Diseases of the small intestine
The final process of food digestion occurs in the small intestine, followed by the absorption of digestive substances, vitamins and minerals. Various diseases of the small intestine manifest themselves in the same way. Most often, our doctor in this case diagnoses “poor absorption syndrome.”
Manifestations of the disease that you may notice in yourself
Diseases of the small intestine usually manifest themselves:
- stool disorders
- rumbling and bloating
- pain.
The most common manifestation is diarrhea 3-6 times a day. Pain occurs in the navel area, sometimes in the epigastric region or the right half of the abdomen. They are most often pulling, aching, bursting and decrease after the passage of gas. There may be intestinal colic: very severe pain with intestinal spasms.
Small intestine: briefly about diseases
Chronic enteritis is inflammation of the small intestine. The causative agents of acute intestinal diseases play a primary role in its occurrence. Enteritis itself is often a post-infectious process. Vascular diseases : abdominal pain that occurs after eating, stool disorders. Timely contact with a professional is very important, since complete blockage of blood vessels may occur. Allergies manifested by intestinal disorders. Celiac enteropathy : deficiency of the enzyme peptidase, which breaks down gluten, a protein ingredient in grain plants; The disease manifests itself as severe diarrhea and weight loss. A rare Whipple's disease , characterized by severe diarrhea, fever, cramping abdominal pain, weight loss, and enlarged lymph nodes. Tumors are mostly benign.
Colon diseases
Colon diseases are:
- ulcerative colitis
- ischemic colitis
- Crohn's disease
- irritable colon
- dolichosigma, megacolon
- diverticulosis
- colon tumors.
Symptoms you may notice
- stool disorders
- stomach ache
- pathological discharge
- rumbling and bloating.
Stool disorders: constipation is more common. Pain in the anus, sides of the abdomen, above the navel or in the epigastric region. The pain is cramping or aching, bursting and is usually not associated with eating. They weaken after bowel movements and the passage of gases.
Large intestine: briefly about diseases
Ulcerative colitis affects the mucous membrane. Dangerous due to the possible development of polyps and tumors. Irritable colon is a complex of intestinal disorders due to disruption of intestinal motility. Crohn's disease : the entire intestine, esophagus, and stomach are affected. With ischemic colitis, inflammation occurs due to narrowing of the vessels that nourish the intestinal walls. Diverticulosis means the presence of multiple diverticula (ending in blind pouch-like protrusions of limited areas of the intestine) and leads to constipation. Dolichosigma - elongation of the sigmoid colon; megacolon - expansion of individual zones or the entire colon. Both diseases cause persistent constipation. Of benign and malignant neoplasms, the latter are more common. Now colon and rectal cancer is the most common malignant tumor.
Colon diseases
09.10.2021
The large intestine is the final section of the digestive system. It is in it that food is digested, all necessary vitamins and microelements are absorbed, as well as feces are excreted.
But, just like any human organ and any system, the colon is susceptible to various kinds of diseases. Therefore, pain in the rectum is not a rare occurrence. Impaired motor skills , inflammation, the appearance of tumors, problems with absorption and digestion - all this negatively affects the health and general condition of a person.
About the general signs of diseases of the rectum
As a rule, most problems associated with the intestines are practically asymptomatic. With the progress of a particular disease, so-called intestinal discomfort appears, which over time becomes unbearable.
Common signs of colon disease include:
- Disturbed stool: constipation, diarrhea
- Stool instability
- Painful sensations in the epigastric region
- The appearance of rumbling sounds in the stomach
- Bloating, gas
In addition to all of the above symptoms, a person may complain of purulent and bloody discharge. False urge or tenesmus and gas become commonplace.
The most common diseases of the large intestine
Regional enteritis
A chronic inflammatory disease characterized by damage to the entire intestine, stomach and esophagus . Inflammatory changes can be either single or multiple. As a rule, they spread throughout the entire intestine. A characteristic sign of Crohn's disease is a narrowing of the intestinal lumen. Accumulation of granuloma cells and damage to lymph nodes are observed in almost all patients. Symptoms depend on the area affected by the disease. When changes occur in the right side, there are complaints of pain, frequent diarrhea, bloating and rumbling. When a narrowing of the intestine occurs, intestinal , which is characterized by unbearable pain and vomiting.
Complications of this disease include:
- The appearance of pustular tracts (fistulas)
- Fever
- The appearance of a rash on the skin
- Damage to the liver , eyes and joints
Neoplasms in the colon
A tumor in the large intestine can be benign or malignant. The most common causes of tumors are:
- a diet that includes large amounts of refined foods and animal fats
- intestinal polyps
- hereditary polyposis
- ulcerative colitis
Detecting cancer at an early stage is impossible, since pain in the abdomen , increased constipation, and spotting are symptoms that are characteristic of many diseases. And therefore, diagnosis and detection of a tumor can drag on for quite a long period.
Colon diverticulosis
The disease is characterized by the appearance of small diverticula in the walls of the rectum . Most often, elderly and old people suffer from this disease. The sigmoid and descending colon are the most common sites of diverticulum formation. Typically, they appear due to increased pressure inside the colon cavity, and the most common cause is constipation. This disease, in principle, has no characteristic symptoms. The symptoms are quite similar to other diseases of the large intestine .
In any case, your main task is to contact a specialist at the first suspicious symptoms and undergo an examination. You must understand that you should not joke or delay with the listed diseases.
Published in Gastroentorology Premium Clinic
Diagnostics
Difficulties in diagnosing diseases of the small intestine are explained by the peculiarities of its location. Analysis of the clinical picture, histological, endoscopic, and immunological methods are of decisive importance.
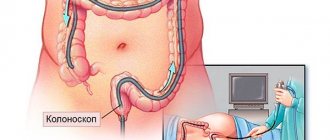
Almost all diseases of the colon are detected by fiber colonoscopy (flexible fiber colonoscopes with fiber optics are used). The examination also includes:
- study using contrast agents
- angiography
- fistulography
- lymphography
- parietography
- ultrasound
- research using radioactive isotopes.
Pathology of the colon: from functional to organic
I.G. PAKHOMOV
, Candidate of Medical Sciences,
North-Western State Medical University named after. I.I. Mechnikov The relevance of diseases of the colon, differential diagnostic features of functional and organic intestinal pathology, diagnostic algorithms are considered.
At the present stage of development of new technologies and progress in many areas of medicine, there is a tendency towards an increase in a number of diseases of the gastrointestinal tract (GIT), including pathology of the colon. There are many reasons for this, despite active propaganda in the media and education of the population in maintaining a healthy lifestyle: this is a sedentary, sedentary lifestyle, and the nutritional habits of modern people, the influence of environmental changes, etc. The widespread prevalence of colitis of various origins among the population, diverticular disease, hemorrhoids, proctitis and other pathologies of the colon remains a serious problem for many specialists - therapists, gastroenterologists, surgeons, infectious disease specialists, etc. In clinical practice, diseases of this kind, as well as functional disorders of the colon, occur almost every day. The role of the colon in digestion
Despite the fact that the large intestine is the final stage in the digestive process, its role is no less significant compared to other parts of the gastrointestinal tract. As you know, food is almost completely digested and absorbed in the small intestine. At the same time, a small amount of nutrients, including fiber and pectin, in the composition of food chyme are hydrolyzed in the colon by enzymes of chyme, microorganisms and intestinal juice (cathepsin, peptidase, lipase, amylase and nuclease).
After absorbing water (up to 4–6 liters per day), chyme gradually turns into feces (150–250 g of formed feces are excreted per day), the volume of which depends on the composition of the food consumed. If foods are rich in fiber, pectin, lignin, cellulose, the amount of feces increases, the movement of chyme accelerates, which prevents the development of constipation and their corresponding consequences.
The functions of the large intestine are diverse, the main ones being: motor, transport and excretory, thereby ensuring the formation and evacuation of feces. Complete bowel emptying occurs within 48–72 hours.
Functional disorders of the colon
Functional pathology of the colon is one of the most common diseases of the gastrointestinal tract and constitutes the largest group of requests at the outpatient stage of medical care. Only in a small number of patients these disorders can take a persistent, long-term course and require hospital treatment.
The main types of functional bowel disorders include [1]:
1. Motor disorders: a) hypermotor (increased tone, accelerated propulsion), b) hypomotor (decreased tone, slow propulsion). 2. Transport disorders: a) hypersecretion of ions and water into the intestinal lumen, b) increased absorption of ions and water in the colon. 3. Mucus secretion disorders: a) excessive mucus secretion, b) reduced mucus secretion.
According to the recommendations of the Rome III Consensus (2006), functional intestinal disorders include [2]:
• irritable bowel syndrome (IBS); • functional constipation; • functional diarrhea; • functional flatulence; • functional abdominal pain.
Irritable bowel syndrome (IBS) is the most common functional bowel disease (in most countries of the world, the incidence of IBS averages about 20%, ranging from 9 to 48%) [3]. The study of IBS has been carried out since the end of the 19th century, while the first diagnostic criteria for diagnosis were formulated by A. Manning in 1978, which later formed the basis for the recommendations of a group of international experts on the diagnosis and treatment of IBS: Rome criteria I (1988 g.), II (1999) and III (2006). IBS is an extremely important social pathology, since it is often diagnosed in people of young working age, significantly affects the quality of life of patients, causes economic damage to society in terms of direct costs of medical care and treatment, as well as compensation for temporary disability. According to modern concepts, IBS is a biopsychosocial functional intestinal disorder, which is based on the interaction of two main pathogenetic mechanisms: psychosocial effects and sensorimotor dysfunction, i.e. disturbances of visceral sensitivity and motor activity.
Returning to the Rome criteria, third revision (2006), the diagnosis of IBS [2] is established by the presence of recurrent abdominal pain or discomfort in the abdominal area for 3 days of each month over the past 3 months. in combination with two or more of the following:
- improvement of condition after defecation; — the onset is associated with a change in stool frequency; — the onset is associated with a change in the shape of feces.
Additional symptoms:
- pathological frequency of stool (< 3 times a week or > 3 times a day); - pathological form of stool - lumpy/hard or liquid/watery stool; - straining during defecation; - imperative urge or feeling of incomplete emptying, mucus and bloating.
It is important to emphasize that symptoms must have been present within the last 3 months. with their debut at least 6 months in advance.
The incidence of abdominal pain syndrome in IBS is quite high and amounts to 96%. The pain can be of varying intensity and is usually localized in the lower abdomen, although it can also be noted in other parts of the abdomen. It often intensifies after a diet violation, with a surge of emotions, against the background of nervous and physical fatigue, usually decreases after defecation or the passage of gases and, very importantly, does not bother you at night [4]. There are four main mechanisms for the formation of abdominal pain: visceral, parietal, radiating and psychogenic. Visceral pain occurs in the presence of pathological stimuli in the internal organs (increased pressure in a hollow organ and stretching of its walls, etc.), and is determined by the threshold of visceral sensitivity (Table 1) [4]. Somatic pain is caused by the presence of pathological processes in the parietal peritoneum and tissues.
Psychogenic pain occurs in the absence of somatic causes and is caused by a deficiency of inhibitory factors and/or an increase in normal incoming afferent signals due to damage to central control mechanisms and/or a decrease in the synthesis of biologically active substances. The pain is constant, sharply reducing the quality of life, and is not associated with impaired motor skills, food intake, intestinal motility, defecation and other physiological processes. The mental status of the patient often reveals symptoms of obsession, phobic and depressive states.
In functional intestinal disorders, the pathogenetic mechanisms of pain formation can be different and be isolated or combined: visceral genesis is often combined with radiating and/or psychogenic mechanisms. [4]. At the same time, it is important to emphasize the absence in patients of the so-called. “alarm symptoms” or “red flags” of IBS [5]:
- unmotivated decrease in body weight, onset of the disease in old age, persistence of symptoms at night (during sleep), constant intense abdominal pain as the only and main symptom, progression of the severity of symptoms, colon oncology in relatives (found out by collecting complaints and anamnesis ); - fever, changes in status (hepato-, splenomegaly) detected during physical examination; - blood in the stool, leukocytosis, anemia, increased ESR, changes in biochemical blood parameters (determined during laboratory examination).
However, it must be taken into account that “anxiety symptoms” can be combined with IBS (for example, the presence of blood in the stool due to hemorrhoids).
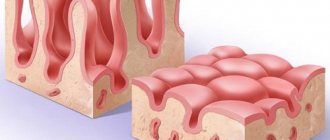
Patients with IBS and constipation complain of the absence of bowel movements for 3 or more days, while the act of defecation itself often requires straining. Unlike isolated functional constipation, IBS with constipation is characterized by prolonged, varying intensity abdominal pain, as discussed above. It is interesting to note that constipation can be replaced by daily bowel movements with the release of a meager amount of feces, which does not bring a feeling of relief and complete emptying of the intestines. In this case, the stool resembles sheep feces with the presence of mucus on its surface or takes on a ribbon-like shape (pencil-shaped stool) (Fig. 1). In some patients, constipation may be accompanied by bloating and may also alternate with diarrhea.
According to the Rome III criteria, the defining sign of constipation or diarrhea in IBS is a change in stool consistency, assessed in accordance with the Bristol scale (Fig. 1). The consistency of stool corresponding to types 1 and 2 on the Bristol scale allows us to determine the presence of constipation in the patient, while types 6 and 7 give grounds to establish the presence of diarrhea.
Functional diarrhea can be either one of the main variants of IBS or an independent nosological entity. However, as practice shows, the presence of functional diarrhea is not always recognized by practitioners. At the same time, the features of the manifestations of functional diarrhea are quite characteristic, so this disease can be suspected even after careful questioning of the patient (Table 2) [6]. In addition, a variety of clinical symptoms are revealed, extraintestinal complaints are possible (headaches, pain in the sacrum, urinary disorders, etc.) and the absence of “anxiety symptoms.”
Organic pathology of the colon. Differential diagnosis
In clinical practice, a diagnosis of “chronic colitis” has been established for a long period of time, mainly on the basis of clinical symptoms. At the present stage of development of medical technologies, the results of endoscopic and morphological studies indicate that organic diseases of the colon are much less common (despite the increasing prevalence of intestinal cancer) than functional disorders. In addition, pathology of the colon often accompanies various diseases of other digestive organs (chronic gastritis, peptic ulcer of the stomach and duodenum, etc.).
It is important to emphasize that for timely diagnosis and prescription of adequate therapy, the doctor must have a complete understanding of coloproctology, differential diagnostic criteria for a “clinical situation”, which allows us to speak either about organic pathology and the secondary nature of functional disorders, or about functional disorders of the colon.
Differential diagnosis of chronic/recurrent colonic dysfunction is carried out with the following diseases/conditions [5]:
- IBS; — Intestinal infections (bacterial, viral); - Inflammatory bowel diseases (ulcerative colitis, Crohn's disease); — Diverticular disease; — Parasitic intestinal diseases (amoebiasis, schistosomiasis, etc.); — Oncology of the colon — Proctoanal pathology (perineal prolapse syndrome, single rectal ulcer, etc.); — Psychopathological conditions (depression, anxiety syndrome, panic attacks, somatization syndrome); — Taking medications (laxatives, iron supplements, bile acids, antibiotics).
You should also exclude reasons such as:
— malabsorption syndrome (postgastroectomy, pancreatic, enteral); - pathological conditions of the central nervous system (overwork, fear, emotional stress, anxiety); — neuroendocrine tumors (carcinoid, VIPoma); — endocrine diseases (thyrotoxicosis); -functional conditions in women (premenstrual syndrome, pregnancy, menopause); - gynecological diseases (endometriosis, repeated gynecological operations); - food reactions to caffeine, alcohol and other foods.
In the presence of colonic dysfunction occurring with pain, it is necessary to collect a more detailed history from the patient and clarify the features of both the act of defecation and the nature of the stool, as well as pain manifestations. Thus, at the initial stages, organic diseases (appendicitis, diverticular disease, etc.) can be accompanied by visceral pain, then, in the case of inflammation of the peritoneum, parietal pain [7]. In addition, pain syndrome with organic damage to the colon has a number of features (Table 3).
Treatment of functional diseases of the colon, in particular correction of abdominal pain syndrome, presents significant difficulties due to mixed mechanisms. Treatment should be comprehensive, aimed at eliminating interdependent central and visceral harmful effects, normalizing motor and sensory functions (Table 4).
Psychotherapeutic influence, contact between the doctor and the patient, explanation of the causes of the disease and possible ways to eliminate it are very important. Only trust in the doctor determines the success of treatment. Pharmacological correction of psychoneurotic disorders is carried out primarily with antidepressants (A. Zlatkina, 2000; J. Wood et al., 1999). Traditionally, tricyclic antidepressants are used - amitriptyline, but recently it is giving way to new generation drugs with a serotonin reuptake mechanism. Less commonly, depending on the type of psychopathological syndrome, benzodiazepines and sulpiride are used. Amitriptyline, in addition, has a cholinolytic effect, and eglonil has a prokinetic effect.
Motility disorders in different functional diseases of the colon can occur as hypotension and atony or be of a mixed nature. In these cases, the pain is not caused by a spastic component, but by stretching the walls of a hollow organ with an increase in intraluminal pressure. The leading role in the structure of abdominal pain syndrome most often plays spastic visceral pain, which is based on involuntary contraction of intestinal smooth muscles, not accompanied by their immediate relaxation. Based on a thorough analysis of clinical data from patients with IBS, the UK National Institute for Health and Clinical Excellence (NICE) concluded that antispasmodics (Greek: spasmos - cramp, spasm) should be considered the first choice drugs for this pathology. , lyticos - liberating, relieving) - medications that eliminate spasm of the smooth muscles of internal organs. New guidelines have been released for the diagnosis and treatment of IBS in primary care [24]. Practical recommendations of the World Gastroenterological Organization (WGO Global Guideline IBS) for IBS from 2009 also name a group of antispasmodics as the main treatment for pain syndrome in this suffering. The latter, unlike analgesics, not only relieve pain as a symptom, but also weaken or completely eliminate spasm of the smooth muscles of internal organs - the direct cause of pain.
Criteria for the effectiveness of IBS therapy:
•cessation of symptoms of the disease or reduction in their intensity; •relief of pain and dyspeptic syndromes, normalization of stool and laboratory parameters (remission); •improved health without significant positive dynamics in objective data (partial remission). Considering the complex and multifactorial nature of IBS, the presence of several clinical forms of the disease, optimal treatment should be individualized and patient-oriented.
In some cases, in patients with pathology of the lumbosacral spine, radicular syndrome may occur with pain reminiscent of intestinal diseases. Diagnostic difficulties may also arise in patients with latent ulcerative colitis, when there is not only pain, increased body temperature, but also no signs of bleeding. The appearance of the latter in a patient with intestinal dysfunction almost always indicates organic damage to the intestine (Table 6) [1].
Of course, it is important to once again emphasize the fact that, in addition to the presence of “alarm symptoms,” a distinctive feature of functional intestinal disorders from organic pathology is the variety of clinical manifestations: both gastroenterological and extraintestinal, as well as the presence of psychoneurological complaints. The first appearance of signs of the disease after 50 years of age casts doubt on the diagnosis of functional intestinal pathology and requires the exclusion, first of all, of colorectal cancer. Risk groups for colon and rectal tumors are [8]:
1. Age over 50 years (the vast majority of patients with tumors of the colon and rectum are 60–70 years old or more); 2. Chronic intestinal diseases (nonspecific ulcerative colitis, colon polyposis); 3. Hereditary predisposition (familial colon polyposis, hereditary colorectal cancer); 4. Daily smoking (15–20 or more cigarettes per day)
Diagnostic search for colon pathology
The variety of genesis of lesions of the colon determines the difficulties of the diagnostic search and requires a fairly wide range of studies to clarify the nature of the pathology. The set of necessary studies should include [5, 7]:
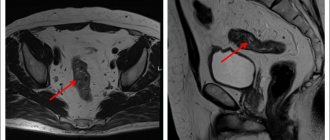
1. Laboratory tests: general blood test, general urine test, biochemical study assessing the functional state of the liver (total bilirubin, AST, ALT, alkaline phosphatase, γ-GTP), coprogram (to assess enteric or colitic syndrome), stool for dysbacteriosis, stool occult blood test. 2. Instrumental diagnostics: sigmoidoscopy, irrigoscopy (allows not only to exclude organic diseases, but also to identify some specific functional disorders: uneven haustrations, areas of spasms and atony), colonoscopy with biopsy, FGDS, ultrasound of the abdominal and pelvic organs, ECG; if necessary, angiography, laparoscopy. 3. Consultations with specialists: consultation with a gastroenterologist and/or coloproctologist; according to indications: gynecologist, urologist, psychotherapist, neurologist.
Thus, based on the above, the algorithm for diagnosing functional and organic pathology of the colon may look like this (Fig. 2). In conclusion, we note that patients with any intestinal pathology should be under constant clinical supervision of a local therapist or gastroenterologist, visiting a specialist at least once every 6 months, even if their health has not worsened since the last examination. The patient must be explained that a serious attitude towards their health, towards the existing disease, regular visits to the doctor, timely implementation of all examination recommendations and treatment recommended by the doctor can provide reliable prevention of progression and exacerbations of the disease, prevent the transition of a functional intestinal disease to an organic one (primarily in oncological). The appearance of any symptoms of deterioration or relapse of the process is an indication for immediate consultation with a doctor. Self-medication without prior examination poses a particular danger to the patient. Therefore, when managing such patients, the doctor requires skill and patience.
Literature:
1. rasstroistva-tolstoi-kishki.html 2. Drossman DA The Functional Gastrointestinal Disorders and the Rome III Process // Gastroenterology. 2006. No130 (5). R. 1377–1390. 3. Simanenkov V.I., Lutaenko E.A. Treatment of irritable bowel syndrome from the perspective of evidence-based medicine: a manual for doctors and clinical pharmacologists. St. Petersburg, 2008. 4. Shulpekova Yu. V., Ivashkin V. T. Symptom of visceral pain in pathology of the digestive organs // Doctor. 2008. No. 9. pp. 12–16. 5. Ardatskaya M.D. Irritable bowel syndrome. Clinical lecture // Gastroenterology. Consilium medicum application. 2010. No. 8. pp. 21–26. 6. Ivashkin V.T., Sheptulin A.A. Diagnosis and treatment of diarrhea in irritable bowel syndrome // RMJ. 2004. No. 1. pp. 14–19. 7. Komarov F.I., Osadchuk M.A., Osadchuk A.M. Practical gastroenterology. M.: Medical Information Agency LLC, 2010. 8. Irritable bowel syndrome: textbook. manual / ed. IN AND. Sharobaro. Smolensk, 2011.
Treatment of the intestines in women
If you notice abdominal pain, constipation, diarrhea or other symptoms, immediately answer the question: “Do I know the reason why this could happen?” If you haven’t found any reasons (for example, you haven’t eaten fast food for the last three days), then it’s better to contact a good gastroenterologist .
Qualified doctors work, for example, in the ACMD-MEDOX clinic. They will not only find out the exact cause of the disease, conduct a diagnosis using special medical equipment, but also adjust the diet (if the latter really refers to the catalysts that caused the patient to have a medical problem).
Be healthy!
Why is inflammation of the intestinal walls dangerous?
Recently, the number of Russians diagnosed with IBD has increased annually by an average of 10–12%. Most often, residents of modern megacities suffer from ulcerative colitis and Crohn's disease. In the first case, the mucous membrane of the colon is affected, and in the second, the end of the small intestine and the beginning of the large intestine. Inflammation leads to the formation of bleeding ulcers and progresses rapidly, leading to irreversible tissue damage if undiagnosed and treated.
- Patients with Crohn's disease have a significantly increased risk of intestinal obstruction and, as a result, fistula formation.
- Massive bleeding in ulcerative colitis can cause intestinal perforation and life-threatening peritonitis.
- Finally, IBD is recognized as one of the factors that significantly increases the likelihood of tumor formation in the intestine.
Even at the initial stage, intestinal diseases manifest themselves with unpleasant symptoms that significantly reduce the quality of life.
What is irritable bowel syndrome and how to live with it
They occur frequently, but are not usually discussed - irritable bowel syndrome is just one of these diseases. It affects up to 25 percent of the world's population. How IBS manifests itself, is diagnosed and treated, explained Vera Serezhina, a medical expert at the LabQuest personalized medicine laboratory.
Symptoms: how does it manifest itself?
Although irritable bowel syndrome is common, it is not known exactly what causes the condition. Each patient with IBS has his own history of the onset of the disease, but it almost always involves stress factors - social, psychological, biological, etc. In addition, periods of exacerbation are also associated with stress. The work of the intestines is subject to nervous regulation, and constant stress leads, among other things, to disruption of its motor function.
It is believed that the main symptom of IBS is diarrhea, but rare bowel movements are another option. There is also a mixed option, when a person is bothered by both. Other symptoms include bloating, the association of intestinal symptoms with certain foods that either make you feel better or worse, a feeling of incomplete bowel movements, and sudden urges that force you to literally run to the toilet. In some cases, patients cannot leave the house because of this. There are manifestations that have nothing to do with the intestines: for example, insomnia, migraines, muscle pain, discomfort during sexual intercourse in women. By the way, women suffer from IBS much more often than men.
There are so-called Roman diagnostic criteria for IBS. This disease is characterized by recurrent abdominal pain that has occurred at least once a week over the past 3 months and has been associated with at least two of the following: associated with defecation, a change in stool frequency, and/or a change in stool shape.
A special feature of IBS is the morning ritual: every morning at a certain moment (for example, after breakfast), the patient begins to experience discomfort in the abdomen, and then the need to visit the toilet. The discomfort after this usually goes away until the next morning. The morning ritual does not happen in all cases of IBS; unfortunately, it is often much more difficult for patients and irritable bowels remind themselves not only in the morning.
Examination: what tests are needed
Often, patients with IBS manage to take control of the disease or adapt to it, learn to coexist with it, but this is not a solution, because the very situation with a chronic intestinal disorder, be it diarrhea or constipation, leads to impaired absorption of nutrients from food, and ultimately affects the functioning of the entire body. Therefore, it is better not to get used to IBS, but to be examined and, if the problem is really irritable bowel, to fight the cause.
Irritable bowel syndrome is a diagnosis of exclusion. It is diagnosed only after all other possible causes have been excluded: infectious and diseases of the endocrine system (thyroid and pancreas), food intolerance, autoimmune and oncological processes, etc. There are so-called “red flags” - symptoms that are in no way cases that cannot be ignored and require mandatory consultation with a doctor: weight loss, nighttime abdominal pain, the appearance of discomfort and pain in old age, cases of autoimmune diseases or intestinal cancer in the family, fever, blood in the stool.
Before a doctor makes a diagnosis of IBS, he must refer the patient for an examination, which includes several stages.
* Clinical and biochemical blood test. This will help identify anemia and
diseases of internal organs (diabetes mellitus, etc.)
* Stool analysis to identify intestinal pathogens (Shigella, Salmonella,
Yersinia), toxins A and B of Clostridium difficile.
* Study of the level of thyroid hormones to identify its hyperfunction.
* Stool analysis to detect hidden blood during an ulcerative process in the wall
intestines.
* Study of antibodies to tissue transglutaminase IgA or IgG in patients with
diarrheal and mixed variants of the disease if celiac disease is suspected.
* Determination of calprotectin level in feces. It will show the degree of inflammation in the wall
intestines.
* Ultrasound examination of the abdominal organs.
* Endoscopy with duodenal biopsy to exclude celiac disease. Biopsy
performed when antibodies to transglutaminase are detected in the diagnostic titer.
* Colonoscopy with biopsy.
Treatment: which doctor to go to and is it possible to forget about this disease?
IBS is the most common gastrointestinal disease. However, according to statistics, only one patient out of three goes to the doctor. The rest are left without help for various reasons. For some, IBS does not particularly interfere with life - there are quite a few of them, up to 40 percent of all patients. Another scenario: a person finds out that he “just” has irritable bowel syndrome, and not Crohn’s disease or intestinal cancer, calms down and lives from relapse to relapse. Often people with IBS go for help only to gastroenterologists and see diet as treatment. Eliminating certain foods - coffee, fatty foods, grains, spicy seasonings, etc. - can really give a noticeable result, as it can reduce the discomfort that causes flatulence. Only this is not enough. As soon as the patient experiences stress, irritable bowel syndrome makes itself felt again. The correct approach to treating this problem for many people with IBS involves the joint work of a gastroenterologist and a psychotherapist. The first one selects proper nutrition, antispasmodics, antidiarrheal or laxative drugs and other therapy, the second one helps to solve the underlying problems that lead to IBS, for example, to cope with increased anxiety. For some patients, talking with a psychotherapist is enough to understand the causes of the illness; others require a course of antidepressants. With intestinal diseases, a situation of amino acid deficiency arises in the body for the synthesis of the neurotransmitter serotonin, which is also called the hormone of happiness. Therefore, patients with IBS need to replenish this hormone and antidepressants have good therapeutic effects.