Quick Jump How to Treat Colon Cancer
Colorectal cancer is cancer of the colon , which is the final part of the gastrointestinal tract and includes the colon, sigmoid and rectum.
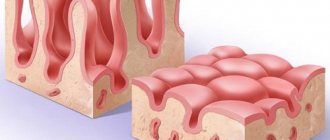
Most cases of colon cancer begin as small, benign tumors called adenomatous polyps and adenomas. Over time, some of these polyps can develop into malignant tumors and become colon cancer.
Polyps may cause no symptoms or symptoms may be subtle. For this reason, doctors recommend regular screening tests to prevent colon cancer by identifying and removing polyps before they turn into cancer.
What are the symptoms of colon cancer?
Signs of colon cancer include:
- Changes in bowel habits, including diarrhea or constipation, or changes in stool consistency that last more than four weeks.
- Passage of blood or blood in the stool.
- Constant discomfort in the abdomen, such as bloating, variable pain.
- Feeling of intestines not being completely emptied.
- General weakness, fatigue.
- Unexplained weight loss.
In the early stages of colon cancer, many people do not experience symptoms. When symptoms appear, they usually vary depending on the size of the tumor and its location in the colon.
Symptoms
If a person's intestine is affected by cancer, the initial symptoms may not be noticeable and do not necessarily cause illness. Often, the initial forms of the lesion are determined during screening or during examinations for other reasons.
More than 90% of people with bowel cancer have 1 of the following combinations of symptoms:
- persistent changes in bowel function;
- more frequent urination, loose stools, and sometimes abdominal pain;
- blood in the stool without other rectal symptoms (when hemorrhoids or anal fissures are unlikely to be the cause);
- Abdominal pain, discomfort or bloating is always caused by food, which sometimes leads to a decrease in the amount of food eaten and weight loss;
- Constipation, rarely hard stools, is rarely caused by serious intestinal diseases.
It is important to see a doctor if a person has 1 or more symptoms of bowel cancer that persist for more than 4 weeks.
Rare bowel cancer syndromes are intestinal obstruction or intussusception. In some cases, bowel cancer can stop digestive waste from passing through the intestines. Symptoms of intestinal obstruction may include:
- periodic and sometimes severe abdominal pain that does not go away;
- unintentional weight loss with constant abdominal pain and swelling, bloating;
- lack of stool and passing gas, increasing general malaise.
Intestinal obstruction is a medical emergency. Without surgery or other urgent measures, this threatens death.
When should you see a doctor?
If you notice any symptoms of colon cancer, such as blood in your stool or persistent bowel discomfort, don't hesitate to make an appointment with your doctor.
The Rassvet clinic has a multidisciplinary team of highly qualified specialists - gastroenterologists, therapists, nutritionists, to whom you can turn for help.
The doctor will first examine the more common causes of these signs and symptoms, and if a tumor process is identified, he will refer you for a consultation with an oncologist at the Rassvet Clinic.
You can also find out when you should start screening for colon cancer. As a rule, it is recommended to start it after the age of 50 years. But your doctor may recommend more frequent or earlier screening if you have risk factors.
What are the causes of colon cancer?
In most cases, it is not conclusively determined what exactly causes colon cancer. Doctors know that it occurs when healthy colon cells have errors in their genetic code - DNA.
Healthy cells grow and divide in ways that keep the body functioning normally. But when a cell's DNA is damaged and the cell becomes cancerous, it continues to divide even if new cells are not needed. The immune system normally identifies and destroys such cells, but over time, cancer cells acquire the ability to evade the immune system. This is how a malignant tumor is formed.
Over time, the number of cancer cells grows, they penetrate into nearby tissues and destroy them. Cancer cells can also move to other parts of the body. This is called metastasis.
Hereditary colon cancer
Inherited gene mutations that increase the risk of colon cancer can run in families, but these inherited gene changes are associated with only a small percentage of colon cancer cases.
Inherited gene mutations do not always necessarily lead to cancer, but can significantly increase the risk of the disease.
The most common hereditary cancer syndromes associated with colon cancer are:
- Family adenomatous polyposis (FAP). FAP is a rare disease that causes thousands of polyps to form in the lining of the colon and rectum. With this disease, the patient has an almost 100% chance of developing colon cancer by age 40.
- Hereditary nonpolyposis colorectal cancer (HNPCC), also called Lynch syndrome. This is a genetic disease associated with a high risk of developing colon cancer, as well as other cancers, including endometrial cancer, ovarian cancer, stomach cancer, small intestinal cancer, liver cancer, urinary tract cancer, brain tumors and skin tumors. The increased risk of developing these cancers is due to inherited mutations that impair the repair of DNA damage.
Patients with Lynch syndrome have a 50-70% risk of developing colon cancer during their lifetime.
FAP, Lynch syndrome, and other rarer hereditary colon cancer syndromes can be detected through genetic testing. If you are concerned about a history of colon cancer in your family and want to find out how high your risk of developing colon cancer is, schedule a consultation with an oncologist at the Rassvet Clinic.
The doctor will determine the necessary examination program to determine the degree of risk and tell you about cancer prevention methods in your case.
Link between diet and increased risk of colon cancer
Studies of large groups of people have shown an association between a typical “Western” diet and an increased risk of colon cancer. The typical “Western” diet is high in fat and low in fiber.
When people move from areas with a low-fat, high-fiber diet to areas with a typical "Western" diet, their risk of developing colon cancer increases significantly. This is due to the effect of a high-fat, low-fiber diet on the bacteria that normally live in the colon and the maintenance of chronic inflammation, which contributes to cancer. Currently, this topic is the subject of active research.
Also, the risk of developing colon cancer increases the increased consumption of red meat and processed meat products.
What are the risk factors for colon cancer?
Factors that may increase your risk of developing colon cancer include:
- Elderly age. The vast majority of colon cancer cases occur in people over 50 years of age. This disease can also occur in young people, but much less frequently.
- African American race. African Americans have a greater risk of colon cancer than other races.
- History of colon cancer. If you have already had colon cancer or an adenomatous polyp, you have an increased risk of developing colon cancer in the future.
- Inflammatory bowel diseases. Chronic inflammatory diseases of the colon, such as ulcerative colitis or Crohn's disease, may increase the risk of developing colon cancer.
- Hereditary syndromes. Genetic syndromes that are passed down from generation to generation can increase the risk of colon cancer. These syndromes include familial adenomatous polyposis and hereditary colon cancer without polyposis, which is also known as Lynch syndrome.
- Family history of colon cancer. You are more likely to develop this disease if you have parents, siblings, or a child with the disease.
- A low fiber, high fat diet.
- Sedentary lifestyle. People with low physical activity have an increased risk of developing colon cancer. Regular physical activity can reduce your risk of developing it.
- Diabetes. People with diabetes and insulin resistance have an increased risk of developing colon cancer.
- Obesity. People who are obese have an increased risk of developing and dying from colon cancer compared to people whose weight is normal.
- Smoking. People who smoke have an increased risk of developing colon cancer.
- Alcohol. Excessive alcohol consumption increases the risk of developing this cancer.
- Radiation therapy. People who have had radiation therapy to the abdomen or pelvis for another cancer have an increased risk of developing colon cancer.
Prevention of colon cancer. Screening
Screening plays a vital role in the prevention of colon cancer.
Doctors recommend certain screening tests for healthy people without signs or symptoms of disease to detect colon cancer at an early stage.
Finding colon cancer at its earliest stage offers the best chance of cure. Screening has been shown to reduce the risk of death from the disease.
According to American Cancer Society guidelines, routine colon cancer screening should begin between ages 45 and 50. This can be done either by testing for occult blood in the stool, or by examining the colon during an endoscopic procedure, called colonoscopy, or the lower parts of the colon, called rectosigmoidoscopy. It is also possible to conduct CT colonography - this is a study using computed tomography.
People in good health should be screened regularly for colon cancer before age 75.
For people aged 76–85 years, the decision to get screened is an individual decision made with your doctor and should be based on preference, life expectancy, general health and previous screening history.
Colon cancer screening is not recommended for people over 85 years of age.
The following types of colon cancer screening are distinguished:
- Colonoscopy. Usually performed once every 10 years in the absence of signs of pathology.
- CT colonography. Conducted every 5 years.
Another screening option is an annual stool occult blood test in combination with rectosigmoidoscopy every 5 years.
Each method has its own advantages and disadvantages. Talk to your doctor and together you can decide which tests are right for you. If colonoscopy is used for screening, polyps can be removed during the procedure before they turn into cancer.
The most important thing is to get screened. At the Rassvet Clinic, you can get advice from an oncologist about the types of examinations for colon cancer screening and decide which method is right for you.
People at increased risk for colorectal cancer may need to be individualized because they may need to start screening before age 45, have more frequent screenings, and/or undergo special tests.
The risk of colon cancer is increased if:
- There is a family history of colon cancer or certain types of polyps.
- Treatment of colon cancer or certain types of polyps in the gap.
- Have inflammatory bowel disease (ulcerative colitis or Crohn's disease).
- Known family history of hereditary colorectal cancer, such as familial adenomatosis (FAP) or Lynch syndrome.
- Previous radiation therapy was given to the abdomen or pelvis to treat another cancer.
- One or more family members have colon cancer.
- People who have had certain types of polyps removed during a colonoscopy.
If you have an increased risk of colon cancer, you can consult with specialists at the Rassvet Clinic and receive an individual screening program that is necessary in your case.
Advice from doctors at the Rassvet clinic on lifestyle changes to reduce the risk of colon cancer
You can take steps to reduce your risk of colon cancer by making changes to your daily life. To do this you need:
- Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants that may play an important role in cancer prevention. Choose a variety of fruits and vegetables to get a variety of vitamins and nutrients.
- Drink alcohol in moderation, or don't drink at all. If you drink alcohol, limit the amount you drink to no more than one drink per day for women and two for men.
- Stop smoking. Quitting smoking on your own can be very difficult; you can contact the doctors at the Rassvet Clinic. You will be given practical advice and information about available medications to help you quit smoking.
- Be physically active as many days a week as possible. Try to exercise for at least 30 minutes as often as possible. If you have been inactive, start gradually and build up to 30 minutes.
- Maintain a normal weight. To maintain your weight, combine a healthy diet with daily exercise. If you need to lose weight, at the Dawn Clinic you can get advice from a nutritionist about healthy ways to achieve your goal. Aim to lose weight slowly by increasing the amount of exercise you do and decreasing the number of calories you eat.
Diagnostic methods
Fortunately, bowel cancer can be detected early. Genetic tests are used for this. They allow you to confirm or refute the presence of gene mutations in cells. And if colorectal cancer does develop, the patient will know about it earlier and, therefore, will have a chance for a full recovery.
What screenings for colorectal cancer should be performed in patients who have warning signs?
- blood tests (general, biochemistry, CEA);
- stool occult blood test;
- examination of the rectum (through the anus);
- Colonoscopy - an alternative to stool occult blood testing (examination with a camera inserted into the intestines through the anus) - every 10 years as a preventive measure in all men and women over 50 years of age. In patients over 65 years of age, the frequency of colonoscopy depends on the individual decision of the physician;
- rectoscopy (examination of the final section of the rectum about 30 cm long through a special mirror);
- virtual colonoscopy, that is, colonography (study of a three-dimensional image of the intestine using images obtained using a computed tomograph);
- biopsy - taking a tissue sample to study the degree of malignancy of the tumor;
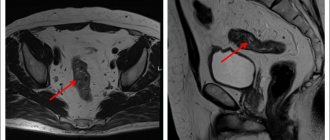
- PET/CT/MRI - helps determine the location and size of the tumor.
- determination of the concentration of marker 5 CEA in the blood.
Colonoscopy and stool occult blood testing are preventive tests recommended for early detection of the disease. They are usually performed on people without symptoms.
Rectoscopy, examination of tumor markers for intestinal cancer, virtual colonoscopy and a number of other additional diagnostic tests useful for making a diagnosis are performed as part of an in-depth diagnosis of patients, whose attending physician decides on the need for them based on the medical history and the results of previous examinations.
All of the above studies can lead to a diagnosis, but do not give a clear answer as to whether it is colorectal cancer. A definite diagnosis can only be made by histopathological examination, that is, taking a sample of the affected tissue, such as a tumor or polyp, and analyzing it.
Diagnosis of colon cancer
If your symptoms indicate that you may have colon cancer, you need further testing. To do this, use the following procedures:
Endoscopic diagnostics:
1. Colonoscopy. During colonoscopy, a special instrument (colonoscope) is used, which is a long, flexible and thin tube combined with a video camera and monitor. Thus, the doctor examines the mucous membrane of the entire colon.
If suspicious tissue or polyps are found, he passes surgical instruments through the colonoscope and takes tissue samples (biopsies) or removes the polyps. At the Rassvet clinic, the procedure is performed under general anesthesia, which makes it painless and avoids discomfort during the examination.
A tissue biopsy is extremely important, as the tissue is subjected to modern pathomorphological diagnostics, with histological, immunohistochemical and molecular genetic studies, this allows not only to make a diagnosis, but also to correctly prescribe treatment.
Once a diagnosis of colon cancer is made, examinations are ordered to determine the extent of its prevalence. Correct determination of the extent of the tumor process (stage) is necessary to select the most appropriate treatment protocol.
These tests include imaging procedures such as CT scans of the abdomen and chest.
2. Magnetic resonance imaging of the pelvic organs. The final scope of the examination is determined by the doctor, based on complaints and the clinical picture of the disease.
3. Clinical blood tests are also performed. A blood test cannot detect colon cancer. But your doctor can test your blood to look for signs of general health problems.
A blood test is performed to look for tumor markers—chemicals sometimes produced by colon cancer cells (carcinoembryonic antigen CA19-9, or CEA). The level of tumor markers monitored over time can also help the doctor assess the prognosis of the disease and understand whether your cancer is responding to treatment.
In some cases, the stage of the tumor can only be determined after surgery to remove colon cancer.
Colon cancer stages
There are 4 stages of this disease:
- Stage I. The cancer spreads within the wall of the colon, but does not spread beyond the wall or rectum.
- Stage II. Cancer grows through the entire thickness of the colon wall and can invade adjacent tissue, but does not spread to nearby lymph nodes.
- Stage III. The cancer spreads to nearby lymph nodes but does not affect other parts of the body.
- Stage IV. The cancer spreads to distant organs, such as the liver or lungs.
Treatment survival statistics
The prognosis for bowel cancer depends on a number of factors, so it is impossible to predict the success of therapy with certainty. Unfortunately, 80% of patients with colorectal cancer are diagnosed with advanced stage disease. About 40% of cases are inoperable. There is no cure for them, and the only thing patients can count on is relief of symptoms and slowing down the progression of the disease.
What about the other 60% of patients? If the disease is diagnosed at stage I, the 5-year survival rate reaches 90%. This does not mean that the patient will live only 5 years. On the contrary, it means that the disease is under control and the risk of cancer recurrence after 5 years is low.
If colorectal cancer is detected at the last stage, when metastases have already appeared in other organs and their removal is impossible, the 5-year survival rate is only 7%. If metastases are surgically removed - 25-35%. The average survival rate of patients with colorectal cancer is 40%.
IMPORTANT:
Most often, cancer metastases affect the liver through the blood and lymphatic vessels, less often the lungs, ovaries, adrenal glands, brain and bones.
How to treat colon cancer
In the treatment of colon cancer, as with most other malignant tumors, surgery, chemotherapy, radiation therapy and their combinations are used. The need and sequence of each of these stages is determined taking into account the prevalence of the process, as well as the patient’s condition and identified concomitant diseases.
At the Rassvet clinic, a multidisciplinary approach is used to treat malignant tumors of the colon, with complex cases discussed at a consultation involving a surgeon, chemotherapy and radiotherapist.
The Rassvet clinic has everything necessary for chemotherapy for colon cancer according to Russian and Western protocols, as well as accompanying therapy. If necessary, the patient is routed to other treatment methods.
Treatment methods
The main treatment method for rectal cancer is surgery (removal of the malignant tumor). Surgery may be preceded by radiation therapy. The malignant tumor is excised along with the surrounding healthy portion of the intestine and, most often, the surrounding lymph nodes.
If possible, the remaining sections of the intestine are stitched together. However, it may be that suturing is impossible, then an artificial anus is formed, that is, a stoma is an opening in the abdominal wall into which the end of the large intestine is placed. Outside the opening there is a plastic container into which feces fall. For some patients, this condition can cause a decrease in quality of life, but the stoma may allow you to function normally for several years. In some cases, removal of the so-called artificial anus is necessary for life, but sometimes only until the intestinal anastomosis heals.
If the diagnosis of colorectal cancer is confirmed, surgery on multiple organs may be required. Not only a fragment of the intestine is cut out, but also other organs affected by cancer, for example, a fragment of the liver, stomach, kidneys, abdominal wall or ovary.
Additional radiation and chemotherapy may be required after surgery. Postoperative rehabilitation is required.