Forms
The morphological substrate of the tumor is Berezovsky-Stenberg-Reed cells, however, their number in the tumor tissue rarely exceeds 10%. The second variant of cells is Hodgkin cells, which are a provariant of the Berezovsky-Stenberg-Reed cell. Depending on how the tumor tissue looks under a microscope, there are five forms of Hodgkin lymphoma.
- The variant of Hodgkin's disease with lymphocytic predominance accounts for 5-6% of all cases of HL. There are very few Berezovsky-Stenberg-Reed cells.
- The mixed cell variant is diagnosed in three quarters of patients. Berezovsky-Stenberg-Reed cells and Hodgkin cells are found in sufficient numbers.
- Lymphocytic depletion is the most rare morphological variant of the tumor (less than 1%).
- The most common variant of Hodgkin's lymphoma is nodular sclerosis.
- With nodular lymphoid predominance, the lymph node tissue is completely or partially replaced by an infiltrate of a nodular structure, often combined with zones of diffuse growth.
Forecast
Lymphogranulomatosis, which is the most common of the lymphomas, has the most favorable prognosis. When Hodgkin's lymphoma is detected at the first or second stage, clinical recovery after treatment occurs in 70% of patients.
The progression of the disease reduces the rate of favorable outcome. Stage 4 of the disease makes the prognosis unfavorable. However, as always when making predictions in medicine, we must not forget that we are talking about an organism that is unique in its individuality. A simple transfer of statistical indicators cannot be truly decisive in the outcome of the disease.
Non-measurable factors such as faith, hope, perseverance influence the body’s resistance and produce favorable results, increasing the effectiveness of treatment.
Clinical stages
Clinical stage is determined according to the Ann Arbor classification (1971), supplemented by the Cotswold recommendations (1989):
Stage I - damage to one or two groups of lymph nodes (I) or one non-lymphatic organ (or tissue) - (IE);
Stage II - involvement of two or more lymphatic areas on one side of the diaphragm (II) or involvement of one non-lymphatic organ (or tissue) and one (or more) lymphatic areas on one side of the diaphragm (IIE), involvement of the spleen (IIS);
Stage III - involvement of the lymphatic system on both sides of the diaphragm (III), which may be combined with localized involvement of one non-lymphatic organ or tissue (IIIE), or involvement of the spleen (IIIS), or involvement of both (IIIES);
Stage IV - widespread damage to one or more non-lymphatic organs (lungs, pleura, pericardium, bone marrow, bones, etc.) with or without involvement of the lymph nodes.
In Fig. Figure 1 shows the affected areas in Hodgkin lymphoma.
Rice. 1. Affected areas in Hodgkin's disease
What kind of disease is this?
Hodgkin's lymphoma is a type of tumor that usually affects the body's lymphatic system, which consists of lymph nodes interconnected by small vessels. As a result of the constant division of affected lymphocytes, their new cells move to somatic organs and lymph nodes, thereby disrupting their adequate functioning. The disease was first described in 1832 by Thomas Hodgkin. Until 2001, it was called lymphogranulosis or Hodgkin's disease. This pathological process affects people of any age. Moreover, statistics prove that women suffer from this disease much less often than men.
To the very common question “is lymphoma cancer or not?” You can answer briefly and unequivocally: “Yes.” The term “cancer” is a Russian translation (that is, a literal translation) of the Latin word “cancer” (crab). In the original language of science - Latin, this was the name from ancient times for all internal tumors that were asymmetrical and had an irregular angular shape when palpated and were accompanied by unbearable gnawing pain.
Therefore, the term “cancer” (or in the literal Russian translation – “cancer”) is assigned to all malignant tumors. And in a broad concept, it is often transferred to any tumor process, although the combinations “blood cancer” or “lymph cancer” used in colloquial speech offend the ears of a specialist, since cancer is a malignant tumor of epithelial cells. Based on this, it would be more correct to call lymphomas malignant tumors rather than the term “cancer.”
Symptoms
The first and most characteristic symptom of Hodgkin lymphoma is enlarged lymph nodes. Lymph nodes are usually painless, dense, mobile, often in the form of conglomerates (reminiscent of a “bag of potatoes”). The most common enlarged lymph nodes can be seen in the neck (Fig. 2), in the armpits, near the collarbone, in the groin, or in several places at the same time. Lymph nodes can also enlarge where they cannot be felt, for example, in the chest, abdomen, or pelvis.
Rice. 2. Damage to the cervical lymph nodes in Hodgkin lymphoma.
If enlarged lymph nodes are located in the chest (mediastinum) (Fig. 3), coughing attacks or shortness of breath may occur.
Sometimes the liver and spleen become enlarged (in medical practice this is called hepatomegaly and splenomegaly).
Central nervous system involvement can develop in advanced cases of Hodgkin lymphoma.
Bone damage: the vertebrae and hip joints are most often affected.
Bone marrow involvement occurs in 5-10% of cases of Hodgkin's disease.
Children may experience general symptoms of the disease : increased body temperature above 38°C for three days without signs of infectious diseases, severe night sweats, weight loss of more than 10% over the past 6 months for no apparent reason, fatigue, weakness, skin itching all over the body. In medical practice, these symptoms are called B-symptoms and are designated by the letter “B”; they are used in determining the stage of the disease.
For staging, it is necessary to take into account the biological activity of the disease . It is determined on the basis of two or more of the following indicators: ESR ≥ 30 mm/hour; fibrinogen ≥ 4 g/l; albumin ≤ 40%; SRB (++ and more); leukocyte count ≥ 12x10 /l; alpha-2-globulin ≥ 12%
Diagnostics
If, after a thorough examination, the pediatrician finds signs of Hodgkin's lymphoma, then he gives a referral to a specialized hospital (clinic of pediatric oncology and hematology).
The following are carried out in the hospital:
- Examination of the affected tissue . The main method of diagnosing lymphoma is a biopsy (surgical removal of the affected lymph node or tissue and examination of the material under a microscope). Based on the results of examining a tissue sample, it is possible to accurately determine whether a child has Hodgkin lymphoma, and if so, what type of lymphoma.
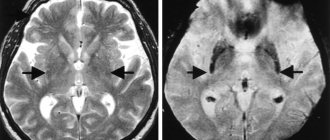
- Analysis of the prevalence of disease in the body. After making a diagnosis, it is necessary to find out how far the disease has spread throughout the body and what organs it has affected. For this purpose, PET-CT with glucose is performed. According to indications, a bone marrow examination is performed (trephine biopsy of the bone marrow in patients with stages IB, IIB-IV), osteoscintigraphy, and MRI for bone lesions.
- If there is a history of cardiovascular pathology, a heart murmur is listened to, and LVEF (left ventricular ejection function) is performed.
Rice. 3. Damage to the intrathoracic lymph nodes in Hodgkin lymphoma
Causes
So far, experts have not been able to definitively determine the specific causes of lymphogranulomatosis. Some scientists are inclined to believe that the disease has a viral etiology. They believe that the root cause of Hodgkin lymphoma is the Epstein-Barr virus, which provokes the development of cellular changes and mutations at the gene level.
In addition, experts have identified several factors that provoke pathology:
- Radiation exposure;
- Living in unfavorable environmental conditions;
- Working with carcinogenic or chemical substances such as pesticides, benzenes, herbicides, organic solvents, etc.;
- The presence in the family history of ancestors with pathologies of the lymphatic system (a controversial factor)
The occurrence of lymphomas is often affected by anti-cancer drugs used in chemotherapy treatment or hormone-based drugs. In addition, autoimmune diseases such as lupus, rheumatoid arthritis, etc. can affect the presence of pathology.
Contrary to popular assumption, the genetic factor is not particularly important in the formation of lymphomas. Although if a lesion is found in one of the identical twins, then the other twin will also have it.
Modern approaches to treatment
Chemotherapy occupies the main place in the treatment of Hodgkin lymphoma.
Chemotherapy is treatment with drugs (cytostatics) that block the division or kill tumor cells. The maximum effect can be achieved using combinations of cytostatics (polychemotherapy - PCT), which have different effects on cells.
Polychemotherapy is carried out in accordance with the risk group to which the patient was assigned during primary staging, in a specialized hospital.
Fig.4
The first cycle of chemotherapy begins immediately after the diagnosis is confirmed and the stage is established; in the case of surgical treatment, polychemotherapy begins 5 days after the operation.
After chemotherapy, radiation therapy (irradiation) is given to the affected areas. Radiation therapy should begin within 14 days of the end of chemotherapy if blood counts are normal.
In Russia today there are two main treatment programs for Hodgkin lymphoma: DAL-HD and SPbHL. Both protocols include polychemotherapy and final radiation therapy. The number of cycles of PCT depends on the stage of the disease and on the choice of therapeutic group in which the patient is treated. Patients usually receive the following program: with favorable options (1st risk group) - 2 cycles of chemotherapy, with an intermediate prognosis (2nd risk group) - 4 cycles of chemotherapy, with unfavorable options (3rd risk group) - 6 cycles of chemotherapy . The division of patients into risk groups has some differences depending on the protocol used.
DAL-HD uses OPPA/OEPA and COPP schemes. The SPbLH protocol contains VBVP and ABVD schemes.
Possible consequences of nodular lymphoma
The main danger of nodular lymphoma is the likelihood of its transformation into B-cell non-Hodgkin lymphoma. Data about this appeared back in the 90s of the twentieth century, and were subsequently confirmed by clinical studies. In particular, the European Lymphoma Working Group reported that 2.7% of patients developed a second lymphoma within 6-8 years. At the same time, in patients with the classical form of lymphogranulomatosis, this figure was 0.9%. At the same time, molecular genetic studies confirmed the clonality of tumor lines.
Radiation therapy
The final stage of treatment for Hodgkin lymphoma is irradiation of all affected areas of the lymph nodes. As a rule, radiation therapy begins 2 weeks after the end of drug therapy when blood counts are normalized.
The radiation dose depends on the completeness of remission after drug therapy: upon achieving complete remission (disappearance of all clinical and radiological signs of the disease) in the lymphatic zone, according to PET-CT data, the radiation dose is 20 Gy. If the size of the tumor after polychemotherapy has decreased by 75% or more from the original tumor and/or there is a decrease in radiopharmaceutical hyperfixation according to PET-CT to 2-3 according to Deauville, then the radiation dose is 25 Gy. If tumor formations are reduced by less than 75% and/or radiopharmaceutical hyperfixation persists according to PET-CT 4-5 according to Deauville, the radiation dose is increased to 30 Gy.
Fig. 5 Radiation treatment plan. Patient I., 4 years 6 months. Hodgkin's lymphoma stage II. with damage to the cervical, supraclavicular, subclavian lymph nodes on the left, the thymus gland, and the nasopharynx. Condition after 4 courses of PCT, remission. Irradiation of the cervical-supraclavicular lymph nodes on the left with a consolidating purpose, SOD 20 Gy.
Fig.6 Patient M., 11 years old. Hodgkin's lymphoma stage II. with damage to the soft tissues of the neck, lymph nodes of the neck. Condition after 2 courses of chemotherapy. According to the control PET/CT data, no metabolically significant lesions were identified, remission. Conducting radiation therapy of the primary involved areas with a total focal dose of 20.0 Gy for the purpose of consolidation.
Prognosis for nodular lymphoma
Nodular lymphoma is characterized by a slow course, has a high curability, and therefore the prognosis of the disease in most cases is favorable. But it is necessary to take into account that the main cause of death in this pathology is long-term complications after treatment, which include pathology of the cardiovascular system and the formation of secondary malignant neoplasms. In this regard, the question arises of finding safe treatment methods, both during immediate use and in the long-term period. This is especially true for late toxic complications, which significantly reduce the quality of life of patients.
Great hopes are placed on expanding the use of rituximab and introducing it into standard first-line treatment protocols. When using radiation therapy, it is recommended to use modern radiation technologies that allow the required dose to be delivered directly to the tumor site, while minimally affecting uncompromised tissue.
Euroonco doctors have extensive experience in treating nodular lymphoma. Thanks to the good material and technical base of the clinic and the use of modern treatment protocols, in most cases the disease can be brought under control and the desired effect achieved.
Book a consultation 24 hours a day
+7+7+78
Criteria for assessing the completeness of remission
Criteria for assessing remission are needed by the doctor to determine the need to continue treatment or intensify therapy programs, or transfer the patient under dynamic observation.
- Complete remission - complete regression of all signs of the disease (clinical, hematological and other manifestations of the disease) according to imaging tests, determined twice with an interval of at least 4 weeks.
- Partial remission is a reduction in the size of tumor formations by at least 50% for a period of 4 weeks in the absence of new lesions.
- Stabilization of the disease is a reduction in the size of tumor formations by less than 50% or an increase in them by no more than 25% of the original volume in the absence of new lesions.
- Progression is the appearance of new lesions during treatment or an increase in previously existing ones by more than 25%, as well as the appearance of symptoms of intoxication.
- Relapse is the appearance of new lesions after achieving complete remission.
Prevention
Unfortunately, to date, effective prevention of this disease has not been developed. More attention is paid to the prevention of relapses; this requires strict adherence to the prescribed treatment program for lymphogranulomatosis and the implementation of the necessary regimen and rhythm of everyday life.
Among the most common reasons for the recurrence of the disease are insolation and pregnancy. After suffering from this disease, the possibility of pregnancy is possible two years after remission.