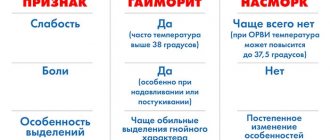
Everyone knows what a runny nose is or, as doctors call it, rhinitis. A runny nose almost always accompanies colds, flu and other respiratory diseases. Most often, rhinitis has an acute form, that is, it develops quickly and quickly subsides.
If acute rhinitis is not treated in time, it may develop into a chronic form. Rhinitis begins to torment a person all year round. Sometimes it seems that it has completely passed, but at the slightest weakening of the immune system it makes itself felt again. Allergy sufferers are also very familiar with the chronic manifestation of rhinitis, which instantly wakes up when the body is exposed to an intolerable allergen.
Like most diseases, chronic rhinitis has its own forms, from familiar and simple to complex and dangerous. Among this diversity, a rather rare form of chronic rhinitis stands out - atrophic rhinitis.
Atrophic rhinitis is a slowly progressive disease that affects the nasal mucosa. Hard crusts with an unpleasant odor form, the nasal passages increase in size, and the person is constantly haunted by a feeling of stuffiness. The disease affects adults, mainly women, and children, most often teenagers.
Recently, atrophic rhinitis has become commonly divided into primary and secondary. The primary develops independently, and the secondary manifests itself against the background of intervention - environmental, physical, surgical and infectious1,2.
Development and causes of atrophic rhinitis
The key difference from other types of rhinitis is that atrophic rhinitis develops dystrophically, that is, the nasal mucosa changes structurally, at the cellular level.
Atrophy occurs locally or covers the entire nasal mucosa. The number of goblet cells (upper layer) of the mucous membrane decreases, the viscosity of the secretion changes2.
Scientists still do not know the exact reasons for the appearance of the first type of atrophic rhinitis, which develops independently, without support from colds or other diseases. It is assumed that the cause in adults and children may be heredity, unfavorable environment, immunological disorders and improper blood circulation in the nasal area1. But at the moment, the first type of atrophic rhinitis develops extremely rarely, its main area of distribution is Africa and East Asia1.
The most common cause of secondary atrophic rhinitis in adults and children is surgical intervention in the nasal cavity, such as resection or removal of the turbinates2. In addition, development is facilitated by problems with immunity, nutritional deficiencies, chronic forms of other diseases of the respiratory system, such as sinusitis, as well as a whole list of various bacterial infections.
Separately, it is worth mentioning the development of atrophic rhinitis in children. Adolescents during puberty, especially girls, are at risk. Most likely, this is due to sharp hormonal surges in the body, as well as vitamin deficiency and a decrease in immune resistance3.
If the problem is not solved, then atrophic rhinitis has a good chance of developing into ozena - a foul runny nose. Ozena is characterized by complete damage to the entire mucous membrane and thick secretions with a distinct fetid odor. This disease is considered a serious complication requiring immediate treatment2.
2. Reasons
The causes and mechanisms of atrophic rhinitis today are not sufficiently clarified, so the results of new studies, hypotheses and statistical data on risk factors are constantly appearing. Thus, hypotheses about hereditary predisposition, the influence of endocrine imbalances and disorders, the role of psychogenic, autoimmune, hemodynamic, nutritional, environmental, and occupational factors are considered and discussed. Many authors see the influence of hypovitaminosis and iron deficiency. In some cases, there is a connection with previous medical interventions, injuries, infections, radiation and chemotherapy. A very serious factor in mucosal atrophy, the significance of which has been confirmed repeatedly, is the abuse of local vasoconstrictors (vasoconstrictor drops), which often turns into severe drug dependence.
In relation to ozena, the role of a specific pathogen has been proven - Klebsiella ozena, but fungal, Proteus, diphtheroid atrophic rhinitis also occurs; the possible role of viral infections as a trigger factor is assumed.
In general, the etiopathogenesis of chronic atrophic rhinitis needs further study.
Visit our Otolaryngology (ENT) page
Symptoms of atrophic rhinitis
A short list of the primary signs of atrophic rhinitis in adults and children:
- A feeling of dryness in the nose is the first main symptom.
- The formation of dense crusts in the nasal cavity is the second main symptom.
- Problems with smell
- Trouble breathing through the nose.
- Sensation of a foreign body in the nose3.
The above symptoms of atrophic rhinitis in adults and children are characteristic of both types of disease - primary and secondary. People complain of dryness and itching in the nose, the formation of crusts of an unpleasant color and odor. Removal of crusts is accompanied by pain and injury to the mucous membrane1.
Primary atrophic rhinosinusitis
Primary atrophic rhinosinusitis is more often diagnosed in patients from low socioeconomic status groups living in geographic areas with warm climates. Areas of high prevalence include southern Saudi Arabia, China, Africa, India, the Mediterranean and the Philippines.
Atrophic rhinosinusitis is more common in women. It is diagnosed more often at young ages than at older ages.
Clinical picture
Patients experience a constant sensation of an unpleasant odor in the nose (this disorder of smell is called cacosmia). At the same time, there is also an unpleasant odor from the mouth, noticeable to others. This is where the term “ozena” (“stench”) comes from, which is sometimes used as a synonym for severe primary atrophic rhinosinusitis.
Other symptoms include lack of sense of smell (anosmia), nosebleeds, nasal pain, sleep disturbances, and suffocation due to excessive crusting.
Patients complain of nasal congestion even with excessively wide nasal passages, which is better characterized by the concept of “lack of sensation of breathing.” Nasal congestion occurs due to improper passage of air through the nasal cavity, lack of resistance and sensation of air flow due to loss of tissue containing sensory receptors. The same phenomenon is observed in patients with perforation of the nasal septum.
The disease is characterized by the replacement of normal pseudostratified columnar epithelium with squamous epithelium. This tissue lacks cilia and mucus-producing goblet cells.
The most common culprits of the bacterial process in the nose are Klebsiella ozaenae, Proteus, Escherichia coli, Staphylococcus aureus, Streptococcus pneumoniae.
ENT examination
During rhinoscopy (examination of the nose), the doctor sees a shiny, thin, pale, and sometimes ulcerated mucous membrane, covered with thick yellow, brown or green crusts, sometimes bloody, covered with a purulent coating. Resorption (destruction) of the underlying cartilage and bone leads to an increase in the volume of the nasal cavity. Some patients are diagnosed with perforation of the nasal septum and secondary saddle deformation of the external nose (recession of the nasal dorsum).
Predisposing factors to the development of primary atrophic rhinosinusitis are completely unknown. It is discussed that these could be endocrine, vascular, infectious and autoimmune diseases, as well as occupational hazards (working in dusty, contaminated areas with chemical or industrial dust).
Computed tomography of the nose and paranasal sinuses
Possible finds include:
- atrophy of the mucous membrane of the lower and middle turbinates and bone resorption;
- resorption of cells of the ethmoidal and uncinate labyrinth;
- an increase in the volume of the nasal cavity with destruction of its lateral walls;
- thickening of the mucous membrane of the paranasal sinuses;
- hypoplasia (reduction) of the maxillary sinuses with a decrease in their pneumatization (airiness).
Treatment of atrophic rhinitis
Almost any doctor can diagnose atrophic rhinitis using rhinoscopy - changes in the nasal cavity are immediately noticeable. After diagnosing and confirming the diagnosis, the doctor will tell you how to treat atrophic rhinitis.
The main goal in the treatment of atrophic rhinitis is to restore all functions. Doctors recommend comprehensive treatment, including therapeutic measures and medications.
Therapeutic treatment includes:
- Moisturizing the nasal mucosa
- Normalization of temperature at the place of stay
- Increasing air humidity
Among the proven medications:
- Inhalation and irrigation of the nasal mucosa with sea salt solutions
- Angioprotectors - drugs that improve the activity of blood vessels
- Immunostimulants
- Antibacterial drugs
- Iron supplements
- Antibiotics3
Vasomotor rhinitis (“false rhinitis”)
A characteristic feature of vasomotor rhinitis is the manifestation of a runny nose symptom complex without pathological signs of inflammation of the mucous membrane. This is either a neurovegetative runny nose, which is a manifestation of autonomic neurosis, or an allergic one, which occurs in response to the action of allergens.
The basis of the neurovegetative form of vasomotor rhinitis is the inadequate “play” of the vessels that make up the main content of the cavernous bodies of the turbinates. These are cycles characterized by regular narrowing and expansion of the vessels of the nasal concha. Subjectively, no nasal breathing disturbances are felt. This alternating cyclical fluctuation of nasal congestion can be considered as a normal manifestation of physiological functional asymmetry. On the other hand, a more pronounced enlargement of the nasal turbinates, in which a clearly felt difficulty in nasal breathing appears, is a pathological condition, namely vasomotor rhinitis, in particular its neurovegetative form.
In healthy individuals, a change in the predominance of breathing through one or another half of the nose occurs according to a sinusoidal law with a period of 20 to 90 minutes, and the ratio of the volumes of exhaled air varies from 25% to 75%, i.e. complete congestion of one half of the nose is not observed. In patients with the neurocirculatory form of vasomotor rhinitis, there is a violation of the period and linearity of the law of change in the predominance of nasal breathing. Their exhaled air volume ratio ranges from 0% to 100%.
In the occurrence of the neurovegetative form of vasomotor rhinitis, the main role is played by functional changes in the central and autonomic nervous systems, as well as the endocrine system. The hypothalamus, the main integrating autonomic center in the regulation of nasal functions, plays an important role. The influence of dysfunction of the endocrine glands, primarily the thyroid gland, on the development of vasomotor rhinitis is also important. Vasomotor rhinitis is an endocrine-vegetative syndrome.
The development of vasomotor rhinitis is also facilitated by reflex effects, in particular: cooling, to which non-hardened people are especially susceptible; sedentary lifestyle; medications used for hypertension and coronary heart disease to dilate blood vessels, etc. Vasomotor rhinitis often occurs in people who have spines and ridges on the nasal septum.
Allergic form
The allergic form of vasomotor rhinitis occurs when exposed to various allergens, and depending on their name, seasonal and permanent (year-round) forms of allergic rhinitis are distinguished. Allergic rhinitis is one of the most common diseases. According to various studies, they occur in 10 - 40% of the population.
The cause of the seasonal form of allergic rhinitis (hay fever) can be pollen from various plants during their flowering period. Residents of many cities are especially concerned about the fluff and pollen of poplars, while rural residents are concerned about the cereals blooming in the fields (timothy, fescue, etc.). In recent years, ragweed, an overseas cereal that has penetrated into the southern regions of Russia from North America and has increased allergenic properties, has become relevant.
In the permanent (year-round) form of allergic rhinitis, the allergens are more diverse and can affect patients over a long period. These include: environmental allergens - book dust, relevant for library workers; house dust, bird feathers (feather pillows), hair, pet dander, daphnia (dry food for fish living in an aquarium); food products - citrus fruits, strawberries, honey, milk, fish, crayfish; medicines, perfumes, etc.
The pathogenesis of allergic rhinitis involves a specific reaction between the allergen and tissue antibodies, resulting in the release of chemically active substances (allergic reaction mediators) that contribute to the development of clinical manifestations of the disease. The possible mechanism of development of allergic rhinitis is described as follows.
An Ig E-dependent reaction occurs - activation of mast cells located in the nasal mucosa. The released mediators are contained in granules (for example, histamine and tryptase) or in the membrane of mast cells (leukotrienes and prostaglandins). Another mediator is platelet activating factor (PAF). Mediators have a vasodilating effect and increase vascular permeability, which leads to nasal congestion. Increased secretion is accompanied by the appearance of mucous discharge. Stimulation of afferent nerve fibers causes itching and sneezing. In addition, afferent stimulation (especially under the influence of histamine) can enhance the axonal reflex with local release of neuropeptides (substance P, tachykinins), which, in turn, cause further degranulation of mast cells, further enhancing the pathological response.
Neurovegetative form
In the neurovegetative form of vasomotor rhinitis, no specific changes in the mucous membrane are observed. The ciliated epithelium is thickened, the number of goblet cells is increased. The cavernous vessels are dilated. Microcirculation is disrupted. These disturbances are especially noticeable in the inferior turbinates. The movement of blood in the capillaries is uneven and often does not correspond to pulse impulses. In the allergic form of vasomotor rhinitis, stasis occurs. The epithelial cover of the mucous membrane thickens, in places metaplasizing into a multilayered flat layer. The number of goblet cells increases significantly. In the subepithelial layer, tissue infiltration with eosinophilic leukocytes takes place. They are also found in significant quantities in nasal mucus.
Clinic of the neurovegetative form of vasomotor rhinitis
As with all forms of vasomotor rhinitis, the neurovegetative form is characterized by the following symptoms: difficulty in nasal breathing, profuse serous or mucous discharge, attacks of paroxysmal sneezing, itching and burning sensation in the nasal cavity. These symptoms are often intermittent. They can occur after waking up from sleep (a change in the predominance of the parasympathetic over the sympathetic autonomic nervous system), with a change in ambient temperature, with overwork, emotions, stress, etc. Difficulty in nasal breathing is associated with the expansion of the cavernous spaces of the nasal mucosa, mainly the lower nasal shells The mucous membrane has a bluish color due to blood overflow (venous hyperemia). "Bluish or pale" spots are often visible. Lubricating the mucous membrane with vasoconstrictor drugs leads to rapid contraction of the conchae.
Clinic for seasonal allergic rhinitis (hay fever)
This form of vasomotor rhinitis is characterized by a clear seasonality of exacerbation, which occurs during the flowering period of plants to the pollen of which patients have increased sensitivity (sensitization). During this period, paroxysms of sneezing, itching and burning in the nasal cavity, eyes, and conjunctival hyperemia are noted. Almost complete nasal congestion and severe rhinorrhea occur, which leads to maceration of the skin in the vestibule of the nose. The mucous membrane in the initial period is sharply hyperemic, and there is a significant amount of clear fluid in the nose. Subsequently, the mucous membrane acquires a cyanotic appearance and then turns pale. Along with the noted rhinological symptoms, patients during this period often experience itching in the eyes, conjunctival hyperemia, a feeling of rawness in the pharynx, larynx and skin itching. In some cases, it is possible to develop Quincke's edema (enlargement of the face or part or limb) and larynx. Various discomfort manifestations are observed, incl. headache, increased fatigue, sleep disturbance, increased body temperature. The duration of the disease usually corresponds to the period of flowering of plants and ceases on its own after its end or after the patient changes the allergenic area.
An intermediate position between the neurovegetative form of vasomotor rhinitis and seasonal allergic rhinitis is occupied by the so-called. "neurosis of a reflected nature." Thus, in people suffering from hay fever, which occurs when smelling flowers, in particular roses, attacks of a runny nose are observed not only when inhaling the aroma of flowers, but also when just looking at an artificial rose, which the patient mistakes for a real one. In these cases, there is a combination of conditioned reflexes coming from the optic and olfactory nerves.
Clinic for permanent (year-round) form of allergic rhinitis
The disease is chronic from the very beginning. Severe swelling of the nasal turbinates is detected, associated with profuse sweating of transudate from the capillaries. The mucous membrane is pale; swelling affects not only the turbinates, but also the mucous membrane of the bottom of the nasal cavity and the nasal septum. The middle turbinates are also swollen, resembling polyps. Due to swelling of the mucous membrane, mucus is difficult to clear and can be discharged from the nose at random.
The allergic form of vasomotor rhinitis is characterized by the formation of mucous polyps. Gradually increasing in size and quantity, they can fill the entire nasal cavity, in some cases pushing apart the bone walls and deforming the external nose. Often there is a combination of allergic rhinitis with bronchopulmonary pathology - asthmatic bronchitis and bronchial asthma. An “asthmatic triad” may occur, including intolerance to acetylsalicylic acid, nasal polyposis and attacks of bronchial asthma.
Treatment of the neurovegetative form of vasomotor rhinitis
It consists of eliminating various causes, often of a reflex nature, that cause this disease. It is necessary to treat general diseases (neuroses, diseases of internal organs, endocrine dysfunction). If there are any local abnormalities in the nasal cavity (Conchabullosa, spines and ridges of the nasal septum), they should be eliminated. An active, mobile lifestyle and hardening procedures are recommended, in particular, effects on reflex zones - short-term dousing of cold water on the soles of the feet. Performing various gymnastic exercises.
Systematic use of vasoconstrictors is not recommended, because this gives only a short-term effect, and with prolonged use it damages the mucous membrane and is addictive. Acupuncture is also used, influencing the reflex zones of the nasal cavity (novocaine blockades in the inferior nasal turbinates, in the aggernasi, on the sphenopalatine node). Surgical interventions on the inferior turbinates (various options for intraturbinate disintegration) are more effective.
Treatment of allergic rhinitis
There are three main areas in the treatment of allergic rhinitis: elimination therapy, immunotherapy and drug therapy. The goal of elimination therapy is to eliminate allergens (pollen, dust, etc.) and control the state of the environment. Specific immunotherapy is very effective, but severe reactions are possible, especially in people suffering from bronchial asthma. It is not widespread in our country. In other countries (Great Britain, Scandinavian countries), the use of specific immunotherapy is sharply limited. To minimize the risk of immunotherapy, the question of its appropriateness should be decided by an allergist or clinical immunologist. Currently, drug therapy for allergic rhinitis has acquired the greatest importance.
Our medical center successfully treats various types of chronic rhinitis!
Cost of ENT services in our Medical Center
Rating 4.09 (11 Votes)
Helping the immune system with atrophic rhinitis
One of the effective remedies that can help with atrophic rhinitis is IRS®19. The medicine is an immunostimulant. It contains bacterial lysates (bacterial particles), which stimulate local immunity. Antibodies are formed on the nasal mucosa damaged by infection, which prevent the proliferation of harmful bacteria. In addition to this, the amount of lysozyme, an antibacterial substance that destroys the cells of already established bacteria, increases.
IRS®19 is produced in the form of an aerosol (spray), in easy-to-use bottles5. This form is especially suitable for children. The nebulizer is inserted into the nasal cavity, and by pressing the valve once, the medicine is delivered directly to the site of infection.
The drug has a high safety profile and is prescribed to children from 3 months. That is why the drug is common in the treatment of many diseases in children associated with bacterial or viral infections of the respiratory system4.
In addition to the treatment of atrophic rhinitis and other types of chronic rhinitis, IRS®19 has confidently proven itself in the prevention of ARVI. If the disease occurs, then children under 3 years of age are prescribed an injection of IRS®19, one dose into each nasal passage twice a day. Adults and children over 3 years of age use IRS®19 2 to 5 times a day, one injection5.
Chronic hypertrophic rhinitis
The causes of hypertrophic rhinitis are the same as catarrhal ones. The development of one form or another of chronic rhinitis is apparently associated not only with the influence of external unfavorable factors, but also with the individual reactivity of a person.
Pathomorphological changes
Pathomorphological changes in hypertrophic rhinitis differ from those in catarrh by the predominance of proliferative processes. The development of fibrous tissue is observed mainly in places where cavernous formations accumulate. Hypertrophy of the mucous membrane of the nasal concha often reaches significant sizes. There are three types of shell hypertrophy: smooth, tuberous and polypous. It can be diffuse and limited. The most typical sites of hypertrophy are the anterior and posterior ends of the inferior and anterior ends of the middle turbinate. Hypertrophy can also occur in other areas of the nose - in the anterior part of the nasal septum and at its posterior edge, on the vomer.
Swelling of the mucous membrane in the area of the nasal turbinates, especially the middle one, is possible, resembling nasal polyps. This swelling and polyp-like thickening, unlike polyps, has a wide base. In the future, polypous hypertrophy can gradually transform into polyps. This is facilitated by allergization of the body (auto- and exogenous). Occurring bony hypertrophy of individual turbinates is a variation of the anomaly of nasal development.
Clinic and symptoms of chronic hypertrophic rhinitis
Hypertrophic rhinitis is characterized by constant nasal congestion, which depends on excessive enlargement of the nasal turbinates, which practically do not contract under the influence of vasoconstrictors. Nasal breathing is complicated by copious mucous and mucopurulent discharge. Due to obstruction (narrowing) of the olfactory fissure, hyposmia occurs and then anosmia. In the future, as a result of atrophy of the olfactory marks, essential (irreversible) anosmia may occur. The timbre of the voice becomes nasal (rhynolaliaclausa).
As a result of compression of the lymphatic gaps by fibrous tissue, lymphatic drainage from the cranial cavity is disrupted, which causes a feeling of heaviness in the head, impaired ability to work, and sleep disturbances.
Shutting off nasal breathing leads to impaired ventilation of the paranasal sinuses, as well as disease of the underlying respiratory tract. Hypertrophy of the posterior ends of the inferior turbinates disrupts the function of the auditory tube and leads to tubo-otitis. Thickening of the anterior sections of the inferior turbinates can compress the nasolacrimal duct with subsequent development of dacryocystitis and conjunctivitis.
Treatment of chronic hypertrophic rhinitis
Endoscopic examination allows us to determine the nature of hypertrophy. Further treatment of hypertrophic rhinitis is predominantly surgical. Treatment methods for diffuse hypertrophy pursue the development in the postoperative period of a sclerosing scar process in the submucosal layer, which reduces the size of the nasal turbinates. For this purpose, various methods of intrashell cauterization of tissue are used (electricity - electrocautery, ultra-low temperatures - cryodestruction), as well as such effects as ultrasonic or mechanical disintegration. A laser beam is also used for this purpose.
How to treat chronic runny nose in adults. Methods and means of treatment
Depending on the causes of the disease, the following treatment methods are used:
- Possible measures are being taken to eliminate the irritating factor.
- A medication is prescribed to help with chronic runny nose.
- For medical indications, surgery is performed (correction of a deviated nasal septum, removal of tumors).
- Physiotherapeutic methods are used.
- Climate therapy is recommended.
The following drugs are currently used:
- Special moisturizing mucous membrane products.
- Medicines to improve trophism of the nasal mucosa.
- Hormonal drugs.
- Salt solutions and products based on sea water, etc.
The best remedy for chronic runny nose is one that is suitable for a specific form of the disease and is adapted to the course of the patient’s illness and the characteristics of his body. Treatment measures must be comprehensive.
Prevention
Competent prevention allows you to avoid severe illness of any disease. In many cases, thanks to such measures, a person does not get sick at all, this is:
- competent and timely treatment of any ENT pathologies;
- exclusion of allergens;
- elimination of congenital anomalies through surgical correction;
- the use of moisturizers and products with sea tar;
- healthy lifestyle;
- rejection of bad habits;
- taking medications to strengthen the body and improve immunity.
How to cure chronic runny nose? After making a diagnosis, you should buy a modern, high-quality remedy for chronic runny nose, which was prescribed by a specialist. Affordable drugs for the treatment of all forms of the disease are available in a wide range in the Stolichka social pharmacies network.