Frontal hyperostosis is a rare pathology, but sometimes it is dangerous for the patient. Due to its low prevalence, it has not been studied enough, so there are not many serious studies in this area. In ICD-10, the disease is defined as No. M85 along with other disorders of bone density.
The very concept of “hyperostosis” means bone growth of a pathological nature. It is often accompanied by tumor processes and serious hormonal disorders. Hyperostosis also occurs as a consequence of malignant neoplasms.
General information
Hyperostosis is a pathologically increased content of unchanged bone substance (from the Greek hyper - over, osteo - bone), which can be a response to certain intoxications , poisoning , physical overload, exposure to radiation, cancer formation , hypervitaminosis of vitamin A and endocrinopathies, obesity , arterial hypertension , chronic infections, and is also a manifestation of osteomyelitis . It is quite rare and formally resembles spondylosis .
The disease is assigned the ICD-10 code: M48.1 Ankylosing Forestier hyperostosis or diffuse idiopathic skeletal hyperostosis. Hyperostosis can affect the entire musculoskeletal system (generalized), several bones, or just one (local). Forestier's disease is a striking example of local hyperostosis and is a degenerative-dystrophic lesion of the spine in the form of ossification and thickening of the longitudinal ligament along the cervical and thoracic spine. The disease is more common in people 55–60 years of age and older.
Local hyperostosis also includes:
- damage and increase in size of the skull bones, most often the facial bones ( craniosclerosis );
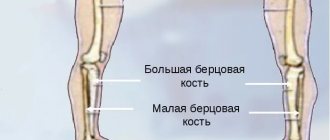
- proliferation of bone tissue that has not undergone pathological changes within the diaphyses in tubular bones;
- Morgagni-Morel-Steward syndrome is characteristic of older women and affects the internal plate of the frontal bone.
What is hyperostosis of the frontal bone?
It is very important to promptly recognize and understand what hyperostosis of the frontal bone is. It usually develops in the setting of virilism , obesity , amenorrhea , or other neuroendocrine and reproductive disorders. However, recent studies have shown that Morgagni syndrome was also identified in men, and it was a hyperostosis of the inner plate of the frontal bone.
In women, the underlying mechanism for the development of pathology is an increase in the concentration of male sex hormones above normal. This manifests itself in the form of a tendency for fat deposition in the abdominal area, a deepening of the voice, increased muscle growth, and the appearance of a beard and mustache. Changes occur gradually, cause pain and discomfort, provoke weight gain, irritability and sleep disturbances, and can even cause depression .
Causes and risk factors
The etiological and pathogenetic mechanisms of frontal hyperostosis have not been fully established. Some researchers talk about the genetic nature of this syndrome. The mechanism of inheritance in this case is autosomal dominant, possibly having a connection with the X chromosome. In clinical practice, many familial cases of the disease are known, for example:
- three children and their mother;
- five women in three generations in a row;
- over four generations, doctors observed 12 such patients (including 10 women).
Among men, Morgagni-Stewart-Morel syndrome is rare and is predominantly random. It is known that it is transmitted only through the female line.
The trigger for the disease may be hidden in infections suffered by a person and other pathologies affecting the head area:
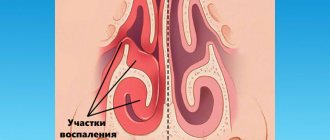
- in sinusitis;
- in neuroinfections;
- in TBI.
An interesting fact is that a number of specialists (in particular, E. Moiseeva and I. Manuilova) observed the development of frontal hyperostosis in two out of three women who underwent surgical castration. It was also found out that the disease can be provoked by long-term use of hormonal therapy after treatment of malignant neoplasms. In women, most often we are talking about breast cancer.
Free consultation on training issues
Our consultants are always ready to tell you about all the details!
In addition, frontal hyperostosis occurs in patients:
- with benign tumors of the uterus;
- with metabolic disorders in the endocrine system;
- with sexual infantilism;
- with menstrual irregularities;
- with syphilis;
- with chemical poisoning.
The exact connection between serious metabolic disorders and tumor processes with the development of frontal hyperostosis has not yet been established, although the frequent presence of pituitary tumors in this pathology constantly leads specialists to think about its obvious involvement in the development of the syndrome. We are talking about both functional and hereditary disorders of the hypothalamic-pituitary system: since the hypothalamus is responsible for connective tissue metabolic processes, a failure in its work can lead to the fact that the structure of protein and carbohydrate complexes in the cranial bones undergoes a number of pathological changes. As a result, bone tissue grows.
There is also a theory of compensation: the disease most often begins to manifest itself in older people. The older a person gets, the smaller his brain, resulting in thickening of the frontal bone.
However, metabolic disorders are also combined with deviations in the sphere of emotions and the autonomic nervous system. This suggests that the level of damage may be higher.
There is another hypothesis: in the presence of an unfavorable environment, patients develop insufficient function of the limbic-reticular formation. This provokes further manifestation of the syndrome.
Pathogenesis
The main manifestation of Forestier hyperostosis is ossification (extraskeletal formation of bone tissue in atypical places) of the anterior longitudinal ligament along the cervical and thoracic spine.
The pathology develops as a result of an autoimmune nonspecific inflammatory process, which leads to diffuse idiopathic changes in the skeleton in the form of replacement of the end structures of the nodes with cartilage and then with bone tissue.
Ligaments of the spinal column
Typically, the ossification process affects the ligamentous apparatus, while bone growths can form in the anterolateral sections - the so-called hyperostotic strata, non-connecting “bridges” and “spurs” of the spine, bypassing the intervertebral discs. As a result, the mobility of the vertebrae suffers, which leads to ankylosis (in some cases to complete immobilization) and, as a consequence, to muscle atrophy.
The disease is characterized by a long course, with no disturbances in the structure of internal organs, joints or the height of the vertebrae.
Treatment of hyperostosis
Currently, conservative treatment methods are mainly used to treat bone hyperostosis. Corticosteroids (hormones) are prescribed, which are designed to suppress bone growth. But in most cases, the effects of manual therapy are sufficient to stop the pathological process and reverse it.
In our manual therapy clinic, the following techniques are used to treat hyperostosis:
- diet therapy – the patient receives comprehensive individual recommendations on how to properly build their diet and diet;
- osteopathy and massage - accelerate metabolic processes, enhance microcirculation of blood and lymphatic fluid in the lesions;
- therapeutic exercises and kinesiotherapy prevent the formation of contractures and maintain full body mobility;
- reflexology restores metabolic processes and triggers the regeneration of damaged tissues;
- physiotherapy allows you to create suitable conditions for the restoration of bone tissue.
In some cases, shock wave therapy, laser treatment and electrical myostimulation are used.
If you need treatment for hyperostosis, we recommend making a free appointment with an osteopath or orthopedist at our manual therapy clinic. During the initial appointment, the doctor will make an accurate diagnosis and talk about the prospects for conservative treatment in your individual case.
Causes
The initiating factors for the development of hyperostosis are considered to be:
- neuroendocrine disorders;
- frequent intoxication;
- age-related changes in connective tissue;
- chronic infectious diseases.
Causes of Forestier's disease
Pain syndrome and ankylosis can be observed in people after 45-50 years of age, and most often such changes were observed in their parents. It is believed that genetic factors are of greatest importance in the development of pathology. Studies have shown that a third of patients had the following antigen: human leucocyte antigen - HLA B27 , the gene of which is responsible for bone formation.
New bone formation - symptoms and treatment
The diagnostic algorithm includes interviewing the patient, detailing complaints and clarifying the medical history. Particular attention should be paid to fever, weight loss, loss of appetite and other general symptoms. The time that has passed since the discovery of a bone tumor, the presence and intensity of its growth are also specified.[8]
During examination, the size of the formation, its structure, localization and skin changes are assessed. The areas of regional lymph nodes are palpated to assess possible changes - enlargement of the lymph nodes, their adhesion to the surrounding tissue and to each other.
A laboratory search begins with a general and biochemical blood test: determination of alkaline phosphatase, phosphate and calcium.[1] These analyzes provide evaluative information.
There are laboratory markers of bone resorption (dissolution) that confirm the predominance of bone breakdown (possibly at the tumor site).[9]
But their diagnostic value, unfortunately, is limited, since bone resorption can also occur in other conditions not associated with a bone tumor.
Instrumental diagnostics
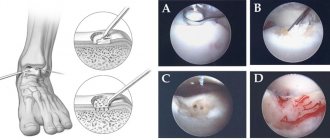
The most accessible, fastest and most revealing instrumental diagnostic method is radiography. An x-ray taken in two projections gives an idea not only of the size and location of the bone tumor, but also of its type.[3]
A more detailed and sensitive visualization of new bone formations is computed tomography.[16] It is especially relevant for joint tumors and small bone tumors that are poorly visible on ordinary X-rays.[8]
Scintigraphy is used as a screening (search evaluation method) - bone scanning after intravenous administration of a radioactive isotope. The isotope accumulates in the bone tumor, causing it to “glow” on the scanner screen. This method provides information about the presence of skeletal tumors and their number. It is also effective for the early detection of bone metastases in cancer patients.[6] However, it is impossible to distinguish a benign tumor from a malignant one, much less determine the type of tumor on a scintiogram.[16]
It is noteworthy that radiation methods for diagnosing neoplasms do not provide the right to reliably diagnose a specific type of bone tumor. Even with all the X-ray signs that speak in favor of a certain tumor, only examination of the tumor under a microscope is decisive.
For microscopy, cells are obtained using a biopsy - taking part of the tumor. For this, a puncture biopsy is used, when the bone is obtained with a wide needle, or an incisional biopsy - surgical removal of the tumor, i.e. cutting off part of it.[16]
Often a biopsy is performed immediately during surgery to obtain a preliminary result. This makes it possible to determine the volume of the operation.[2]
Symptoms
The clinical manifestation of Forestier's disease is only a limitation of the range of motion in the affected part of the spine. In extremely rare cases, patients may experience symptoms such as:
- slight or moderate pain in the thoracic spine;
- smoothing the physiological curves of the spinal column;
- changes in posture in the form of stooping or the development of a pronounced “supplicant pose”;
- dysphagia (more typical for more severe stages of significant ossification of the structures of the cervical spine);
- amyotrophy;
- with ossification of other ligaments, pain may occur in the places of their attachment, including the area of the calcaneus, the process of the ulna, the hip joint, the ischial tubercle, and the patellas.
The disease is much more severe with ossification of the posterior longitudinal ligament (“posterior” Forestier). Its thickening leads to progressive spinal stenosis, compression of the spinal cord, myelopathy and severe neurological disorders.
Tests and diagnostics
Despite the level of development of modern medicine, it is quite difficult to recognize hyperostosis after studying the clinical picture. X-ray examination becomes the most revealing, and tomography is used to accurately determine the localization of the pathological process within the bone structure. In some cases, additional radionuclide testing may be required.
Cervical spine with Forestier hyperostosis
Forestier's disease on an x-ray is characterized by the presence of thickening of the anterior longitudinal ligament and its fusion with the ventral surfaces of the vertebral bodies, but the height of the intervertebral spaces is not reduced. Laboratory values sometimes reveal hyperglycemia .
When making a differential diagnosis with other pathologies that deform the spine, take into account the absence of laboratory signs, manifestations of inflammatory activity, sacroiliitis , ankylosis of intervertebral joints , and narrowing of intervertebral discs.
Hyperostosis - general information
Hyperostosis (from the Greek hyper - over, osis - bone) is excessive bone growth, which is determined by an increase in bone tissue mass per unit volume. It can occur compensatoryly (with increased load on the limb) or be a symptom of a number of diseases. Hyperostosis itself does not pose a danger to the patient, but it can signal pathological processes that require serious therapy. Depending on the underlying disease in which hyperostosis is observed, this pathology can be treated by oncologists, phthisiatricians, endocrinologists, pulmonologists, gastroenterologists, venereologists, orthopedists, rheumatologists and other specialists.
Diet for Forestier hyperostosis
Hypocaloric diet
- Efficiency: 3-6 kg in 30 days
- Terms: 14-30 days
- Cost of products: 1500-1600 rubles. in Week
The fundamental factor in improving the condition of patients with hyperostosis is weight normalization, which can be achieved through a lifelong diet. Most often, a hypocaloric diet is prescribed, which can reduce the number of calories consumed, but at the same time provide the body with all the necessary substances and vitamins. It is recommended to add more to your diet:
- fresh vegetable and fruit salads;
- light soups;
- flour products made from whole grain or wholemeal flour;
- porridge;
- seafood;
- teas and compotes.
It is advisable to completely eliminate alcohol, flour, sweets, fried and fatty foods, as well as harmful foods such as smoked meats, canned food, semi-finished products, fast food, etc.
Types of hyperostosis
Marie-Bamberger syndrome
Marie-Bamberger syndrome (systemic ossifying periostosis, hypertrophic osteoarthropathy) is excessive growth of bone tissue, described by the Austrian physician Bamberger and the French neurologist Marie. It manifests itself as multiple, usually symmetrical, hyperostoses that occur in the area of the forearms, legs, metatarsals and metacarpals. Accompanied by a characteristic deformation of the fingers: the phalanges thicken in the form of “drumsticks”, the nails take on the appearance of “watch glasses”. A patient with hyperostosis experiences pain in the bones and joints. Autonomic disorders (redness and pallor of the skin, sweating) and recurrent arthritis of the metacarpophalangeal, elbow, ankle, wrist and knee joints with a blurred clinical picture are also observed. Possible enlargement of the nose and thickening of the skin on the forehead.
Hyperostosis in Marie-Bemberger syndrome develops secondarily, as a reaction of bone tissue to an imbalance of acid-base balance and chronic lack of oxygen. The cause of the syndrome is malignant tumors of the lungs and pleura, chronic inflammatory diseases of the lungs (pneumoconiosis, tuberculosis, chronic pneumonia, chronic obstructive bronchitis, etc.), intestinal and kidney diseases, as well as congenital heart defects. Less commonly observed in liver cirrhosis, lymphogranulomatosis and echinococcosis. In some cases, hyperostosis occurs spontaneously, without connection with any disease.
X-rays of the legs, forearms and other affected segments reveal a symmetrical thickening of the diaphysis due to the formation of smooth, even periosteal layers. At the initial stages, the density of the layers is less than that of the cortical layer. Subsequently, the layers become more dense and merge with the cortical layer. With successful treatment of the underlying disease, the manifestations of Marie-Bemberger syndrome decrease and may even disappear completely. To reduce pain during exacerbation, NSAIDs are used.
Frontal hyperostosis
Women of menopausal and post-menopausal age suffer from frontal hyperostosis. Hyperostosis is manifested by thickening of the inner plate of the frontal bone, obesity and the appearance of male sexual characteristics. The cause of its occurrence is not clear; it is assumed that hyperostosis is provoked by hormonal changes during menopause. The disease develops gradually. Initially, patients are bothered by persistent, squeezing headaches. The pain is localized in the forehead or back of the head and does not depend on changes in head position. Due to constant pain, patients with hyperostosis often become irritable and suffer from insomnia.
Subsequently, body weight increases and obesity occurs, often accompanied by increased hair growth on the face and in the torso area. Other manifestations of frontal hyperostosis include type II diabetes mellitus, fluctuations in blood pressure with a tendency to increase, palpitations, shortness of breath and menstrual irregularities, which, unlike normal menopause, are not accompanied by hot flashes. Over time, there is a worsening of nervous disorders, and depression is sometimes observed.
The diagnosis of frontal hyperostosis is made on the basis of characteristic symptoms and X-ray data of the skull. Radiographs reveal bone growths in the area of the frontal bone and sella turcica. The inner plate of the frontal bone is thickened. X-rays of the spine often reveal bone growths. When studying the level of hormones in the blood of patients with hyperostosis, an increased amount of adrenal hormones, adrenocorticotropin and somatostatin is determined.
Treatment of frontal hyperostosis is carried out by endocrinologists. A low-calorie diet is prescribed, and patients are advised to maintain sufficient physical activity. For persistent increases in blood pressure, antihypertensive drugs are indicated; for diabetes mellitus, drugs to correct blood sugar levels are indicated.
Infantile cortical hyperostosis
This hyperostosis was first described by Roske in 1930, however, a more detailed description of the disease was performed by Silverman and Caffey in 1945. The reasons for the development are not exactly clear; there are theories regarding hereditary and viral origin, as well as the connection of the disease with hormonal imbalances. Hyperostosis occurs only in infants. The onset resembles an acute infectious disease: a rise in temperature occurs, the child loses appetite, and becomes restless. Accelerated ESR and leukocytosis are detected in the blood. On the face and limbs of patients with hyperostosis, dense swellings appear without signs of inflammation, sharply painful on palpation. A characteristic sign of infantile hyperostosis is a “moon-shaped face” caused by swelling in the lower jaw.
According to radiography of the clavicles, short and long tubular bones, as well as the lower jaw, lamellar periosteal layers are revealed. The spongy substance is sclerosed, compact and thickened. Based on the results of radiography of the lower leg, an arched curvature of the tibia can be determined. General restorative therapy is prescribed. The prognosis for infantile cortical hyperostosis is favorable, all symptoms disappear spontaneously within several months.
Cortical generalized hyperostosis
Hyperostosis is hereditary; inheritance occurs in an autosomal recessive manner. It manifests itself as damage to the facial nerve, exophthalmos, deterioration of vision and hearing, thickening of the collarbones and enlargement of the chin. Symptoms begin after adolescence. Radiographs reveal cortical hyperostoses and osteophytes.