochondrosis and a violation of the innervation of the vascular wall. Emerging areas of ischemia provoke a primary reaction of bone tissue lysis. A serous substrate may remain in the resulting cavity. It provokes a secondary inflammatory reaction.
Bone cysts of the thigh and lower leg in adults rarely form and only against the background of total vascular insufficiency. At the base of the vertebra, a cyst can occur due to excess pressure on the spinal column due to obesity.
Treatment of bone cysts
In most cases, treatment of bone cysts is carried out in a surgical hospital. There a series of intracavitary punctures are made. With their help, excess fluid is removed and increased cavity pressure is relieved. To reduce enzymatic activity, various pharmacological drugs are injected into the cyst. It is important for the doctor to stop the process of bone tissue destruction and start the regeneration of the normal structure.
Manual therapy is required at the rehabilitation stage. It is very important to restore microcirculation of blood and lymphatic fluid in the affected area. For this purpose, methods of osteopathy and massage are used. It is also necessary to restore lost muscle tissue tone. This requires a specially developed course of therapeutic exercises and kinesitherapy.
You can speed up the process of formation of normal bone tissue with the help of reflexology. Physiotherapy methods are also used.
You can schedule a free initial consultation at our manual therapy clinic. The doctor will conduct an examination, review your medical documentation and tell you how and what methods of manual therapy are advisable to use for a quick and complete recovery.
Physical therapy complex
Physical therapy is prescribed to patients who have undergone surgery to remove a Baker's cyst, or as an additional method for conservative treatment.
Exercise therapy classes have several goals:
- strengthen the ligaments of the knee joint;
- stretch the gluteal, thigh, calf and quadriceps muscles;
- stretch your hamstrings.
Specially designed exercises help eliminate fatigue, reduce the tone of tense muscles, and restore blood supply to the limb.
The exercise therapy complex includes the following exercises:
- alternately bending and straightening the legs at the knees while sitting on a chair;
- a similar exercise, but with weights on the ankles;
- chair squats and stand-ups;
- pulling your legs to your chest while sitting on the floor.
For maximum therapeutic effect, it is necessary to perform exercises under the supervision of a specialist – a rehabilitation specialist.
The patient must follow certain rules:
- Warm up your muscles before starting exercise.
- Do not engage in sports training that places intense stress on your knees.
- Do not overwork your leg muscles, perform all exercises measuredly. If muscles become tired, stop training.
- All exercises are performed on a special surface.
All patients with a Baker's cyst in the popliteal fossa are recommended to take long walks (up to 20 km per day), swimming in the pool, and exercise on an exercise bike. You can learn about the exercise therapy complex by following the link.