In the article you will read what indicators are included in a general urine analysis, what are the reference intervals for these indicators, what is the norm of leukocytes and red blood cells in the urine, how much protein and sugar can be in the urine, what epithelial cells are found in the analysis.
The information was prepared by doctors from CIR laboratories and clinics.
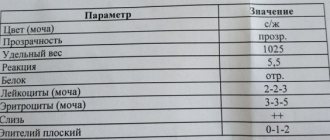
A general clinical examination of urine (general urinalysis, OAM) includes the determination of physical properties, chemical composition and microscopic examination of sediment.
Urine color
The color of urine normally ranges from light yellow to deep yellow and is due to the pigments it contains (urochrome A, urochrome B, uroethrin, uroresin, etc.).
Reference values:
| Children | Various shades of yellow |
| Men | Various shades of yellow |
| Women | Various shades of yellow |
Interpretation
The intensity of the color of urine depends on the amount of urine excreted and its specific gravity. Rich yellow urine is usually concentrated, excreted in small quantities and has a high specific gravity. Very light urine is slightly concentrated, has a low specific gravity and is excreted in large quantities.
Discoloration may be the result of a pathological process in the urinary system, the effects of dietary components, or medications taken.
What are the common causes of hematuria?
Blood in the urine is often not a sign of illness. Studies have shown that 9 to 18 percent of healthy people may have clinically insignificant microscopic hematuria. However, hematuria is often a warning sign for immediate treatment. Below is a list of the most common causes of hematuria:
- Bladder cancer.
- Kidney cancer.
- Prostate cancer.
- Ureteral cancer.
- Urethral cancer.
- Urolithiasis disease.
- Urinary tract infection.
- Pyelonephritis (kidney infection).
- Kidney diseases (hydronephrosis, polycystic disease, tuberculosis).
- Benign prostatic hyperplasia.
- Radiation or chemical cystitis.
- Urinary system injuries.
- Prostatitis.
- Severe physical strain.
Transparency (turbidity)
Normal urine is clear. Cloudiness of urine can be the result of the presence of red blood cells, leukocytes, epithelium, bacteria, fat droplets, precipitation of salts, pH, mucus, urine storage temperature (low temperature promotes the precipitation of salts).
In cases where the urine is cloudy, you should find out whether it is immediately cloudy, or whether this cloudiness occurs some time after standing.
| Children | Full transparency |
| Men | Full transparency |
| Women | Full transparency |
Specific gravity of urine (g/l)
In a healthy person, it can fluctuate over a fairly wide range throughout the day, which is associated with periodic food intake and loss of fluid through sweat and exhaled air.
| Children under 1 month | 1002-1020 |
| Children 2 – 12 months | 1002-1030 |
| Children 1 year - 6 years | 1002-1030 |
| Children 7 - 14 years old | 1001-1040 |
| Children 15 - 18 years old | 1001-1030 |
| Men | 1010-1025 |
| Women | 1010-1025 |
Interpretation
The specific gravity of urine depends on the amount of substances dissolved in it: urea, uric acid, creatinine, salts.
- A decrease in the specific gravity of urine (hyposthenuria) to 1005-1010 g/l indicates a decrease in the concentrating ability of the kidneys, an increase in the amount of urine excreted, and drinking plenty of fluids.
- An increase in the specific gravity of urine (hypersthenuria) of more than 1030 g/l is observed with a decrease in the amount of urine excreted, in patients with acute glomerulonephritis, systemic diseases, and cardiovascular failure; it may be associated with the appearance or increase of edema, large loss of fluid (vomiting, diarrhea ), toxicosis of pregnant women.
How to properly collect a urine test for women
Before urinating, women need to spread their labia with their fingers so that foreign impurities do not get into the urine from the skin of the external genitalia.
If a woman has copious vaginal discharge, then to prevent it from getting into the container with urine, it is recommended to cover the vagina with a napkin or insert a tampon.
The average portion of urine during the first morning urination is collected in a sterile container (the first and last portions are flushed into the toilet).
When collecting urine, it is advisable not to touch the container to your body.
The volume of urine for testing should be ¾ of the volume of the container. The minimum volume of urine for testing is 30 ml.
Urine collection is possible at any time during the day with prior agreement with the attending physician.
It is advisable to deliver the container with urine to the medical office within 2 hours after collecting the biomaterial.
Urine reaction (pH)
The pH of urine in a healthy person on a mixed diet is acidic or slightly acidic.
| Children under 1 month | 5,4 — 5,9 |
| Children 2 – 12 months | 6,9 — 7,8 |
| Children 1 year - 6 years | 5,0 — 7,0 |
| Children 7 - 14 years old | 4,7 — 7,5 |
| Children 15 - 18 years old | 4,7 — 7,5 |
| Men | 5,3 — 6,5 |
| Women | 5,3 — 6,5 |
Interpretation
The urine reaction may vary depending on the nature of the food. The predominance of animal proteins in the diet leads to a sharply acidic reaction; with a vegetable diet, the urine reaction is alkaline.
- An acidic urine reaction is observed with fevers of various origins, diabetes mellitus in the stage of decompensation, fasting, and renal failure.
- An alkaline reaction of urine is characteristic of cystitis, pyelonephritis, significant hematuria, after vomiting, diarrhea, and drinking alkaline mineral water.
What to do if you see blood in your urine?
Hematuria is defined as the presence of red blood cells in the urine. It can be described as “macrohematuria,” when blood in the urine is visible to the naked eye, or “microhematuria,” when red blood cells are detected under a microscope in urine tests.
Hematuria can originate from any part of the urinary tract, including the kidneys, ureters, bladder, prostate, and urethra. In many patients, during examination, serious causes leading to hematuria are not determined, but you need to know that hematuria can be a manifestation of infection, urolithiasis, and benign and malignant tumors of the urinary tract. Smoking, radiation, abuse of certain medications, severe pain, exposure to certain chemicals - all this can lead to hematuria.
Chemical examination of urine
Currently, chemical testing of urine is carried out on automatic analyzers using the dry chemistry method.
Chemical testing includes determination in urine:
- squirrel
- glucose
- ketone bodies
Protein in urine, normal protein in urine
Normal urine contains a very small amount of protein (less than 0.002 g/l), which is not detected by qualitative samples, so it is considered that there is no protein in the urine. The appearance of protein in the urine is called proteinuria.
| Children under 1 month | absent |
| Children 2 – 12 months | absent |
| Children 1 year - 6 years | absent |
| Children 7 - 14 years old | absent |
| Children 15 - 18 years old | absent |
| Men | < 0,1 |
| Women | < 0,1 |
Interpretation
Physiological proteinuria includes cases of temporary appearance of protein in the urine that are not associated with diseases. Such proteinuria is possible in healthy people after eating a large amount of protein-rich food, after severe physical stress, emotional experiences, and epileptic seizures.
Functional proteinuria associated with hemodynamic stress can occur in children with fever, emotional stress, congestive heart failure or hypertension, or after cooling.
Pathological proteinuria is divided into renal (prerenal) and extrarenal (postrenal):
- Extrarenal proteinuria is caused by an admixture of protein secreted by the urinary tract and genitals; they are observed in cystitis, pyelitis, prostatitis, urethritis, vulvovaginitis. Such proteinuria rarely exceeds 1 g/l (except for cases of severe pyuria - detection of a large number of leukocytes in the urine).
- Renal proteinuria is most often associated with acute and chronic glomerulonephritis and pyelonephritis, nephropathy in pregnancy, febrile conditions, severe chronic heart failure, renal amyloidosis, lipoid nephrosis, renal tuberculosis, hemorrhagic fevers, hemorrhagic vasculitis, hypertension.
False-positive results when using test strips can be caused by severe hematuria, increased density (more than 1.025) and pH (above 8.0) of urine.
Determination of glucose (sugar). Normal level of glucose in urine.
Also, urine normally contains traces of glucose not exceeding 0.02%, which, like protein, is not detected by ordinary qualitative tests.
| Children under 1 month | absent |
| Children 2 – 12 months | absent |
| Children 1 year - 6 years | absent |
| Children 7 - 14 years old | absent |
| Children 15 - 18 years old | absent |
| Men | 0 – 1,6 |
| Women | 0 – 1,6 |
Interpretation
The appearance of glucose in the urine (glucosuria) can be physiological and pathological.
- Physiological glucosuria is observed when eating large amounts of carbohydrates (alimentary glucosuria), after emotional stress (emotional glucosuria), after taking certain medications (caffeine, glucocorticoids), and in case of poisoning with morphine, chloroform, phosphorus.
- Pathological glucosuria can be of pancreatic origin (diabetes mellitus), thyroid (hyperthyroidism), pituitary (Ishchenko-Cushing syndrome), hepatic (bronze diabetes). To correctly assess glucosuria, it is necessary to determine the amount of sugar in daily urine, which is especially important in patients with diabetes.
Ketone bodies in urine
Ketone bodies (acetone, acetoacetic acid, (B-hydroxybutyric acid)) can sometimes be detected in the urine of a healthy person with a very small intake of carbohydrates and a large amount of fats and proteins.
| Children under 1 month | none |
| Children 2 – 12 months | none |
| Children 1 year - 6 years | none |
| Children 7 - 14 years old | none |
| Children 15 - 18 years old | none |
| Men | none |
| Women | none |
Interpretation
Ketone bodies appear in the urine during fasting, alcohol intoxication, diabetes mellitus, in children with vomiting and diarrhea, neuro-arthritic diathesis, as well as during severe infectious processes accompanied by a prolonged increase in temperature.
Hematuria as a manifestation of isolated urinary syndrome in children
Hematuria refers to the presence of red blood cells in the urine. Does this always indicate pathology? Can erythrocyturia be observed normally? If yes, in what quantity and how often? There is no clear answer to these questions. Many people consider the presence of single red blood cells in the morning urine collected after the appropriate toilet as a variant of the norm [2, 15, 19]. At the same time, children who even occasionally show single red blood cells in a general urine test require observation and a specific examination algorithm for often several months.
When considering hematuria as a manifestation of isolated urinary syndrome (IUS), it is necessary to take into account both the degree of its severity and the possibility of combining it with other changes in urine analysis and, above all, with proteinuria.
According to the degree of severity, macro- and microhematuria are distinguished. With gross hematuria, urine becomes reddish-brown in color (the color of “meat slop”). With microhematuria, the color of urine is not changed, but when examined under a microscope, the degree of hematuria varies. It is advisable to distinguish between severe hematuria (more than 50 red blood cells per field of view), moderate (30–50 per field of view) and minor (up to 10–15 per field of view).
Hematuria should also be distinguished by duration. It can be short-term (for example, during the passage of a stone), have an intermittent course, as is the case with Berger's disease - one of the variants of IgA nephropathy, and also be characterized by a persistent, persistent course, maintaining varying degrees of severity over many months and even years ( various types of glomerulonephritis, hereditary nephritis, some types of kidney dysplasia). It can be asymptomatic (with a number of congenital and hereditary kidney diseases) or accompanied by dysuria or pain syndrome (with renal colic).
Depending on the site of origin, hematuria can be renal or extrarenal. The presence of so-called “altered” erythrocytes in urine sediment does not always indicate their renal origin, because their morphology often depends on the osmolality of the urine and the duration of stay in it until microscopy of the sediment [26]. At the same time, “unchanged” red blood cells in the urine can be of renal origin (for example, with macrohematuria due to rupture of the basement membrane in some forms of glomerulonephritis or with hemorrhagic fever with kidney damage and the occurrence of thrombohemorrhagic syndrome; as well as with kidney tuberculosis, with Wilms tumor ). In turn, renal hematuria is divided into glomerular and tubular. For glomerular hematuria, the appearance of erythrocyte casts in the urine sediment is typical, but this is observed only in 30% of glomerular hematuria [25]. The renal nature of hematuria can be more reliably established using phase-contrast microscopy of urinary sediment [13].
Glomerular hematuria (), as a manifestation of IMS, occurs mainly with non-inflammatory damage to the glomerular capillaries; more precisely, in the absence of any pronounced proliferative reaction on the part of the mesangium. The only exception is IgA nephropathy, which can occur for a long time without any extrarenal manifestations. Diseases in which hematuria is accompanied by extrarenal symptoms morphologically have a pronounced proliferative nature of the inflammatory reaction either predominantly from the mesangium or from the endothelial lining of the glomerular capillaries.
Tubular hematuria is observed in a variety of diseases of both congenital and acquired origin ().
The mechanism of occurrence of renal hematuria. To this day, there is no common understanding of the pathogenesis of renal hematuria. It goes without saying that red blood cells can enter the urinary space of the kidney only from the capillary bed, and hematuria in renal pathology is traditionally associated with damage to the glomerular capillaries. In microhematuria, red blood cells pass through anatomical pores in the basement membrane due to its increased permeability [7, 23]. Gross hematuria is caused rather by necrosis of glomerular loops [9, 14, 20, 22, 23]. The cause of hematuria may be thinning of the basement membrane with disruption of the structure of type IV collagen and a decrease in the laminin content in its dense layer, which is characteristic of hereditary nephritis [5, 7].
It is considered more likely that the main site of penetration of red blood cells through the capillary wall is the glomerulus. This is facilitated by the increased intracapillary hydrostatic pressure present in the glomerulus, under the influence of which the red blood cells, changing their configuration, pass through the existing pores [18, 22]. Permeability to erythrocytes increases when the integrity of the basement membrane is disrupted, which occurs with immunoinflammatory damage to the capillary wall. Some authors do not exclude a violation of the morphofunctional properties of erythrocytes, in particular, a decrease in their charge, in the occurrence of hematuria [6]. However, there is no correlation between the severity of changes in the glomeruli and the degree of hematuria [11]. This fact, as well as the often absence of severe hematuria in nephrotic syndrome, when the structure of the basement membrane is sharply disrupted, has given rise to a number of authors to express a different point of view on the mechanism of hematuria, namely, the main place of release of erythrocytes is the peritubular capillaries [10, 11]. These capillaries, unlike glomerular capillaries, do not have an epithelial layer and are in very close contact with the tubular epithelium; in this case, significant changes of a dystrophic nature are often found both in the endothelial cells of the capillaries and in the epithelium of the tubules [11].
Despite the existing uncertainty about the nature of renal hematuria in nephropathies, it is nevertheless important to know the place of its origin - the glomerulus or tubule. Dysmorphism of erythrocytes, detected by phase-contrast microscopy, makes it possible to distinguish renal hematuria from extrarenal hematuria [4, 8, 9, 25, 26], but does not allow to differentiate glomerular erythrocyturia from peritubular [11, 16, 21, 27]. Tubular or peritubular hematuria may be indicated by the appearance in the urine of plasma low molecular weight proteins, which are usually completely reabsorbed in the proximal tubule. These proteins include beta2-microglobulin (beta2-MG). If, during hematuria, beta2-MG is detected in the urine in an amount exceeding 100 mg in the absence or less amount of albumin in it, then such hematuria should be regarded as tubular [24]. Other markers of tubular hematuria may include retinol binding protein [12] and alpha1-microglobulin [17, 28]. Determination of the latter is preferable, since beta2-MG is easily destroyed in very acidic urine.
Diagnosis of hematuria in children. Diagnosis of asymptomatic hematuria presents the greatest difficulties for the doctor. However, the absence of one or another symptomatology at the moment does not exclude the presence of it in the anamnesis, such as, for example, past pain, or dysuria, or fever without catarrhal phenomena. The diagnostic process, as always, should begin with a detailed history. The main points to which the doctor’s attention should be drawn when collecting an anamnesis are presented. Identification of certain features of the medical history will allow the most rational examination of the patient, and analysis of the circumstances under which hematuria was detected will help to simplify it.
It is extremely important to determine the age when the debut of hematuria took place, because establishing the fact of the appearance of hematuria in early childhood allows us to consider it as a manifestation, most often, of some congenital or hereditary pathology. A carefully studied family and obstetric history will allow you to confirm this. It is important to establish whether hematuria is constant or occurs occasionally against the background of any intercurrent illness, cooling or exercise. Its severity is also of certain importance, i.e. whether it manifests itself as macro- or microhematuria. But greater significance should be attached to the accompanying proteinuria, especially when it is permanent. This always indicates a renal origin of hematuria.
When starting to examine a child with detected hematuria in a clinic, first of all, it is necessary to determine the place of its origin, that is, whether the hematuria is renal or extrarenal. Undoubtedly, if hematuria is accompanied by proteinuria, then its non-renal origin is excluded. In the absence of proteinuria, the first step in the examination should be a two-glass test (see diagram 1 on page 56). The detection of red blood cells only in the first portion indicates their external origin. In this case, examination of the external genitalia, taking smears for microscopy and latent infection, scraping for enterobiasis will help identify the inflammatory process and its cause. If signs of inflammation are detected, it is necessary to exclude its allergic nature. To do this, in addition to obtaining relevant anamnestic data, a vulvo- or urocytogram should be prescribed, which, in the presence of a predominance of lymphocytes and the detection of eosinophils, will exclude the bacterial nature of the inflammatory process. The detection of red blood cells in two portions indicates involvement of the kidneys and/or bladder in the pathological process. Bladder pathology can be suspected, in addition to relevant anamnestic data, during ultrasound examination, but only cystoscopy makes it possible to definitively verify the presence or absence of cystitis. Ultrasound examination (ultrasound) can reveal changes in the position of the shape and size of the kidneys, suggesting the possibility of cystitis, as well as a neurogenic bladder. In addition, ultrasound can detect the presence of stones. Subsequent IV urography and/or renoscintigraphy will help clarify the nature of the detected changes.
Hematuria, combined with proteinuria, as already mentioned, is of renal origin. If this pathology is established in urine tests in early childhood, after taking an appropriate history (), it is necessary to determine whether the disease is congenital or hereditary. The proposed algorithm of actions (see diagram 2 on page 57) allows at the first stage not only to outline the differential diagnosis between congenital and hereditary kidney pathologies, but also to approach the identification of diseases such as interstitial nephritis and metabolic nephropathy, for which hematuria is one of the manifestations of this pathology.
When hematuria, combined with proteinuria, appears in preschool and school age, the hereditary or congenital nature of the disease cannot be ruled out. However, the role of acquired pathology in the form of various forms of primary or secondary glomerulonephritis, interstitial nephritis, diabetic nephropathy, and pyelonephritis is significantly increasing. After a detailed history collection, examination of this group of children should begin with the collection of 24-hour urine for protein and an orthostatic test. It is preferable to collect daily urine for protein separately during the day and at night. This makes it possible to assess the importance of physical activity on the severity of both proteinuria and hematuria. Since in children of this age group, when hematuria is combined with proteinuria, the incidence of various variants of glomerulonephritis increases, it is necessary to identify a possible connection between this pathology and hemolytic streptococcus. To do this, it is not enough to detect its presence by taking swabs from the throat; it is necessary to establish the appearance and increase in the titer of antistreptococcal antibodies (ASL-O), as well as the activation of the complementary system.
An obligatory step in the examination of this group of patients is an ultrasound scan of the kidneys. Despite the normal ultrasound characteristics of the kidneys in the presence of isolated urinary syndrome in the form of hematuria with proteinuria, regardless of their severity, a positive orthostatic test requires intravenous urography. The latter will eliminate kidney dystopia, the presence of their immobility, and also finally resolve the issue of the absence of pathological kidney mobility. For a functional examination, it is often enough to confine ourselves to performing the Zimnitsky test, and to clarify the state of the tubulointerstitium, a test with Lasix [1]. If certain abnormalities are detected by ultrasound of the kidneys, in addition to the above, it may be necessary to perform a Rehberg test, as well as renoscintigraphy.
Thus, before deciding on the need to use invasive examination methods in children with IMS, manifested in the form of hematuria, it is necessary to conduct the above basic examination on an outpatient basis. This will, on the one hand, prevent unnecessary hospitalization, and on the other, reduce the stay of children in a specialized bed if a more in-depth examination is required.
Literature
- Arkhipov V.V., Rivkin A.M. Diagnosis of the functional state of the kidneys using furosemide. Guidelines. St. Petersburg, 1996.
- Burtsev V.I., Turchina L.P. Hematuria // Clinical Medicine, 1997, No. 6, p. 66–69.
- Duman V. L. Phase-contrast microscopy of urinary sediment in the differential diagnosis of hematuria. Collection of proceedings of the IV annual nephrology seminar. St. Petersburg, 1996, p. 150–152.
- Zaidenvarg G. E., Savenkova N. D. Study of erythrocyte dysmorphism with phase-contrast microscopy, pH, urine osmolality in children with hematuria. Materials of the 1st Congress “Modern methods of diagnosis and treatment of nephrourological diseases in children.” M., 1998, p. 94.
- Ignatova M. S., Fokeeva V. V. Hereditary nephritis: diagnosis, pathogenesis, genetics, prognosis // Klin. honey. 1994, no. 2, p. 51–55.
- Nikolaev A. Yu., Shcherbin A. A. et al. The mechanism of hematuria in hematuric nephritis // Ter. archive, 1988, No. 6, p. 34–37.
- Papayan A.V., Savenkova N.D. Clinical nephrology. St. Petersburg 1997, p. 197–201.
- Prikhodina L. S., Malashina O. A. Modern ideas about hematuria in children // Nephrology and Dialysis, 2000, No. 3, p. 139–145.
- Savenkova N. D., Zaidenvarg G. E., Lisovaya N. A. Hematuria in children. Lecture. St. Petersburg, 1999.
- Shulutko B.I. Pathology of the kidneys. L., 1983, p. 80.
- Shulutko B.I. Nephrology. St. Petersburg 2002, p. 106–110.
- Bernard AM, Moreau D., Lanweys R. Comparison of retinal binding protein and beta2-microglobulin in urine in the early detection of ambular proteinuria // Clin. Chim. Acta. 1982; 126:1–7.
- Birch DF, Fairley KF Haematuria - glomerular or nonglomerular? // Lancet. 1979; vol. 2, p. 845–846.
- Bohle A. at al. Morphological contribution on gross hematuria in mild mesangioproliferative glomerulonephritis without crescents // Klin. Wochenschr. 1985; 63:371–378.
- Dodge WF, West EF et al. Proteinuria and hematuria in schoolchildren: epidemiology and early natural history // J. Pediatrics. 1976; 88:327–347.
- Gibbs DD, Linn KJ Red cell volume distribution curves in the diagnosis of glomerular and nonglomerular hematuria // Clin. Nephrol. 1990. 33: 143–147.
- Hofmann W., Rossmuller B., Guder WG, Edel HH A new strategy for characterizing proteinuria and haematuria from a single pattern of defined proteins in urine // Eur. J. Clin. Chem. Clin. Biochem. 1992; 30: 707–712.
- Jai-Trung L., Hiroyoshi W., Hiroshi M. et al. Mechanism of hematuria in glomerular disease // Nephron. 1983 Vol. 35. P. 68–72.
- Froom P. et al. Significance of microhaematuria in young adults // British Med. J., 1984; vol. 288, p. 20–21.
- Kincaid-Smidt P. et al. Acute renal failure and tubular necrosis associated with haematuria due to glomerulonephritis // Clin. Nephrol. 1983; 19: 206–210.
- Kitamota Y., Tomita M., Akamine M. et al. Differentiation of hematuria using a uniquely shaped red cell // Nephron. 1993, 64: 32–36.
- Lin JT et al. Mechanism of hematuria in glomerular disease. An electron microscopic study in a case of diffuse membranous glomerulonephritis // Nephron. 1983, 35: 68–72.
- Mouradian JA, Sherman RL Passage of erythrocyte throuhg a glomerular basement membrane gap // N. Engl. J. Med. 1975, 293(18):940–941.
- Peterson PA et al. Differentiation of glomerular, tubular and normal proteinuria: determinations of urinary excretion of beta2-microglobulin, albumin and total protein // J. Clin. Invest. 1969, 48: 1189–1198.
- Rizzoni G. et al. Evaluation of gomerular and nonglomerular hematuria by phase contrast microscopy // J. Pediatrics. 1983, 103: 370–371.
- Sandoz P. Verbesserte Urinsedimentdiagnostik durch Differenzierung der Eritrozytenmorphologie // Ther. Umschau. 1988, 12:851–856.
- Stapleton FB Morphology of urinary red blood cells: a simple guide in localizing the site of hematuria // Pediatr. Clin. North Am. 1987, 34(2):561–569.
- Yu H. et al. Alpha-1 microglobulin: an indicator protein for renal tubular function // J. Clin. Pathol. 1983, 36: 253–259.
A. M. Rivkin , Candidate of Medical Sciences, Associate Professor N. A. Lisovaya , Candidate of Medical Sciences
SPbGPMA, St. Petersburg
Contact information for authors for correspondence