- July 31, 2019
- Orthopedics and traumatology
- Bondar Fedor
How to determine a fracture or bruise of the foot? Their symptoms are similar. These are also the most common injuries in medicine that occur to people of any age. These injuries can have a wide variety of causes, which arise not only in everyday life, but also during very intense sports, received at work or in major accidents.
To eliminate unpleasant consequences, each person must accurately diagnose these injuries and distinguish between a foot bruise and a possible fracture, since in certain cases a fracture of the foot bones can be confused with a severe bruise, and vice versa.
It is very important to understand that the selection of the optimal method of providing emergency medical care to the victim, as well as the effectiveness of treating the injury, will entirely depend on the accurate diagnosis, since these methods can vary significantly.
So how to distinguish between a fracture and a bruise of the foot (ICD-10 code for the latter is S90.3)? Read more about it.
General symptoms
You should know how to distinguish between a foot bruise and a fracture. After all, the symptoms are similar. The main signs of foot injury are pronounced cyanosis and hematoma, which, however, after a few days can “spread” quite far and high from the site of injury. The patient may also experience swelling and, of course, severe pain.
If a bruise occurs, movement of the foot may be limited for some time. It is noteworthy that this condition can provoke swelling of the tissues surrounding the foot, rather than damage to the foot from the inside. If the integrity of the bones of the foot is compromised, it practically stops moving - any change in position will cause pain, which can also spread to other parts of the body as a result of nerve innervation.
Even without walking, the pain in the foot persists - excessively swollen surfaces, as well as displaced bone fragments, press on the soft tissues from the inside. A reflexive contraction of the muscles occurs, they try to move into the desired position, but this causes pain to increase again.
A characteristic symptom of an existing fracture is considered to be a very pronounced hematoma - due to a violation of the integrity of the bones, damage to all vessels occurs, and internal hemorrhage may occur. With certain types of foot fractures, the hematoma will appear only 1-2 days after the injury, since the bone is surrounded by a dense layer of muscle.
Visually it is easier to identify a foot fracture in a person: the leg may look unnatural, it can be bent in places without joints. When feeling the fracture site, the doctor can feel the bone fragments and even hear a characteristic crunch.
All open wounds, if any, must be carefully treated to reduce the risk of infection. If a person does not have a tetanus vaccination, it is imperative to carry out emergency prevention - treat the wounds with special antiseptic compounds, and also administer tetanus toxoid.
Osteochondral transplantation.
For osteochondral transplantation, cartilage tissue from the ipsilateral knee joint is most often used. Indications for transplantation are large and deep defects, often with the formation of a cyst, as well as the lack of effect from the surgical treatment methods proposed above. The possibility of using the calcaneal bone site at the Achilles-calcaneal joint as a source of tissue for osteochondral transplantation is currently being studied, with good early results.
The objective of the method is to restore the structural and biomechanical characteristics of damaged hyaline cartilage. This method is characterized by a long and difficult rehabilitation period. Morbidity of the donor site (pain in the knee joint after removal of columns of osteochondral blocks) is observed in 12% of cases. The technique itself is technically complex and time-consuming.
In clinical studies, the effectiveness of the method was estimated from 74 to 100% (average 87%).
Foot bruise
A foot bruise, ICD-10 code S90.3, is an uncomplicated injury to the muscles, subcutaneous tissue, and skin, without compromised integrity. The main symptom of a bruise is severe pain in the leg area, which occurs almost immediately.
Blueness of the skin may also appear after an injury or after some time has passed. The result of a bruise may be a small hematoma or swelling. After a few hours the pain becomes more pronounced, it becomes sharper and sharper, after which it can become dull and aching.
If the risk of fracture is completely eliminated, the pain subsides after a few days. But it is important to remember that if the pain increases, you should urgently consult a doctor. In the first day after a bruise in the foot area, the swelling may increase slightly.
Removal, curettage and bone marrow stimulation.
After debridement, several channels are produced that communicate the defect with the bone marrow. This procedure can be performed using reaming or microfracturing. The purpose of the manipulation is to destroy the barrier of sclerotic subchondral bone that prevents the migration of stem cells from the bone marrow. As a result, a clot is formed, saturated with growth factors and stem cells, which is subsequently rebuilt into hyaline-like cartilage tissue. Most often used for stages 3-4 of the disease. The size of the defect should not exceed 1.5 cm. In clinical studies, the effectiveness of the method was estimated from 46 to 100% (on average 85%).
The appearance of a hematoma
A hematoma is a consequence of hemorrhage in the soft tissues of the foot. Its size and shade will be primarily influenced by the force with which the blow was struck. When the subcutaneous fatty tissue is affected, the bruise usually appears immediately 1-3 days after the injury. If the damage is very deep, the hematoma may not manifest itself at all.
Doctors also note that the hematoma will gradually change its shade: a fresh one has a bright red tint, but a little later it may acquire a purple color. On days 4-5, the hematoma has a dark blue color, and after that it becomes slightly yellowish.
Surgical treatment of osteochondral injuries of the talus.
Surgical treatment of OPTC depends on many factors: patient characteristics such as age, activity level, comorbidities, characteristics of the lesion itself such as its location, size, depth of the lesion, lesion morphology, duration. Basically, surgical treatment is based on one of three principles: 1) removal of the loose body with or without bone marrow stimulation through microfracture, reaming 2) preservation of cartilage through retrograde reaming, fixation of the fragment or replacement of the defect with cancellous bone 3) stimulation of the formation of new hyaline cartilage by due to osteochondral block transplantation, mosaic chondroplasty, allograft.
Localization
Typically, a foot bruise (swelling is its first symptom) varies in a specific area. For example, in most cases the toe area is affected, while the heels and soles are much less likely to be affected. This especially happens if the patient does not have displacement of impacted, subperiosteal and incomplete bone fragments.
The main difficulty in diagnosing a bruise is that the signs described above may indicate a closed fracture without detected displacement. In such a situation, it is impossible to establish a reliable diagnosis without tomography or fluoroscopy.
If edema begins to develop, this is most likely due to excessive accumulation of fluid in the tissues of the limb and their deformation. Typically, swelling subsides after a few days, as well as after removing a previously applied pressure bandage.
It is worth learning more about how to distinguish a bruise from a broken leg.
Rehabilitation after surgery for osteochondral injuries of the talus.
Most authors adhere to the standard rehabilitation protocol, which recommends 6 weeks of immobilization after surgery using bone marrow stimulation. However, recently, work has appeared indicating that a 2-week period of immobilization is more than enough for small and medium-sized defects. Rehabilitation consists of training active and passive range of motion, muscle strength and muscle balance of the lower leg, reducing swelling and proprioceptive training.
Pain, a sensation of wedging, and swelling often persist for up to 1 year after surgery. After 6 months, it is advisable to perform an MRI control to assess the dynamics; in the presence of severe bone marrow edema, the prognosis is unfavorable. In such cases, progression of the lesion may further lead to the need for arthrodesis or ankle replacement.
Signs
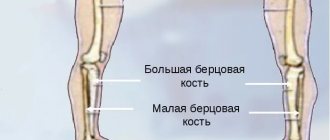
Signs indicating a bone fracture in the foot may differ, depending on the affected part:
- If the heel is damaged, the main symptom will be the appearance of swelling and hematomas that appear a little later, located below the level of the ankle. The swelling quickly grows, the outlines of the heel become blurred, and when you touch it, the person experiences pain and practically cannot walk.
- If there are fragments that have shifted, the pain can also spread to the calf area. If a compression fracture occurs, the arch of the foot may swell, and it may become significantly larger than the other foot.
- If the fracture occurs in the talus, the patient may experience pain and increased swelling. These signs will intensify upon palpation. Bleeding into the joint may also occur. It becomes difficult to move the leg, and the contours of the joint are usually disturbed. It is difficult to diagnose a fracture of the talus using these symptoms alone, and it can be differentiated as much as possible by spraining the ligaments in the foot. To establish the correct diagnosis, you need to monitor the presence of two characteristic symptoms: the localization of swelling from the inside of the leg, which reaches almost to the middle part of the ankle joint, and the second symptom - increased hemorrhage.
- When a fracture occurs in the neck of the bone, a lump may form, the skin becomes blue and becomes very stretched, and discomfort is localized in the front. When the posterior process is injured, pain occurs mainly in the heel.
- When there is a fracture in the metatarsal bone of the foot, the main symptom is swelling located near the sole. Sometimes it spreads to the outside of the injured leg. In most cases, the metatarsal bone of the foot is deformed, and when trying to walk even a little, the patient experiences pain.
- If the phalanges of the fingers are damaged, the victim exhibits signs characteristic of simple fractures. Moving your fingers on a limb is quite painful; you can stand on your foot, but the person feels significant discomfort and notices swelling. Often, a hematoma on the nails is added to a fracture of the phalanges on the feet.
If there is a fracture, even after several hours the pain will not subside, becoming more pronounced and severe. If the patient was diagnosed with an impacted fracture, without involvement of soft tissues, hematomas will not be detected.
When fragments of the bones of the foot are displaced, it will be much easier to recognize the fracture: the foot can be deformed, shortened or lengthened compared to the uninjured leg.
Pathophysiology of osteochondral injuries of the talus.
Anterior-external OPTCs are a consequence of inversion and dorsiflexion of the foot, they are characterized by a large area and are rarely deep. This is most likely due to the longitudinal direction of the injury force vector.
OPTK along the posterior-medial surface, on the contrary, are more often deep, cup-shaped, or accompanied by the formation of a cyst with a cap of cartilage on top. Apparently this is due to the vertical concentrated direction of the trauma force vector.
Thus, it becomes clear that osteochondral injuries of the talus are often combined with instability of the ankle joint, damage to the ligamentous apparatus of the ankle joint, and ankle fractures.
Anatomical studies have shown that the cartilage of the talus is 18-35% softer than the cartilage of the corresponding areas of the tibia. The thickness of the cartilage is inversely proportional to the load it experiences, which can also affect the location of the damage zone.
As studies have shown, the distribution of load in the ankle joint is disrupted when the defect size is more than 7.5\15 mm, which can be used to predict delayed results.
"Stuck heel"
In an adult, the symptom of a broken foot may appear as a “stuck heel”: it is difficult for a person to tear the leg off independently from a lying position. The crunching of fragments may even be felt when palpated. Also, this condition is observed in the absence of a process of pinching of the muscles located between the fragments.
If a patient has a closed foot fracture, doctors may note pathological mobility of the foot outside the joint. It is extremely undesirable to independently check the possibility of mobility of the victim’s foot, since this can further damage the blood vessels and nerve endings, as well as displace fragments.
Complications of toe injuries
Broken toes can lead to dangerous health consequences even when the injury is relatively mild. Without qualified medical care, skin wounds, cracks and bone fractures can provoke the development of the following complications:
- massive hematomas;
- ankylosis (joint immobility);
- deformation of finger joints;
- formation of bone callus;
- sepsis;
- secondary infections.
Damage to the soft and hard tissues of the extremities is especially dangerous for patients who suffer from metabolic disorders and chronic diseases, in particular diabetes. For such patients, even a minor injury can pose a hidden threat.
Open fracture
Another option for distinguishing between a foot bruise and an open fracture is below. An open fracture with a violation of the integrity of the skin in the foot is easy to identify, and anyone can do this simply by feeling the foot. In an open wound, bones may be visible, swelling may increase, and the foot may bleed.
There are times when pain from a fracture in the foot may not be felt at all. This is especially true when there is excessive production of adrenaline. Swelling can appear almost instantly or grow over time. The length of time a hematoma lasts will also be influenced by the amount of muscle tissue available surrounding the injury.
Classification of osteochondral injuries of the talus.
Radiological classification of osteochondral lesions of the talus by Berndt and Harty
CT classification of osteochondral lesions of the talus Ferkel and Sgaglione
MRI classification of osteochondral lesions of the talus Hepple.
How to distinguish between a foot bruise and a fracture?
Only an experienced doctor will be able to identify the existing nature of the damage, if necessary, using additional diagnostic methods: for example, computed tomography and radiography. Therefore, if there is minimal suspicion of a fracture, it is not recommended to load or move the bruised foot in any way.
If you bruise your foot, you need to apply a bandage or splint to secure the injured foot. In order to promote contraction of blood vessels, cold should be applied to the bruise and pain medication should be taken.
In case of an open fracture, you need to apply a sterile bandage to the foot. If the case is particularly severe, the doctor may prescribe heat application to the foot. You should also quickly go to the hospital, where the doctor will perform the necessary tests and prescribe the correct treatment, depending on what happened to the foot: a bruise or a fracture.
Retrograde reaming.
This method will require the use of x-ray control and knowledge of the exact topography of the defect location. Retrograde reaming is the method of choice in the presence of a large subchondral cyst and with intact articular cartilage, as well as in cases of deep defect location, when it is difficult to reach it using the arthroscopic method. For medial defects, the entry point of the wire becomes the tarsal sinus. In clinical studies, the effectiveness of the method was estimated from 81 to 100% (average 88%).