The brain is a complex structure, the condition of which determines the normal functioning of motor, speech and other functions. Traumatic brain injuries (TBI) pose the greatest danger, as they can lead to disability.
Since their consequences are often delayed, and externally the symptoms of mild concussions and bruises may appear mild, such injuries require a serious and careful approach.
To avoid post-traumatic complications, it is extremely important to provide assistance to the injured person within the first hour after receiving a traumatic brain injury. Let's look at the types of head injuries and what needs to be done in each individual situation in more detail.
Brain concussion
Bruise and concussion
Statistically, concussion is considered the most common head injury. It is a mild form, so victims often ignore contacting neurologists.
This condition is characterized by the following symptoms:
- amnesia (memory loss) for events that occurred before the injury;
- short-term loss of consciousness is possible (up to 15 minutes);
- nausea, vomiting;
- headache;
- increased sweating, feeling of heat;
- temporary deafness (tinnitus);
- dizziness.
The main sign of a concussion is the absence of damage to the bone tissue of the skull. It takes about 10 days for complete recovery. If the victim was or is unconscious, examination by a doctor is mandatory.
On this topic ▼
Cervical spine injuries
Before medical assistance arrives, you should adhere to the following rules for providing assistance:
- The victim who is unconscious should be placed on his side. The surface must be hard and level. Legs and arms are bent. It is recommended to turn your head towards the floor. This position provides the necessary flow of oxygen and is also safe in case of vomiting.
- If the skin is damaged or bleeding, apply a clean bandage.
- in the case when the victim is in clear consciousness, lay him down with his head slightly raised. Remove the constricting elements of clothing (tie, belt), unbutton the top buttons on the shirt. Keep him awake until the doctor arrives or for an hour after the injury.
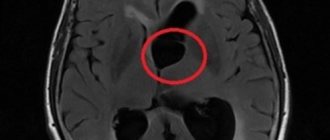
You should know that the distinguishing feature of a concussion from other head injuries is the absence of internal pathological changes. If the examination revealed even minor damage to brain structures, then we need to talk about a more serious type of TBI – brain contusion.
Types and symptoms of brain contusion
With this form, damage to the brain substance occurs at the site of the impact, and foci of destructive changes may also be detected in neighboring areas. This injury is often accompanied by hemorrhage, which can lead to coma and death.
Depending on the damage and external manifestations, brain contusion has 3 degrees of severity:
- A mild degree is accompanied by loss of consciousness for up to 1 hour. Moderate headache, dizziness. Vomiting can be repeated up to 2-3 times. There are fluctuations in blood pressure. When superficial vessels rupture, subarachnoid hemorrhage is possible.
- With a moderate injury, a person can remain unconscious for up to 6 hours. Amnesia is definitely present. The victim may not remember past events or recognize his relatives. Frequent and repeated vomiting with severe headache. There is an increase in blood pressure to 180/100 mm Hg. Art. Possible disorders of the cardiovascular system. Also, such an injury can lead to speech impairment, paralysis, and muscle weakness.
- Severe brain contusion is often accompanied by a coma from a couple of days to several months. Disturbances arise from motor and speech functions. Memory and attention are greatly reduced, inhibition or, conversely, motor agitation appears. Full recovery from such an injury is possible only in childhood, since compensatory mechanisms are better developed in children.
A brain contusion, regardless of severity, should not be left without examination and examination by an appropriate specialist. There are often cases when the consequences overtake victims years after the injury, for example, in the form of a stroke. However, this only occurs when appropriate treatment has not been carried out.
Maybe
Signs of head injuries
All types of head injuries have their own symptoms and mechanisms, knowledge of which will allow you to provide competent assistance to the victim at the scene of the incident. A bruise occurs when struck by a hard object. It can manifest as subcutaneous limited or diffuse hemorrhage, characterized by the presence of fluctuation (softening).
Head wounds can be penetrating (in which the dura mater is damaged) and non-penetrating (without damaging it). Depending on the wounding object, they are divided into cut, chopped, stabbed, bruised, and gunshot wounds.
Cut wounds are inflicted with a knife, blade and other sharp objects. They are accompanied by pain, heavy bleeding; their edges are even, smooth, and gape widely. Chopped wounds occur when struck by a sharp heavy weapon, deep; As a rule, the substance of the brain is damaged. Puncture wounds have a deep channel and are dangerous for the development of anaerobic infection. Bruised wounds are less dangerous, however, they are accompanied by severe damage to surrounding tissues with their further necrosis. Scalped wounds are characterized by damage to surrounding tissue and heavy bleeding. Gunshot wounds are superficial (without damage to the bone) and deep (non-penetrating and penetrating - with damage to the bone, meninges and brain substance).
Fractures of the facial bones reach 4% of skeletal fractures, but the most common are fractures of the lower jaw. With such a fracture, the following signs are determined:
- the patient has difficulty chewing and swallowing;
- the jaw is tilted to the side,
- speech is impaired,
- pain and pathological mobility of fragments are noted.
A calvarial fracture occurs after strong impacts with depression and rupture of the skull bones. It is characterized by:
- the presence of deformation, depression or protrusions,
- mobility of bone fragments and crepitus (a sound reminiscent of that heard when walking on snow in cold weather).
- with an open fracture, brain matter can be seen in the wound.
Fracture of the base of the skull appears:
- leakage of blood and cerebrospinal fluid (cerebrospinal fluid) from the nose and ear,
- symptom of “spectacles” - hemorrhage into the tissue around both eyes,
- exophthalmos (displacement of the eyeball forward).
It must be remembered that the severity of the victim’s condition will be determined not by a bone fracture, but by a traumatic brain injury.
Fracture of the base of the skull
Fracture of the base of the skull
This type of TBI is a rare occurrence. Most often it occurs as a result of a car accident that occurs due to a violation of the speed limit. Sometimes falls from a height, as well as fights, lead to a fracture of the base of the skull.
On this topic ▼
Skeletal injuries: types and characteristics
A fracture of the base of the cranial vault has very noticeable external manifestations:
- "Raccoon eyes" or glasses syndrome. Dark circles and swelling occur around the eyes due to hemorrhage in the periocular tissue. Possible decrease in visual acuity.
- Battle's sign is a hematoma or bruise in the temporal lobe (above the mastoid process). It is this that is the “beacon” sign of a fracture.
- Liquororrhea. If the membranes of the brain are damaged, fluid may leak into the nasal cavity or ear canal.
- Hearing and vision impairments.
- The muscles of the tongue, palate, or larynx may become weakened.
Such a traumatic brain injury is characterized by periods of false well-being. The victim may come to his senses and be adequate, but after a while fall into a coma.
Causes of head injuries
Head injuries occur as a result of such events:
- • injuries in everyday life, fights;
- • injuries at work;
- • use of firearms;
- • injuries during an accident.
Classification of head injuries
The following types of head injuries are distinguished:
- injury to the skin, subcutaneous tissue, muscles,
- fractures of the skull bones.
All injuries can be closed (bruise) or open (wounds). There are also fractures of the skull (vault and base) and facial skull (the most common are fractures of the upper and lower jaw, the temporal bone).
Principles of providing first aid for severe TBI
When providing assistance to a victim with a traumatic brain injury, you must adhere to the following rules:
- put the person on a horizontal surface and ensure peace;
- the head and cervical region should be fixed. A homemade roller made from clothing or any dressing material is suitable for this. This point is especially important if it is necessary to move the victim.
- to prevent swelling, apply cold (ice, snow, a bottle of water) to the injury site;
- Cover the open wound with clean material. If there is a foreign object in the wound, do not try to pull it out under any circumstances. Cover it with tampons on all sides and bandage it using the crosswise technique.
- if you notice blood from the ear, nose or mouth, cover with a sterile bandage and turn the person to the side where the liquid is flowing;
- monitor the victim’s condition: check pulse, breathing;
- transportation is carried out only in cases of emergency. Definitely with neck and head fixation.
- in the presence of vomiting and any brain damage, pain relief cannot be administered until the ambulance arrives;
- if breathing stops, begin resuscitation measures (indirect cardiac massage and artificial respiration).
Thus , before the medical team arrives, you must provide the victim with rest, apply cold, immobilize the head and neck, and monitor the general condition. It is prohibited to give medications to the victim. Given the seriousness of traumatic brain injuries, hospitalization or evaluation by an appropriate specialist is necessary to prevent unwanted health problems.
What should we do before medical help arrives in the event of a traumatic brain injury?
Make sure the victim has the two most important vital signs - pulse and breathing. Then it is important to check your memory and orientation. This is done by asking simple open-ended or guiding questions - “what is your name”, “what day is it”, “what happened”, etc. If the patient is not in contact, an initial vital signs check is performed.
The test should be carried out in order of importance of vital signs. When the heart stops, a person dies within a couple of minutes. Stopping breathing makes it possible to return to life in 5-10 minutes. In this sequence, inspection and assistance are carried out. In medicine, a triple Safar maneuver is recommended: throw back your head, place a cushion under your neck, push out your lower jaw and open your mouth slightly. These techniques ensure tracheal patency. If the chin is pressed to the chest, the trachea becomes kinked.
Gently press the depression on the side of your neck to check for carotid pulsation. You can also apply pressure to your wrist to check your peripheral arterial heart rate. When blood circulation stops, the skin and especially the mucous membranes turn blue very quickly, this is noticeable even to an inexperienced person. If a person cannot determine the pulse, but a change in skin color is visible, it should be assumed that the heart is not working.
Indirect massage in the absence of heartbeat
- Determine the presence or absence of a pulse by pressing on the carotid artery on the front side of the neck.
- If there is no pulsation, begin rhythmic external pressure on the heart area at a frequency of 90-100 pressures per minute. Place both hands on your chest and use your body weight. Pressing is performed with palms one on top of the other on the middle of the sternum between the nipples. With each press, the chest should bend 3-5 cm.
- The heart has valves. When the chest is compressed, a fresh portion of blood is sucked into its cavity and, thanks to the valves, the blood is pushed further into the circulation. This will ensure blood supply to the brain, the organ most sensitive to hypoxia.
Lack of breathing due to head injury
- If there is a heart rhythm, breathing should be checked immediately. This is done by placing the ear to the victim's mouth. You should not trust the movement of the chest. This does not always mean that there is normal breathing - there may be convulsions or attempts to inhale. If vital signs of free breathing are absent, immediate respiratory and cardiac resuscitation should be initiated. This is done until an emergency medical team arrives. Place the person horizontally, tilt their head back slightly, placing a cushion under their neck. If there is no breathing, check your mouth and clear the airway if necessary.
- As much as possible, do not twist your head - expect a fracture of the cervical vertebrae. The person must lie on a flat, hard surface.
- Inspect the oral cavity, if there are foreign objects or broken teeth, remove dentures with a finger wrapped in gauze or a clean cloth.
- If the jaw is broken during a frontal impact and the soft tissue of the mouth and tongue are blocking the windpipe, still clear the airway. To do this, wrap your fingers in dry gauze and tightly grasp your tongue, pulling it out. At the same time, turn the person on his side or stomach so that the tongue does not go back under its own weight. In case of a frontal impact, damage to the jaws is accompanied by knocking out teeth and bleeding. It is this blood, together with saliva and fragments of teeth and bones, that blocks breathing. If bleeding in the mouth continues, the person should be placed face down, placing a cushion of clothing under the chest and forehead so that the blood can flow freely from the mouth to the outside rather than filling the bronchi.
- If breathing does not return, begin artificial respiration from mouth to mouth at a frequency of 3 to 5 times per minute between chest compressions (about 100 compressions per minute). For 30 compressions, perform 2 air injections into the lungs. With artificial ventilation, gas exchange in the lungs occurs at a sufficient level to prevent the death of the brain and other organs; with vigorous artificial ventilation and chest compressions, life can be maintained for up to several hours. When the inflation is done correctly, the chest rises.
After a head injury and in the absence of breathing and heartbeat
When there are two rescuers, one kneels at the victim’s head and performs artificial respiration using the mouth-to-mouth method or using an artificial breathing device at a frequency of 3 to 5 times per minute (20-30 heartbeats - 2 inhalations). The second rescuer applies rhythmic external pressure to the heart, stopping every thirty pressures to force air into the lungs.
When the rescuer is alone, perform the same actions in the following sequence: every 20-30 sternum squeezes alternate with two consecutive mouth-to-mouth breaths into the lungs.
We emphasize once again that these must be energetic, powerful movements. In this case, the blood is enriched with oxygen and circulates from external influences, but this is enough to maintain human life for several hours. With a head injury, the main consequence that must be avoided is the death of the victim. This is exactly what assistance should be aimed at in the first minutes.