What is congenital hypothyroidism in children
Congenital hypothyroidism (ICD code 10 - E03) is a congenital disease of the thyroid gland, which is characterized by the inability to produce thyroid hormones or their insufficient quantity. Congenital hypothyroidism is scary because it prevents the child’s body from growing and developing normally; various forms of mental and physical development delay occur.
According to statistics, this disease occurs in one baby out of 4-5 thousand. Most often, the pathology occurs in girls: 2-2.5 times more often than in newborn boys.
Causes of congenital hypothyroidism
The causes of hypothyroidism in newborns can be varied. The disease itself develops due to abnormal development of the thyroid gland. Such an anomaly may be abnormal intrauterine development of the fetal organs: the thyroid gland may develop in the space behind the sternum or in the sublingual space, in addition, the tissues of the organ itself may be underdeveloped or completely absent.
The disease can also be caused by unfavorable factors affecting a woman during pregnancy:
- poor nutrition (lack of vitamins and minerals, important nutrients for the thyroid gland iodine and selenium);
- infectious diseases;
- autoimmune diseases;
- intoxication of the body;
- abuse of various medications;
- being in a radioactive irradiation zone.
According to statistics, hypothyroidism is a genetically determined pathology in only 2% of newborns.
Consequences of the disease
The consequences of insufficient thyroid hormone production can be catastrophic for a child without the necessary treatment.
Consequences of congenital hypothyroidism:
- delay in physical, emotional and intellectual development;
- since thyroid hormones affect the functioning of many organs, we can talk about emerging pathologies also from the heart, nervous system and psyche;
- in advanced cases, myxedema occurs (insufficiency of thyroid hormones in tissues and other organs), which leads to the patient’s coma.
Dear patients, in our medical center you can do an ultrasound of the thyroid gland.
Description of the disease
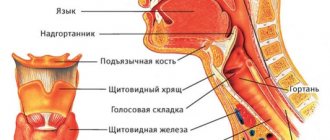
The thyroid gland begins to work already by the 12th week of intrauterine development, releasing three basic hormones into the body: thyroxine (T4), triiodothyronine (T3). They regulate the formation of organs and tissues, including the cerebral cortex, which is responsible for higher nervous activity.
The work of the gland and its participation in the regulation of various processes in the body continues throughout life, but in childhood it is especially important. Lack of hormones leads to delayed physical and mental development, delayed puberty, deterioration of metabolism and thermoregulation.
Symptoms
There are a number of symptoms that may indicate pathology in a child even before birth or in the first hours of life:
- prematurity or post-term pregnancy;
- genetic predisposition;
- enlarged fontanel;
- birth of a large fetus (more than 4 kg).
Other symptoms begin to appear gradually:
- jaundice;
- with late passage of meconium in a newborn (first feces);
- frequent constipation and severe gas formation;
- hyporeflexia;
- incomplete fusion of cranial bones;
- Muscle weakness and apathy may occur.
By 3-6 months of life, a newborn with hypothyroidism may experience:
- dry skin;
- skin color may be jaundiced-gray;
- changes occur in the voice, it may be low with hoarseness;
- delays in mental and physical development.
In some cases, congenital hypothyroidism may not appear until the age of six.
Hypothyroidism in newborns
13.09.2019
Thyroid examination is one of the screening tests for newborns. An examination of the thyroid gland can detect endocrine gland disorders, such as, for example, congenital hypothyroidism . According to scientific research, girls with thyroid suffer twenty times more often than boys. The thyroid gland is the largest endocrine gland in the human body. In children it weighs about 4–15 g, while in adults it weighs 15–30 g. The thyroid gland produces hormones that control body temperature and metabolic processes. Proper functioning of the thyroid gland affects the nervous, digestive and reproductive systems. In infants, thyroid affect the slowdown of the child’s development and growth and the formation of the skeletal system.
Hypothyroidism in a newborn
If the thyroid gland produces too little hormone relative to the body's needs, it is called hypothyroidism . Hypothyroidism can be caused by abnormal hormone or abnormal development of the thyroid gland . In children, congenital hypothyroidism is the most common. In this case, thyroid gland is not able to produce enough hormones . Congenital hypothyroidism is not always diagnosed during pregnancy because the deficiency of fetal hormones hormones produced by thyroid gland . In some cases, hypothyroidism in children is caused by an underactive thyroid gland , which is manifested by physical problems such as a widening of the tongue.
The main symptoms of congenital hypothyroidism in newborns are:
- prolonged jaundice of newborns;
- slow intestinal motility and frequent constipation and abdominal ;
- long sleep time for the newborn and low activity of the child;
- lack of appetite;
- newborn crying;
- decreased muscle tone.
Hypothyroidism in children can manifest itself as delayed growth of teeth and bones , while hypothyroidism in adolescence mainly manifests as delayed puberty and learning problems. Hypothyroidism in newborns most often occurs as a result of genetic disorders or hormone in the mother. In older children, thyroid can be caused by a lack of iodine or medications. Congenital deficiency thyroid hormones in a child can lead to mental retardation and dwarfism because the thyroid gland is responsible for the proper development of tissues, especially bone tissue. Hypothyroidism , which occurs in a child over two years of age, usually develops without signs indicating mental retardation. However, growth retardation and learning problems are common.
Diagnosis of hypothyroidism in newborns
Diagnosis of hypothyroidism in newborns is based on clinical symptoms and blood tests by a specialist on the third day of life, which determine the level of TSH (thyrotropin - pituitary hormone that stimulates the thyroid hormone to hormonal activity). A high TSH level usually indicates hypothyroidism . The TSH standard for newborns is below 15 mU/L on the fourth day after birth . In newborns, the concentration of TSH is significantly increased until the fourth day after birth, which is a completely natural phenomenon. Hashimoto's disease may cause congenital hypothyroidism due to abnormalities in the immune system . immune system attacks the thyroid gland , resulting in disruption of the production thyroid hormones .
Neonatal screening for thyroid is carried out in neonatal units. However, making a diagnosis is not easy. If a mother notices alarming changes in her child after leaving the hospital , she should inform the doctor . Alarm should be caused by symptoms such as pale and dry skin, low mobility of the child, drowsiness, frequent constipation and difficulty passing stool, slow growth. These are symptoms that may indicate hypothyroidism in a child. Treatment of hypothyroidism in children involves the administration of appropriate replacement medications that complement the deficiency thyroid hormones . Early diagnosis of the disease and treatment ensure the child’s normal psychophysical development.
Published in Endocrinology Premium Clinic
Diagnostics
In the first weeks of life, it is very difficult to diagnose congenital hypothyroidism and this is possible only in 10-15% of cases, so doctors need to focus mainly on the existing symptoms, which were voiced in the article above. If symptoms exist in the first months and years of life, a number of studies are carried out that will be aimed at identifying the disease:
- routine examinations by a pediatrician, and before the child reaches the age of one month – by a neonatologist;
- taking a general and biochemical blood test to determine the concentration of thyroid hormones, cholesterol and other important indicators;
- monitoring the child’s pulse and blood pressure, since with hypothyroidism in children these indicators will be reduced;
- conducting an ECG, which may show bradycardia and other abnormalities;
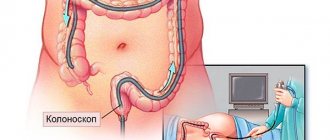
- ultrasound examination of the thyroid gland, which can reveal both some deviations from the norm and the complete absence of the thyroid gland;
- in some cases, a CT or MRI of the baby’s head may be prescribed.
Diagnosis of hypothyroidism
A pediatric endocrinologist diagnoses hypothyroidism in children. The examination is aimed at timely detection of hormone deficiency, determining the form and cause of the disease. All newborn babies are required to have their thyroid-stimulating hormone (TSH) levels checked on days 4-5 of life. If it is in excess, a preliminary diagnosis of hypothyroidism is made.
An extensive laboratory examination includes determination of the level of hormones T3, T4, thyreglobulin, hormone binding index, detection of antibodies to thyroid hormones, and a test with thyrotropin-releasing hormone to assess the functioning of the pituitary gland.
In addition to tests, other diagnostic procedures are used: ultrasound and scintigraphy of the thyroid gland, determination of bone age (by x-ray of the knee joints, feet, hands), MRI or CT of the sella turcica, heart examinations (ECG, ultrasound) in the presence of related problems. If necessary, the child is referred for consultations to specialized specialists: ophthalmologist, neurosurgeon, neurologist, cardiologist, hematologist, etc.
Treatment of congenital hypothyroidism
For treatment to be effective, it must begin immediately after diagnosis.
Usually, the child is immediately prescribed synthetic thyroid hormones - L thyroxine. The amount of this substance is selected individually, depending on the child’s weight and other parameters.
The effectiveness of drug therapy is assessed by the content of thyroid hormones in the child’s blood (TSH and T4), as well as the disappearance or presence of symptoms.
Sometimes, if necessary or to achieve greater effectiveness of treatment, additional vitamin complexes or drugs are prescribed to reduce the symptoms of hypothyroidism.
Hypothyroidism - symptoms and treatment
The goal of treatment for hypothyroidism is to maintain TSH levels between 0.5 and 1.5 mIU/L.
The only treatment method is lifelong replacement therapy. It should be started when the TSH level is more than 10 mU/l, high titers of antibodies to TPO and other indicators. For this purpose, levothyroxine sodium preparations are preferred. Its use is contraindicated only in cases of untreated thyrotoxicosis and adrenal insufficiency, acute myocardial infarction, allergies and individual intolerance to the drug.[16]
Treatment is usually carried out in a hospital setting. Indications for hospitalization of patients with hypothyroidism are:
- severe disease;
- the presence of severe cardiac pathology;
- hypothyroid coma.
Replacement therapy for primary (manifest) hypothyroidism is indicated for life with the administration of thyroxine at an average dose of 1.6-1.8 mcg/kg. For patients with cardiac pathology, the dose is calculated based on the calculation of 0.9 mcg/kg. It is worth noting that due to a decrease in the metabolism of thyroid hormones, the need for them decreases with age.[5][7][9]
Doses of thyroxine depend on the causes and pathogenesis of the disease. The need for the drug in people with spontaneous hypothyroidism is higher than in patients with hypothyroidism that occurs after surgical treatment and the use of radioactive iodine.
The TSH level when diagnosing hypothyroidism is directly related to the optimal replacement dose of thyroxine: for most women it is 75-100 mcg, and for men - up to 150 mcg per day of administration.
The first control of TSH levels after the start of treatment is carried out after 2-3 months, then once every six months (provided the patient complies with the treatment regimen).[6][9][13]
With subclinical hypothyroidism, there is a risk of developing a manifest form of the disease with all the characteristic manifestations. Thus, overt hypothyroidism occurs in 20-50% of patients within 4-8 years, and the presence of antithyroid antibodies increases the risk to 80%.[8][9][10] Therefore, people with hidden hypothyroidism should be monitored by specialists for a long time.
Problems in treating hypothyroidism
Treatment with thyroxine is safe, simple and relatively cheap. But, despite many years of experience in its use, many problems can still arise with it. The main one is related to the patient’s non-compliance with the treatment regimen. Thus, a simultaneous increase in T4 and TSH levels will most likely indicate that the patient did not follow the doctor’s orders several days before the doctor’s visit.
Decreased effectiveness of the prescribed dose of thyroxine is often due to lower levels of the hormone in the tablets (eg, generic drugs) or drug interactions when other drugs are taken concomitantly.[9][13]
Insufficient dosage may also be associated with decreased absorption of thyroxine, impaired enterohepatic blood flow, accelerated circulation or excretion of the hormone in the urine, or a slow decrease in thyroid function after treatment of hyperthyroidism.
There are other considerations and challenges in treating hypothyroidism.[6]
| Factors | Features and possible problems |
| Drug interactions due to concomitant use of drugs | Decreased absorption of thyroxine |
| Acceleration of thyroxine metabolism | |
| Decreased levels of thyroxine-binding globulin | |
| Heart diseases | Worsening of baseline coronary heart disease |
| Angina pectoris | |
| Bone Mineral Density | Harmful effects on the skeleton due to thyroxine overdose |
| Pregnancy | Thyroxine dose may need to be increased |
| Hypothyroidism in old age | Difficulty in diagnosis |
| Smaller initial replacement doses of thyroxine | |
| Transient hypothyroidism | Some recommend temporary administration of thyroxine |
| Careful follow-up studies are required | |
| Myxedema coma | Difficulty in selecting doses of thyroxine or triiodothyronine |
| Adrenal insufficiency | Combination of adrenal and thyroid insufficiency |
| Decreased TSH levels when treated with corticosteroids alone | |
| The need to prescribe thyroxine and corticosteroids in some cases of pituitary hypothyroidism | |
| Pre- or postoperative period | There is no need to compensate for hypothyroidism before the upcoming surgery |
| Hypothyroidism may increase sensitivity to usual doses of anesthetics and sedatives | |
| Lung diseases | The connection between hypothyroidism and sleep apnea (stopping breathing) |
| Worsening of asthma during treatment with thyroxine | |
| Mental illness | The connection between hypothyroidism and mental illness |
| Possible remission with thyroxine treatment |
The best criterion for selecting the dose of thyroxine for autoimmune thyroiditis is the study of TSH and free T4. In this case, treatment is aimed at compensating for hypothyroidism thanks to the same replacement therapy and reducing goiter using suppressive therapy.[6][9] The criteria for the effectiveness of treatment will be:
- reduction of goiter in volume;
- decreased thyroid density;
- decrease in antibody titer to normal;
- maintaining TSH levels within normal limits.
Prescribing thyroid hormone drugs for autoimmune thyroiditis without dysfunction of the thyroid gland is inappropriate, and surgery can lead to a condition that can significantly worsen the patient’s quality of life with the possibility of developing severe hypothyroidism and disability.[9][13]
Forecast
If the pathology is detected early, the consequences of congenital hypothyroidism will not be detrimental to the patient’s health, but are assessed by doctors as favorable.
With proper therapy, bringing the main thyroid hormones to normal levels, we can say that nothing will hinder the child’s development (taking into account the fact that hormone replacement therapy will be lifelong).
If congenital hypothyroidism is detected not in the first months of life, but at 3-6, then the chances of complete normalization of the condition are significantly reduced, even with proper treatment. At the same time, it is possible to achieve the required level of psychophysical development of the child, but there is a high probability of lagging behind in intellectual development.
Which doctor will help?
The treatment of congenital hypothyroidism in children is carried out by an endocrinologist together with a pediatrician.
I, Georgy Nikitich Romanov, am a qualified and experienced endocrinologist. My medical practice spans more than 20 years, during which time I have encountered various cases, including a disease such as congenital hypothyroidism, with which we successfully worked.
I acquired my skills not only at universities in our country, but also abroad (I completed internships in the UK, Germany, and Russia). The skills and experience I have gained help me accurately prescribe treatments for my patients.
At the moment, I am conducting face-to-face appointments at the Amadeus Clinic medical center in Gomel and conducting paid online consultations. As part of an online consultation, I can evaluate diagnostic results, treatment progress, adjust treatment, and more.
To sign up for a consultation, write to me in one of the suggested messengers: Viber, Skype, Instagram, VKontakte, WhatsApp.