In the overwhelming majority of cases of ARVI, including coronavirus, antibiotics are not needed, according to the Russian Ministry of Health. Bacterial infection can be determined by several blood test parameters.
Altai and Russian doctors have recently been talking a lot about the dangers of prescribing antibiotics for signs of acute respiratory viral infection from the first days of illness, especially on their own. In the vast majority of cases, such treatment is unjustified, since viral pneumonitis and bacterial pneumonia are different diseases. And yet there are situations when bacteria join viruses. The most obvious sign is the appearance of purulent sputum. But the best way to tell is blood tests.
CRP – indications for examination
CRP is assigned:
- if the patient is at risk of a bacterial infection;
- For patients recovering from surgery, if CRP values remain elevated three days after surgery, a bacterial infection may be suspected;
- newborns with signs of infection;
- patients with signs of sepsis: fever, chills, rapid breathing and palpitations;
- when a health condition needs to be assessed, such as lupus or arthritis;
- to check the effectiveness of inflammation therapy - during it, the level of CRP should decrease;
- to study body damage and consequences after operations, organ transplants and burns, for early detection of possible infection.
The CRP test can help with:
- assessing the severity of the inflammatory process;
- early detection of postoperative complications;
- detection of transplant rejection;
- monitoring the success of antibiotic treatment for bacterial infections;
- monitoring patients with inflammatory rheumatic diseases.
Thus, the most common use of the CRP test is to determine its level when inflammation caused by a bacterial infection is suspected.
This is especially useful for distinguishing viral from bacterial infections. Since in viral infections - inflammations accompanied by increased sedimentation and an increase in the number of leukocytes, the level of CRP remains in a lower range than in the case of a bacterial infection. And in this case his growth is much higher.
An increase in CRP is present in the following cases:
- with inflammation;
- after operation;
- in the presence of malignant diseases;
- for allergic reactions;
- for chronic inflammatory diseases such as rheumatoid arthritis or lupus.
Microbiological cultures
What is microbiological culture? Microbiological culture is a study in which any biomaterial (blood, urine, mucus, pus, etc.) is transferred from the body to a nutrient medium, and if the transferred biomaterial contains microbes, they grow in this medium. In some cases, we combine microbiological cultures with PCR (polymerase chain reaction) research, because not all microbes grow well on media, but are easily detected by PCR, and vice versa, some microbes are poorly detected by PCR, but grow well on nutrient media. PCR is widely used to determine viral infections.
What biomaterials of the body can be tested on nutrient media. In our clinic you can inoculate almost any biomaterial: eye and nasal discharge, material obtained during puncture, saliva, various smears, sputum, feces, urine, blood, skin scrapings, hair (if there is a scalp infection), nails and etc.
Based on the readiness of microbiological inoculation, the sensitivity of the inoculated microbes to various antibiotics can be determined. After determining the sensitivity, it will be clear which drug will be suitable for treatment. It is also possible to determine the sensitivity of microbes to bacteriophages in cases where treatment without the use of antimicrobial chemotherapy is required.
High CRP and disease diagnosis
During an acute inflammatory reaction, the concentration of CRP increases many times over. It begins to grow 6 to 9 hours after the onset of inflammation and reaches a maximum after 48 hours. Protein returns to baseline levels within 7 to 10 days after stopping treatment.
| SPB level | Meaning | What does it indicate? |
| <5 mg/l | Normal | No inflammation |
| 0-40 mg/l | Slightly elevated | Mild inflammation |
| 40-200 mg/l | Increased | Acute inflammation |
| 200 and above mg/l | High | Severe bacterial infection |
Testing the concentration of C-reactive protein often reveals problems in the proper functioning of the body at an early stage before symptoms appear.
| Type of infection | SPB level |
| Gram-negative bacteria – Escherichia coli, Salmonella, Helicobacter pylori and others | 500 mg/l or more |
| Gram-positive bacteria – staphylococci, streptococci, tuberculosis or parasites | up to 100 mg/l |
| Viruses | up to 50 mg/l |
Results above 50 mg/L are a sign of serious infection, injury, or chronic disease, which will require additional testing to determine the cause.
In such situations, rapid identification of the bacterial pathogen is especially important to determine targeted antibiotic therapy.
2.Causes and risk factors
Bacterial infections are the most common cause of sepsis. But sepsis can also develop due to other infections. An infection can start anywhere—where bacteria or other infectious agents can enter the body. Blood poisoning can be the result of a seemingly harmless scratch or a serious medical problem - appendicitis, pneumonia, meningitis or a urinary tract infection. Sepsis can occur with bone infections - osteomyelitis.
Theoretically, anyone can develop sepsis. But some people are at increased risk of developing sepsis
. Among them:
- People whose immune systems are not functioning well due to diseases such as HIV/AIDS or cancer. This group also includes patients treated with narcotic drugs that suppress the immune system (for example, to prevent organ transplant rejection).
- Babies.
- Elderly people, especially if they have health problems.
- Patients hospitalized in the hospital, including those undergoing invasive medical procedures. According to statistics, common areas of primary infection in sepsis are surgical incisions, urinary catheters and bedsores.
- Patients with diabetes.
Visit our Therapy page
What can a CRP test show?
C-reactive protein manifests itself as a protective reaction of the body. Its function is to participate in the immune response, which consists in inactivating the inflammatory factor and stimulating the function of immune cells.
Quantitative CRP testing has less diagnostic value in the case of chronic inflammatory diseases such as rheumatic diseases, since the CRP value can vary from 10 to 1000 mg/L. However, diagnostically important is the fact that the level of CRP is associated with the degree and activity of the inflammatory process. Monitoring changes in the concentration of C-reactive protein - decrease or increase - informs about the stage of inflammation, its extinction or failure of therapy.
Before taking a CRP test, it is recommended that you consult with your doctor in advance to discuss any medical conditions that may affect the results.
It is important that your consultation with your doctor takes into account lifestyle risk factors, other medical conditions and family history. If there is a risk of cardiovascular disease, an echocardiogram, computed tomography of the coronary arteries, a stress test, cardiac catheterization or an electrocardiogram may be prescribed.
There is no need to panic, but you need to get treatment. What do we know about the Epstein-Barr virus?
You can't hide from him. Sooner or later, every person encounters him. Should we be afraid of him? Or maybe the infection is completely harmless? There is no need to panic, but a frivolous attitude is also a mistake.
Elena Gennadievna Koroleva, an infectious disease specialist at the Expert Clinic Tula, spoke about the Epstein-Barr virus.
— Elena Gennadievna, what is the Epstein-Barr virus?
— Among herpes viruses, there are 8 types that cause pathologies in the species Homo sapiens, that is, in people. Epstein-Barr virus is a type IV herpes virus. Once infected with the Epstein-Barr virus, the infection remains in the body forever and never leaves it.
Epstein-Barr virus is one of the most common herpes viruses in humans. Human susceptibility to it is high. Many children become infected before they reach the age of one, and by the age of 40-50, almost everyone has an infection in their body.
— How does Epstein-Barr virus infection occur?
— The source of infection is virus carriers, as well as patients with typical (manifest) and erased forms of the disease. The most common route of transmission is airborne droplets: with saliva particles when talking, sneezing, coughing. The virus can be transmitted by kissing (which is why in some sources the infectious mononucleosis caused by it is called the “kissing disease”). A contact route of infection is also possible (for example, through household items).
The Epstein-Barr virus enters the body through the upper respiratory tract, and from there it spreads into the lymphoid tissue, causing damage to the lymph nodes, tonsils, spleen and liver.
When the Epstein-Barr virus multiplies in the body, it affects the immune system. The mechanism of action is complex, but the end result is that due to damage to B lymphocytes and inhibition of T-cell immunity, the production of interferon, a protein responsible for the body’s antiviral defense, is suppressed.
In the modern world, children are experiencing a surge in morbidity, especially in cities. The highest probability of infection is in crowded places.
— Can an asymptomatic carrier be dangerous?
— Most often, the source of infection is a person in the acute stage of the disease. But transmission from an asymptomatic carrier cannot be ruled out.
— What disease is caused by the Epstein-Barr virus?
— The classic manifestation is infectious mononucleosis. It is characterized by general intoxication symptoms: high body temperature, drowsiness, lethargy, headaches, sore throat, swollen lymph nodes (or lymphoproliferative syndrome).
Lymphoproliferative syndrome combines:
- Damage to the oropharynx: acute pharyngitis with hypertrophy (enlargement) of the lymphoid tissue of the nasopharynx, acute adenoiditis and tonsillitis. This is manifested by difficult nasal breathing and snoring during sleep.
- Damage to peripheral lymph nodes (anterior cervical, submandibular and posterior cervical ones are often affected). A marked enlargement of the cervical lymph nodes may be accompanied by puffiness of the face and pasty eyelids.
- Enlarged liver and spleen.
A general blood test determines the presence of atypical mononuclear cells. What it is? Atypical mononuclear cells (another name is “virocytes”) are altered mononuclear blood cells. During the course of infectious mononucleosis, the number of atypical mononuclear cells in the blood increases significantly (more than 10%). The total number of platelets and leukocytes may decrease, which indicates the severity of the infection.
There are features of the manifestation of the Epstein-Barr virus in children. Those infected fall into the category of “frequently ill children.” Due to weakened immunity, diseases of the ENT organs regularly occur, difficulties during recovery (coughing, constantly red throat), and snoring occurs (due to the proliferation of tonsils). With this progression, by adulthood the immune system learns to resist infection, and adults no longer get sick as often. Indications for surgical removal of adenoids in children are almost always associated with untreated Epstein-Barr virus. And this is very sad: there is nothing unnecessary in the body, and with timely treatment, removal could have been avoided.
Read materials on the topic:
Often – how much? A frequently ill child is seen by a pediatrician. Adenoids in children: should they be removed or not?
Knowing that a child is infected is important for another reason. The Epstein-Barr virus can change the reaction to some antibiotics and provoke a toxicoallergic reaction. Therefore, it is imperative to identify the virus in a timely manner and report it to your attending physicians; they will select antibiotics taking this fact into account.
Severe consequences occur if primary infection occurs in a woman during pregnancy. The Epstein-Barr virus crosses the placental barrier, which can lead to fetal death or significant developmental defects.
“After the initial infection, some of these infections do not leave the body. They “sleep” in certain cells if everything is in order with the immune system and it controls their “sleep” well. Quote from the material “What are the dangers of TORCH infections”
— There is an opinion that the Epstein-Barr virus causes hepatitis and even lymphoma. This is true?
— Herpetic viruses spread throughout the body through the bloodstream and affect all groups of lymph nodes. Both the liver and spleen are enlarged in acute mononucleosis. In this case, the course of the disease is usually favorable, and liver health is completely restored.
It is impossible to say that the Epstein-Barr virus necessarily leads to lymphoma. Detecting the virus is not enough: if almost the entire population of the planet is infected, naturally, tests will detect the presence of the virus in the body, but not everyone gets lymphoma. Of course, chronic suppression of the immune system can lead to various disorders, including cancer. But there is no reliable connection. And modern medicine is able to compensate for immune disorders.
There's definitely no need to panic. But there is no need to hope for an independent cure. When a child is constantly sick, parents often fall into despair. And although it is impossible to get rid of herpes viruses forever, it is quite possible to alleviate the condition and significantly reduce the incidence of diseases. Treatment can and should be done.
Read more about hepatitis in our articles:
“The silent killer” of contemporaries How to protect yourself from Botkin’s disease Shield and sword from hepatitis C. How to protect yourself and your loved ones?
— What methods can be used to check whether the Epstein-Barr virus is present in the body? What tests detect it?
— We have two methods in our arsenal: enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR). The advantage of the PCR method is the ability to determine the DNA of the virus in saliva and scrapings from the nasopharynx. Thanks to this, you don’t have to take blood and don’t irritate the child. But if there is no exacerbation, such an analysis may give a false negative result. This means that the virus is in the body, but it is “sleeping”, and, accordingly, may not be present in a nasopharyngeal swab. And since PCR is used to look for the virus itself, or more precisely, its nucleic acids (DNA), the analysis will be negative. There are also frequent distortions due to the fact that the smear was taken incorrectly.
The ELISA method is more accurate; in any case, it will show both the presence of infection and the severity of the infectious process. In this case, conclusions are made based on the presence of specific immunoglobulins (antibodies) to the virus in the blood. For example, if immunoglobulins of class M (IgM) are detected, we can talk about the acute phase of the infection (primary infection or reactivation of a virus that once entered the body). If a certain fraction of immunoglobulin G (IgG) is found, this indicates that the body has already encountered an infection in the past. Therefore, to determine the diagnostic method, you need to consult a doctor.
— What methods of treating the Epstein-Barr virus does modern medicine have?
- This is a difficult task. While there are specific antiviral agents for herpes viruses type I and II (herpes simplex viruses), specific therapy has not yet been developed for the Epstein-Barr virus and cytomegalovirus. In mild cases, the disease may go away on its own, but in severe cases with damage to the bone marrow, medical attention is necessary. Treatment is aimed at stimulating the immune system, using interferons. The treatment regimen is chosen based on many factors; only a doctor should determine it.
After treatment, the virus continues to live in the body. Exacerbations may occur from time to time: due to hypothermia, prolonged exposure to the sun, stress, etc. Manifestations of infection are always a reason to go to the doctor.
Interviewed by Daria Ushkova
The editors recommend:
Herpes: how to recognize and cure? ELISA blood test: when is it used? Diagnosis of infections using PCR: what is it?
For reference:
Koroleva Elena Gennadievna
In 1992 she graduated from the pediatric faculty of the Kyrgyz State Medical Institute. From 1992 to 1993 - internship in pediatric infectious diseases. She worked at the Republican Infectious Diseases Hospital (Bishkek), first as a pediatric infectious disease specialist, then as a resuscitator in the intensive care unit for infectious patients. In Tula, she worked at the regional children's hospital for more than 10 years, and headed the intensive care unit for 7 years. Currently, he is a pediatric infectious disease specialist at the Expert Clinic in Tula. Receives at the address: Tula, st. Boldina, 74.
CRP and cardiovascular disease
Recently, CRP protein levels have also been taken into account in the diagnosis and treatment of cardiovascular diseases. It is used to assess the risk of myocardial infarction, ischemic stroke and sudden cardiac arrest. It turns out that there is a relationship between the risk of coronary heart disease and the level of CRP in the patient’s blood.
Low levels of CRP accompany mild inflammation, which medicine associates with atherosclerosis because the inflammatory process plays a key role in the detachment of atherosclerotic plaques, the formation of local blood clots and blockage of blood vessels. CRP levels are also associated with hypertension, low good cholesterol, and metabolic disorders leading to abdominal obesity.
According to the Cleveland Clinic, a non-profit multidisciplinary academic medical center (Ohio, USA), the CRP test can be used to identify the risk of developing cardiovascular diseases:
| CRP value | Risk of developing cardiovascular diseases |
| below 1 mg/l | Short |
| from 1 to 2.9 mg/l | Moderate |
| exceeds 3 mg/l | High |
However, the CRP test does not provide a complete picture of the risk of cardiovascular disease.
Other causes of elevated CRP
If the reading is above 10 mg/L, this may be a signal for further research to answer the question of what is causing the inflammation.
Such a high CRP value may indicate:
- osteomyelitis or bone infection;
- tuberculosis;
- inflammatory bowel diseases;
- lupus;
- connective tissue disease;
- some kind of autoimmune disease;
- exacerbation of autoimmune arthritis;
- pneumonia;
- type 2 diabetes;
- cancer – with a special indication for lymphoma.
Increased levels of CRP may occur in women:
- taking birth control pills;
- in pregnant women - this condition may indicate complications, so additional tests should be carried out to be sure.
CRP and cancer
The highest concentrations of CRP are observed in patients with malignant neoplasms, especially neoplasms of the hematopoietic system. Sometimes these are three-digit numbers or more. If the CRP blood test results show a high level of C-reactive protein, doctors immediately begin looking for a neoplastic process that, in addition to the elevated CRP level, has not yet caused any symptoms other than an altered ESR level.
However, keep in mind that the CRP test is not useful in diagnosing cancer. Too many other factors influence its level. A low level of CRP does not exclude the presence of a neoplasm, and its elevated level should direct the diagnosis primarily to infectious and inflammatory diseases. Moreover, the CRP protein is a very plastic molecule: the rate can increase up to a thousand times in 24 or 48 hours - this happens during acute bacterial or viral infections and after serious injuries.
Analysis of cerebrospinal fluid for neuroinfections. Examination of cerebrospinal fluid for viruses, bacteria, fungi
Our clinic specializes in neurology, neuroimmunology and the treatment of autoimmune diseases of the nervous system. The study of cerebrospinal fluid for neuroinfections is one of the most reliable methods for laboratory diagnosis of inflammatory and autoimmune diseases of the nervous system. We will offer you a study of cerebrospinal fluid for neuroinfections on an outpatient basis, with a stay in the day care ward. Read more about the procedure for obtaining cerebrospinal fluid.
A number of studies for neuroinfections can also be performed using blood tests: more details.
Which neuroinfections are available for research in our clinic:
| Chlamydia trachomatis PCR |
| Herpes simplex virus types 1 and 2 / Herpes simplex virus I, II PCR |
| The causative agent of syphilis / Treponema pallidum PCR |
| Cytomegalovirus / Cytomegalovirus PCR |
| Epstein-Barr virus / Epstein Barr virus PCR |
| Herpes virus type 6 / Human herpes virus VI PCR |
| Pathogen of tuberculosis / Mycobacterium tuberculosis complex PCR |
| Listeria / Listeria monocitogenes PCR |
| Toxoplasma / Toxoplasma gondii PCR |
| Microscopic examination of a stained smear (bacterioscopy) |
| Culture of microflora and determination of sensitivity to antibiotics |
| CSF culture for meningococcus |
| Culture for fungi of the genus Candida and determination of sensitivity to antimycotic drugs |
| Culture for anaerobic microflora and determination of sensitivity to antibiotics |
| Culture for gonococcus and determination of sensitivity to antibiotics |
| Serological diagnosis of tick-borne borreliosis using immunochip method (blood + CSF) |
| Enterovirus / PHK Enterovirus PCR |
| Varicella-Zoster virus (causative agent of herpes zoster) / Varicella-Zoster PCR |
| Adenovirus / Adenovirus (groups B, C, E) PCR |
The study of cerebrospinal fluid helps to make a differential diagnosis between neuroinfection and demyelinating disease, neurosarcoidosis, neuroleukemia, etc. CSF examination helps diagnose neuroborreliosis in doubtful cases. It is also possible to examine the cerebrospinal fluid for the presence of oligoclonal Igg antibodies to diagnose multiple sclerosis.
Carrying out a lumbar puncture. Lumbar puncture is a method of obtaining cerebrospinal fluid for laboratory testing. You can find out more information about lumbar puncture here.
To perform a lumbar puncture, we may need:
- MRI of the brain. If you have brain images no more than 3 months old, please bring them to the clinic. This is important for your safety: there may be risks.
- Examination by a neurologist. The doctor who will perform a lumbar puncture must know exactly the indications for this study in your case and understand the possible risks.
Elevated CRP – is this always a pathology?
In adults, an elevated CRP value exceeds 5 mg/l, with the exception of smokers, people with obesity or hypertension, for whom the norm is less than 10 mg/l.
In older children, elevated CRP values are considered to be greater than 10 mg/L. As with adults, interpretation of the result should be left to the pediatrician. He will evaluate the result in the context of the child's condition and medical history.
Slightly elevated CRP values up to 40 mg/l may be observed in older people and during pregnancy.
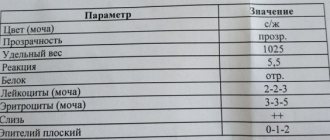
Therefore, when interpreting the results and drawing up a medical report, it is necessary to take into account other laboratory parameters, such as a complete blood count (CBC) with a leukocyte formula.
Effect of drugs on CRP concentration
Taking acetylsalicylic acid or aspirin, even in high doses, does not affect the quantitative level of CRP. This is somewhat surprising since aspirin is known for its anti-inflammatory properties.
Patients with high cholesterol who take statins are less likely to have a heart attack because statins not only lower lipid levels but also have anti-inflammatory properties. This is very important because high CRP and low cholesterol are more dangerous than high cholesterol and low CRP. The level of CRP is also reduced by drugs from the group of fibrates and beta-blockers, but less effectively than by statins.
C-reactive protein and ESR
ESR or Birnatsky reaction is a measurement of the erythrocyte sedimentation rate in a test tube with blood. It is expressed in millimeters per hour. ESR is an indirect indicator of the inflammatory response. However, the ESR test is less specific than CRP.
In addition to inflammation, an increase in ESR is also affected by:
- Obesity. Adipose tissue is a source of interleukin 6. This is one of the proteins involved in the formation of inflammation.
- Kidney failure. In end-stage renal failure and in the case of nephrotic syndrome, patients have significantly increased ESR values.
- Hemoglobin concentration. Anemia speeds up the decline of red blood cells.
- Shape of red blood cells. Determination of ESR is unreliable in diseases with abnormal red blood cells, such as sickle cell disease.
If there is a disproportion between CRP concentration and ESR, the first step is to consider the possibility of a false measurement due to the above factors or laboratory error, such as taking too long from collection to delivery to the laboratory or storing the tube in inappropriate conditions.
CRP levels respond more dynamically to increased inflammation than ESR. In the case of, for example, lupus erythematosus, the ESR value may be elevated when the level of CRP in the blood is low. This is caused by high levels of type 1 interferon, which suppresses the liver's production of CRP.
If you find an error, please select a piece of text and press Ctrl+Enter