General information
Stridor is called hissing or whistling, that is, noisy breathing, which is caused by turbulent air flows in the trachea or larynx, that is, passing through the respiratory tract with narrowed areas or, in more rare cases, in the presence of foreign objects, tumors, outgrowths that can be caused by infectious agents.
It is more often recorded in young children due to laryngomalacia - delayed formation of laryngeal cartilage. Stridor is a symptom of respiratory obstruction. Pathological conditions manifested by stridor are usually life-threatening and require immediate medical attention, as there is a possibility of developing complete obstruction, respiratory failure and pulmonary edema .
1.General information
Stridorous is called heavy, labored, noisy breathing with a hissing and/or whistling sound; Many other acoustic effects are also possible (gurgling, gurgling, wheezing, etc.), which even for a non-specialist can instantly distinguish pathological breathing from normal breathing. The fundamental, physical cause of stridor (stridor breathing) is a change in the nature of the air flow in the respiratory tract: from laminar (uniform, smooth) it becomes turbulent, i.e. vortex. Obviously, given the anatomical complexity of the human airway, stridor can be caused by many specific factors - unfavorable, abnormal or pathological.
Strictly speaking, wheezing at birth is not a disease in itself. However, in such cases, consultation with a pediatric otolaryngologist and other specialists is mandatory, since abnormal breathing may be based on one or another obstruction (blocking the lumen) of the airways, or structural features of the latter. The International Classification of Diseases (heading “Congenital anomalies [malformations] of the respiratory system) provides the diagnosis “Congenital stridor of the larynx.” This condition occurs in the general population with a frequency of over 4%; If we consider all cases of stridor breathing in newborns, then the share of congenital stridor of the larynx accounts for more than 40% (according to other sources, up to 60-70%). Almost always (98%) congenital stridor is accompanied by chronic hypoxia, i.e. oxygen starvation - which explains the need for diagnosis and, at a minimum, observation by a specialist - however, in most children, hypoxia is compensated, transient and, thus, does not require intervention.
A must read! Help with treatment and hospitalization!
Pathogenesis
The pathogenesis of stridor is usually based on significant obstruction of the larynx or trachea, caused by edematous-inflammatory processes, the entry of foreign bodies into the lumen (usually food or bolus), the development of a tumor or other pathological condition. This changes the difference between intrathoracic and atmospheric flow and creates turbulent air currents.
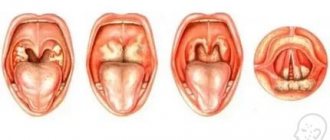
Structure of the oropharynx
Congenital stridor in newborns caused by laryngomalacia occurs when the epiglottis folds into a tube and the development of laryngeal cartilages is delayed, their excessive softness and pliability. The position of the aryepiglottic ligaments is close to each other with the formation of some loose sails, which creates noise - most often during inhalation due to vibrations.
Stridorous breathing is characterized by high resistance to normal breathing, loss of uniform flow and flow of air (the so-called laminarity). As a result, characteristic sounds and vibrations arise, the mucous membranes dry out at the site of narrowing of the airway lumen and sputum crusts form.
Classification
Stridor may differ in pitch, volume, and in what phase of breathing it occurs. Inspiratory - occurs on inspiration, expiratory - on exhalation, and can also be biphasic.
A separate type is the extrathoracic type of stridor in children with a weak chest frame (not able to protect against collapse) and too pliable airways, which narrow due to the difference between atmospheric pressure and low air pressure in the airways immediately behind the narrowing.
Causes
In 87% of cases, congenital stridor is observed in children under one year of age, caused by congenital anomalies in the development of the respiratory tract. The acquired pathological condition of stridor is usually the result of processes such as:
- ingestion of foreign objects through inhalation, for example, food bolus or small parts of toys during children's games;
- burns or smoke inhalation;
- tumor formation in the larynx, esophagus or trachea, more often with the development of squamous cell carcinoma ;
- congenital heart defects or mediastinal tumors;
- infections leading to epiglotitis , paratonsilial and retropharyngeal abscess , diphtheria, tuberculosis, syphilitic, influenza croup or papillomatosis , post-traumatic encephalopathy, arachnoiditis , bulbar or pseudobulbar syndrome ;
- swelling of the respiratory tract, which is not of an infectious nature, but of a toxic or allergic nature;
- prolonged intubation and the development of subglottic stenosis, in more rare cases - subglottic hemangioma ;
- the presence of vascular rings compressing the trachea;
- development of thyroiditis or tumors of the thyroid and thymus glands;
- tetany;
- paralysis of the vocal folds or larynx;
- post-intubation period or paradoxical movements during inspiration, causing laryngospasm .
What is stridor and why is it dangerous?
The baby is breathing noisily and with difficulty. What's wrong with it, and is it dangerous? Let's talk about stridor.
What is stridor
Stridor is the name given to characteristic sounds that occur during pathological (abnormal, difficult) breathing in a child, when, due to the congenital characteristics of the larynx or trachea or for other reasons (more on them later), the air encounters obstacles (that is, obstruction occurs), as a result it comes out with noise or whistling.
Causes of stridor
Stridor occurs for many reasons, which for simplicity we will call congenital anomalies. These include narrowing of the airways, abnormal structure of the cartilage of the larynx, less commonly, paralysis of the vocal cords, and much more. The causes of congenital stridor can be pathologies of the cardiovascular system and damage to the central nervous system.
However, sometimes stridor is a symptom of infectious diseases, enlarged lymph nodes, vascular abnormalities in the larynx, tumors, or a sign that a foreign body has entered the baby’s respiratory tract. Asthma also sometimes causes intermittent stridor.
The cause may also be hidden in the nasal cavity (for example, inflammation of the tonsils or adenoids) - in this case, stridor most often occurs when the child is sleeping.
Symptoms of congenital stridor
- noisy, labored breathing that gets worse with crying or coughing
- shortness of breath
- cardiopalmus
Diagnosis of stridor
Stridor is hard to miss. A preliminary diagnosis is made by a pediatrician and confirmed by an otolaryngologist based on examinations - radiography of the larynx and soft tissues of the neck, ultrasound of the larynx, computed tomography, tracheobronchoscopy, laryngoscopy, fiberoscopy, esophagoscopy. The doctor will determine which ones are needed based on the child’s condition and medical history.
Treatment of stridor
It is generally believed that congenital stridor is a “growing pain.” That is, as the child grows older (by about 3 years) and the cartilage of the larynx grows, the stridor goes away on its own. It is enough to see an otolaryngologist regularly. In some cases, surgery is required to relieve breathing difficulties.
If stridor is caused by aspiration (a foreign body entering the respiratory tract), then this body is removed from there. In the case of inflammatory diseases, the doctor will first alleviate the child’s condition (breathing), then begin treating the diseases themselves. He may prescribe bronchodilator inhalations, antibiotics, even surgery - it all depends on the cause of stridor.
Why is stridor dangerous?
The danger of stridor is that it can be not only a result, a manifestation of difficulty breathing in a baby, but also a symptom of more serious diseases.
The risk assessment takes into account the volume of the stridor, the pitch of the sound, and the phase of breathing during which the stridor occurs. We'll leave the nuances to the doctors, but parents should be alerted to a sudden (not gradual) weakening of stridor: if the usually loud breathing noise suddenly becomes weaker, almost unnoticeable, perhaps the obstacles in the larynx have increased, and breathing difficulties have increased. In this case, you should consult a doctor.
In addition, when acute infectious diseases or inflammation of the respiratory tract occur in the body (for example, pneumonia, bronchitis and other diseases), stridor can intensify, manifesting itself in acute attacks, causing panic and suffocation in the baby and parents.
Acute attacks of stridor can occur due to laryngeal stenosis (false croup), diphtheria, retropharyngeal abscess, inflammation of the epiglottis (epiglottitis).
When assessing the danger of stridor, the doctor will definitely ask the parents about the time when noisy breathing began and the circumstances under which it occurred. The early occurrence of stridor indicates its congenital nature. If stridor occurs between the ages of 6 months and 2-3 years, then the first suspicion will be that a foreign body has entered the respiratory tract. If before the onset of stridor the baby was absolutely healthy and breathing was silent, then it is necessary to urgently consult a doctor. If there were symptoms of malaise (fever, crying, lack of appetite, hoarseness), then we are probably talking about an infectious disease, in which it is necessary to call an emergency doctor, since infectious diseases progress quickly in children.
So when to call the doctor?
Doctors will most likely notice a congenital condition in the maternity hospital. If we are talking about acquired stridor (that is, one that arose at an older age), then you should consult a doctor immediately, since many causes of stridor are conditions that seriously threaten health and life.
Prevention of stridor
- Be attentive to the baby, do not leave small and sharp objects in his reach that the child could put in his mouth or nose.
- Ventilate the apartment regularly, remember about personal hygiene (changing towels, washing hands), limit communication during periods of false croup epidemics.
- Vaccinations against diphtheria and Haemophilus influenzae according to the vaccination calendar will help protect the child from these diseases (thereby preventing the occurrence of stridor).
Symptoms
There are many comparisons and descriptions of congenital stridor - reminiscent of the cooing of pigeons, the purring of cats, the clucking of a chicken, etc. However, in most cases the sound is transient, whistling and ringing. Moreover, the child’s voice is the same ringing, clear, general health is normal, breathing is practically not difficult (in some cases, inhalation may be difficult), the sucking process is normal.
Other symptoms associated with stridor include:
- ringing cough with a metallic tint;
- salivation;
- hoarse voice;
- the presence of such signs of respiratory failure as shortness of breath , accompanied by retraction of the intercostal spaces and the participation of auxiliary muscles;
- anxiety;
- rapid breathing and heart rate;
- depression and anxiety;
- increasing obstruction can lead to cyanosis .
To reduce the sound intensity, it is enough to move the child to a warmer room or lay him on his stomach. Also, stridor in infants subsides during sleep, but increases if the child performs physical activity, screams, is nervous, or coughs. If there is normal growth and development of the cartilage of the larynx, then closer to the age of one year, stridor may spontaneously subside; otherwise, stridor in children may occur at rest, which requires immediate hospitalization.
Expiratory stridor breathing can intensify with the progression of edematous-inflammatory narrowing of the bronchi and an increase in expiratory force.
Tests and diagnostics
The examination begins with a history and physical examination. It is important to detect the cause and level of obstruction in the airways. Thanks to the height of stridor and its connection with the phases of breathing, it is possible to determine the location of the obstruction:
- if the sound of stridor is high, then the narrowing of the lumen of the larynx is at the level of the vocal cords;
- low - the narrowing is more likely localized above the vocal folds in the laryngopharynx or upper larynx;
- with an average height of stridor, the obstruction is most likely located below the vocal cords;
- if stridor occurs during inspiration, then the obstruction is usually localized above the prominence of the vocal folds; when stridor occurs during exhalation, it is usually lower;
- when stridor is biphasic, this may indicate an obstruction located in the vocal folds or subglottic apparatus of the larynx.
To obtain a more complete picture and determine the nature of structural changes in the respiratory tract, fiberoscopy , direct laryngoscopy under anesthesia, tracheobroncho- or esophagoscopy , radiography of the neck and chest, bronchoscopy, CT and MRI are performed.
Breathing rhythm disturbance
Stroke
Hepatitis
Diabetes
Encephalitis
Thyrotoxicosis
17619 08 April
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Irregular breathing: causes, diseases in which it develops, methods of diagnosis and treatment.
Definition
Respiration is a set of physiological processes whose ultimate goal is the delivery and consumption of oxygen, as well as the removal of carbon dioxide.
The respiratory organs include the airways and lungs. In addition, the muscular and nervous systems take part in the breathing process. Thanks to the diaphragm, intercostal and some other muscles, respiratory movements are performed, a change in the volume of the chest occurs, which is a necessary condition for the expansion and collapse of lung tissue during inhalation and exhalation. The respiratory center is located in the central nervous system, namely in the medulla oblongata. The key feature of the functioning of the respiratory center is the automatic generation of impulses in it - that is, the person does not think about the fact that he needs to take a breath. At the same time, the activity of the respiratory center can be suppressed by higher-lying parts of the brain; for example, a person can voluntarily hold his breath while diving.
It is the respiratory center of the medulla oblongata that plays a key role in maintaining the rhythm of breathing.
Types of breathing rhythm disturbances
The following types of breathing are distinguished:
- eupnea
– normal breathing rhythm (in a healthy adult it is about 14–18 respiratory movements per minute); - hyperpnea
– deep and rapid breathing, observed during muscular work, emotional stress, thyrotoxicosis, anemia, acidosis, decreased oxygen content in the inhaled air; - tachypnea
- an increase in the frequency of respiratory movements due to pronounced stimulation of the respiratory center during hypercapnia, hypoxemia; observed with increased body temperature, congestion in the lungs, etc.; - bradypnea
- a decrease in the frequency of respiratory movements, which occurs when the respiratory center is damaged and depressed against the background of hypoxia, edema, ischemia and exposure to narcotic substances; - apnea
– temporary cessation of breathing (considered the extreme severity of bradypnea); - Cheyne-Stokes breathing
- characterized by alternating groups of respiratory movements with increasing amplitude and periods of apnea; - breathing according to the Biota type
- characterized by alternating periods of apnea with groups of respiratory movements of equal amplitude; - Kussmaul breathing
is noisy and deep breathing, which is characterized by separate convulsive contractions of the main and auxiliary respiratory muscles. This type of breathing indicates significant hypoxia of the brain.
Possible causes of respiratory rhythm disturbances
The immediate cause of respiratory rhythm disturbances is a change in the functioning of the respiratory center. The respiratory center has numerous connections with other parts of the nervous system and with receptors (nerve endings) that perceive changes in the internal environment of the body: changes in the concentration of oxygen and carbon dioxide in the blood, blood acidity, etc. For example, with a decrease in the concentration of oxygen in the blood, an increase in the concentration of carbon dioxide and acidification of the blood, receptors that activate the respiratory center are excited. In turn, an increase in the frequency and depth of breathing compensates for changes in the gas and acid-base composition of the blood.
The respiratory center can be directly affected by certain brain-toxic substances circulating in the blood.
Disturbances in the functioning of the respiratory center occur as a result of structural changes in the corresponding area of the brain during strokes, cerebral edema, etc.
Diseases that cause breathing problems
Among the diseases that lead to the accumulation of toxic substances in the blood, which can subsequently irritate or damage the respiratory center, it is worth mentioning the following:
- diabetes mellitus in the stage of decompensation
, when carbohydrate metabolism products accumulate in the blood; occurs at the onset of previously undiagnosed diabetes mellitus or with insufficient control of the disease during insulin therapy and glucose-lowering therapy; - liver failure
, developing acutely against the background of hepatitis (viral, alcoholic, autoimmune etiology, etc.), toxic liver damage (for example, paracetamol poisoning), as well as chronic intoxication with liver failure against the background of cirrhosis. Toxic damage to the brain in liver diseases is primarily due to the fact that the pathologically altered liver is not able to perform a barrier function (retain and neutralize harmful substances), and therefore toxins accumulate in the blood; - renal failure
, which can manifest acutely or have a long-term chronic course, develops against the background of inflammatory diseases (glomerulonephritis, tubulointerstitial nephritis, etc.), toxic damage to the kidney (for example, tubular necrosis) and other diseases; - Severe infectious diseases
can cause severe intoxication or lead to direct brain damage, for example, in viral or bacterial encephalitis.
Respiratory rhythm disturbances can occur during poisoning with opium-type drugs that cause bradycardia and apnea.
Structural changes in the brain are observed during strokes (acute cerebrovascular accident due to hemorrhage or blockage of cerebral vessels by a blood clot), neoplasms, and cerebral edema.
Separately, it is worth mentioning Pickwick's syndrome, which develops in patients with severe obesity, one of the manifestations of which is episodes of respiratory arrest during sleep.
Which doctors should I contact if my breathing rhythm is disrupted?
Irregular breathing is a serious symptom, so often the first specialist to assist a patient is an emergency physician or resuscitator.
If a violation of the breathing rhythm does not pose a threat to life, then diagnostic measures are carried out by a doctor of a narrower specialty: a hepatologist (a specialist in liver diseases), a nephrologist (a specialist in kidney diseases), a toxicologist, an infectious disease specialist, etc.
Diagnostics and examinations for respiratory rhythm disorders
Diagnosis begins with a survey of the patient, during which the doctor establishes possible causes and risk factors for the development of arrhythmic breathing.
Laboratory tests include determination of blood glucose levels, arterial blood gases and the acid-base status of the blood CBS.
Stridor in children
The most common cause of stridor that occurs immediately after birth is tracheo(laryngo)malacia or tracheobronchomalacia.
Anatomical changes in laryngomalacia include stenosis of the larynx, the presence of additional folds of the mucous membrane, and the retraction of the soft epiglottis into the larynx due to the tightened arytenoid cartilages or being pulled up during inspiration. In other cases of mixed forms of laryngomalacia, the aryepiglottic folds may be shortened and not only the epiglottis, but also the arytenoid cartilages will be pushed into the lumen of the respiratory passages. Laryngomalacia is characterized by a “benign” course with spontaneous resolution at the age of approximately 1.5-2 years. In boys, this deviation occurs 2 times more often than in girls.
2. Reasons
According to modern concepts, congenital stridor is due to genetic reasons; the question of the possible influence of harmful factors at the stage of gestation (gestation) needs further study using extensive statistical material.
Weakness of the outer ring of the larynx (so-called laryngomalacia, literally “softening of the larynx”) and infantility of the arytenoid cartilages lead to retraction of the epiglottis and aryepiglottic folds of the mucous membrane into the lumen of the airway, which is the direct cause of turbulent breathing. Congenital stridor is often observed in premature infants; in many cases it is accompanied by other congenital malformations.
Visit our Otolaryngology (ENT) page
Diet for stridor
Diet for pulmonary tuberculosis
- Efficacy: no data
- Dates: no data
- Cost of products: 1900-2000 rubles. in Week
The diet for respiratory system disorders should be high in protein and high in vitamins. The energy value is possible in the range of 200-2900 calories, depending on the characteristics of the body.
It is important that all necessary nutrients are present;
- complete proteins (110-120 g) – the most preferred content in poultry and veal;
- fats (80-90 g) – sources of which are seeds, nuts, unrefined mala and fish;
- fiber and carbohydrates (250-330 g) - found in fruits, vegetables and herbs, it is recommended to enrich the diet with apples, pears, oranges, mangoes, tomatoes, cucumbers, zucchini, eggplants, as well as berries - strawberries, blueberries, currants, raspberries, etc. .;
- vitamins A, B, C - rich in rosehip decoctions, liver, bran, citrus fruits, carrots and all possible yellow vegetables and fruits.
All synthetic substances and products are prohibited.