Genetic pathologies are rare congenital diseases that are difficult to predict in advance. They arise even at the moment when the formation of the embryo occurs. Most often they are passed on from parents, but this does not always happen. In some cases, gene disorders occur independently. Bruton's disease is considered one of these pathologies. It refers to primary immunodeficiency conditions. This disease was discovered recently, in the mid-20th century. Therefore, it has not been fully studied by doctors. It occurs quite rarely, only in boys.
Bruton's disease: history of study
This pathology refers to X-linked chromosomal abnormalities transmitted at the genetic level. Bruton's disease is characterized by disturbances in humoral immunity. Its main symptom is susceptibility to infectious processes. The first mention of this pathology was in 1952. At that time, the American scientist Bruton studied the history of a child who was sick more than 10 times at the age of 4. Among the infectious processes in this boy were sepsis, pneumonia, meningitis, and inflammation of the upper respiratory tract. When examining the child, it was found that there were no antibodies to these diseases. In other words, no immune response was observed after the infections.
Later, in the late 20th century, Bruton's disease was studied again by doctors. In 1993, doctors were able to identify a defective gene that causes immune dysfunction.
Pathogens
The causative agents of Lyme disease are several species of human pathogenic borrelia - Borrelia burgdorferi, Borrelia garinii and Borrelia afzelii. Borrelia are microaerophiles and, like other gram-negative spirochetes, are extremely demanding on cultivation conditions. Infections caused by Borrelia burgdorferi most often present with arthritis (especially in North America, where it is the only causative agent of borreliosis), while B. garinii is more likely to cause neurological disorders and B. afzelii is more likely to cause chronic skin diseases. All three pathogens cause erythema migrans.
Causes of Bruton's disease
Agammaglobulinemia (Bruton's disease) is most often hereditary. The defect is considered a recessive trait, so the probability of having a child with the pathology is 25%. Women are carriers of the mutant gene. This is due to the fact that the defect is localized on the X chromosome. However, the disease is transmitted only to males. The main cause of agammaglobulinemia is a defective protein that is part of the gene encoding tyrosine kinase. In addition, Bruton's disease can also be idiopathic. This means that the reason for its appearance remains unclear. Among the risk factors affecting the genetic code of a child are:
- Alcohol and drug abuse during pregnancy.
- Psycho-emotional stress.
- Exposure to ionizing radiation.
- Chemical irritants (harmful production, unfavorable environment).
What is the pathogenesis of the disease?
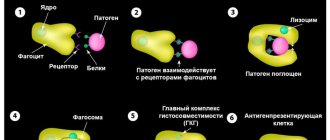
The mechanism of disease development is associated with a defective protein. Normally, the gene responsible for encoding tyrosine kinase is involved in the formation of B lymphocytes. They are immune cells that are responsible for the body's humoral defense. Due to the failure of tyrosine kinase, B lymphocytes do not mature completely. As a result, they are not able to produce immunoglobulins - antibodies. The pathogenesis of Bruton's disease is the complete blocking of humoral defense. As a result, when infectious agents enter the body, antibodies to them are not produced. A feature of this disease is that the immune system is able to fight viruses, despite the absence of B lymphocytes. The nature of the violation of humoral protection depends on the severity of the defect.
Epidemiology
The natural hosts of Borrelia in nature are wild animals (rodents, birds, deer), which feed ticks of the genus Ixodes - carriers of Borrelia. During blood sucking, borrelia enter the tick's intestines, where they multiply and are excreted in feces. Despite the high level of infection of ticks, the possibility of infection through a bite is not always realized, because borrelia are contained in the salivary glands in small quantities or are absent altogether.
In natural foci, the circulation of the pathogen occurs as follows: ticks → wild animals → ticks. It is possible that domestic animals - goats, sheep, cows - may be involved in the epidemiological chain. The likelihood of other carriers of Borrelia, such as horse flies, is being studied. A person becomes infected with Lyme disease in natural foci. Natural foci of Lyme disease are found mainly in forest landscapes of the temperate climate zone. In recent years, it has been established that the area of distribution of tick-borne borreliosis coincides with tick-borne encephalitis, and the disease is registered throughout the Russian Federation. However, the incidence of Lyme disease is 2-4 times higher than tick-borne encephalitis, and it occupies one of the first places among natural focal zoonoses. Tick-borne borreliosis is widespread in Europe, Asia, and America. In Russia, borreliosis is widespread in the forest and forest-steppe zones from Kaliningrad to Sakhalin. In European Russia, borreliosis is the most common tick-borne infection.
The risk of getting borreliosis after a tick bite is much higher than tick-borne encephalitis. Natural foci of tick-borne borreliosis coincide with the range of ixodid ticks. The incidence of borreliosis is seasonal and coincides with the activity of ticks. The first patients with tick bites are usually registered in March-April. The latter, in the presence of warm weather, are recorded even in October. Peak activity occurs in May-June. The percentage of ticks infected with borreliosis differs in different regions. A tick can simultaneously be infected with Borrelia, tick-borne encephalitis virus and other pathogens. Therefore, the development of a mixed infection is possible.
Transmission of the infection occurs transmissibly through a tick bite (inoculation), although the possibility of infection cannot be ruled out when tick feces come into contact with the skin, followed by rubbing them in when scratching (contamination). In case of a tick rupture, due to improper removal? the pathogen may enter the wound. The nutritional route of infection through consumption of raw goat or cow milk is discussed.
The main risk groups are workers of forestry farms, timber industry enterprises, hunters, foresters and residents of forested areas.
The carriers of Borrelia are ticks of the genus Ixodes, in our country and Europe - I. ricinus and I. persulcatus, in America - I. pacificus and I. scapularis. The life cycle of these ticks (larva - nymph - adult) lasts an average of three years. Ticks become infected from numerous rodents, as well as hares, hedgehogs, birds, etc. Ticks live in grasses, ferns and low shrubs.
Bruton's disease: symptoms of pathology
Pathology first makes itself felt in infancy. Most often, the disease manifests itself by the 3-4th month of life. This is explained by the fact that at this age the child’s body ceases to be protected by maternal antibodies. The first signs of pathology may be a painful reaction after vaccination, skin rashes, and upper or lower respiratory tract infections. Nevertheless, breastfeeding protects the baby from inflammatory processes, since mother's milk contains immunoglobulins.
Bruton's disease manifests itself at approximately 4 years of age. At this time, the child begins to contact other children and attends kindergarten. Among infectious lesions, meningo-, strepto- and staphylococcal microflora predominate. As a result, children may be susceptible to purulent inflammation. The most common diseases include pneumonia, sinusitis, otitis media, sinusitis, meningitis, and conjunctivitis. If not treated in a timely manner, all these processes can develop into sepsis. Dermatological pathologies can also be a manifestation of Bruton's disease. Due to a reduced immune response, microorganisms quickly multiply at the site of wounds and scratches.
In addition, manifestations of the disease include bronchiectasis - pathological changes in the lungs. Symptoms include shortness of breath, chest pain, and sometimes hemoptysis. It is also possible for inflammatory foci to appear in the digestive organs, genitourinary system, and mucous membranes. Swelling and pain in the joints are periodically observed.
Prevention
There is no prophylactic vaccine to prevent borreliosis. The best prevention is protection against tick bites. Prevention consists of observing individual protection measures against tick attacks and raising awareness among the general public. Proper tick removal is of great importance for preventing infection. If the tick has attached itself, it needs to be removed quickly. Borrelia live in the intestines of the tick and do not immediately enter the bloodstream. The longer the tick was on the body, the higher the risk of borreliosis.
The question of the benefits of preventing borreliosis after a tick bite with antibiotics is controversial. Prescribing antibiotics in the first days after a bite can reduce the risk of illness. But they should only be prescribed by a doctor. If a bite occurs, you should immediately seek medical help.
Due to the lack of specific prevention measures, identifying patients based on early clinical signs and mandatory antibiotic therapy according to a rational regimen are of particular importance to avoid severe late complications.
Diagnostic criteria for the disease
The first diagnostic criterion is frequent morbidity. Children suffering from Bruton's pathology suffer more than 10 infections per year, as well as several times during the month. Diseases can recur or replace each other (otitis media, tonsillitis, pneumonia). When examining the pharynx, there is no hypertrophy of the tonsils. The same applies to palpation of peripheral lymph nodes. You should also pay attention to the baby’s reaction after vaccination. Significant changes are observed in laboratory tests. The CBC shows signs of an inflammatory reaction (increased number of leukocytes, accelerated ESR). At the same time, the number of immune cells is reduced. This is reflected in the leukocyte formula: a low number of lymphocytes and an increased content of neutrophils. An important study is an immunogram. It reflects the decrease or absence of antibodies. This sign allows you to make a diagnosis. If the doctor has doubts, a genetic test can be performed.
Differences between Bruton's disease and similar pathologies
This pathology is differentiated from other primary and secondary immunodeficiencies. Among them are agammaglobulinemia of the Swiss type, DiGeorge syndrome, and HIV. In contrast to these pathologies, Bruton's disease is characterized by a violation of only humoral immunity. This is manifested by the fact that the body is able to fight viral agents. This factor differs from agammaglobulinemia of the Swiss type, in which both humoral and cellular immune responses are impaired. To make a differential diagnosis with DiGeorge syndrome, it is necessary to take a chest x-ray (thymic aplasia) and determine the calcium level. To exclude HIV infection, palpation of the lymph nodes and ELISA are performed.
Treatment methods for agammaglobulinemia
Unfortunately, it is impossible to completely overcome Bruton's disease. Treatment methods for agammaglobulinemia include replacement and symptomatic therapy. The main goal is to achieve a normal level of immunoglobulins in the blood. The amount of antibodies should be close to 3 g/l. For this purpose, gamma globulin is used at a rate of 400 mg/kg body weight. The concentration of antibodies should be increased during acute infectious diseases, since the body cannot cope with them on its own.
In addition, symptomatic treatment is carried out. The most commonly prescribed antibacterial drugs are Ceftriaxone, Penicillin, and Ciprofloxacin. For skin manifestations, local treatment is necessary. It is also recommended to wash the mucous membranes with antiseptic solutions (irrigation of the throat and nose).
Diagnostics
The blood pattern has its own characteristics
During diagnosis, the patient's medical history is studied, and characteristic signs are noted using radiography: abnormally small sizes of the tonsils and lymph nodes, disruption of the structure of the spleen.
Laboratory research data reveals:
- Significant decrease in B lymphocytes.
- Leukopenia may be accompanied by neutropenia.
- The number of T-lymphocytes is usually close to normal, but can be increased as a compensatory function.
- All isotypes of immunoglobulins (IgG, IgM, IgA, IgE, IgD) are absent or markedly reduced. The IgG level is determined first; a level < 100 mg/dL is a prerequisite for diagnosis.
- There are no plasma cells in the intestinal mucosa.
Additional examinations include ultrasound of the abdominal organs, colonoscopy, and lung diagnostics.
Prognosis for Bruton's agammaglobulinemia
Despite lifelong replacement therapy, the prognosis for agammaglobulinemia is favorable. Constant treatment and prevention of infectious processes reduce the incidence to a minimum. Patients usually remain able-bodied and active. With the wrong approach to treatment, complications may develop, including sepsis. In case of advanced infections, the prognosis is unfavorable.