How common is toxicosis during pregnancy?
This ailment occurs during most pregnancies. It affects 3 out of 4 women, and in only one of them the symptoms are limited to nausea; in the other two, vomiting comes along with it.
Many women who suffered during their first pregnancy are very afraid to meet him again. This is possible, but not at all necessary. The presence or absence of this disease and how severe it was does not help in any way to predict what will happen during the next pregnancy.
Sources
- Waldthaler A., Schramm C., Bergquist A. Present and future role of endoscopic retrograde cholangiography in primary sclerosing cholangitis. // Eur J Med Genet - 2021 - Vol - NNULL - p.104231; PMID:33905896
- Cai J., Qiong G., Li C., Sun L., Luo Y., Yuan S., Gonzalez FJ., Xu J. Manassantin B attenuates obesity by inhibiting adipogenesis and lipogenesis in an AMPK dependent manner. // FASEB J - 2021 - Vol35 - N5 - p.e21496; PMID:33904622
- Tu S.Y., Tsai T.Y., Chen CH., Wong CH. A Postpartum Woman With Right Upper Quadrant Pain and Jaundice. // Ann Emerg Med - 2021 - Vol77 - N5 - p.499-522; PMID:33902826
- Hriskova K., Marosevic D., Belting A., Wenzel JJ., Carl A., Katz K. Epidemiology of Hepatitis E in 2021 in Bavaria, Germany. // Food Environ Virol - 2021 - Vol - NNULL - p.; PMID:33900549
- de Jong JJ., Lantinga MA., Tan ACITL., Aquarius M., Scheffer RCH., Uil JJ., de Reuver PR., Keszthelyi D., Westert GP., Masclee AAM., Drenth JPH. Web-Based Educational Intervention for Patients With Uninvestigated Dyspepsia Referred for Upper Gastrointestinal Tract Endoscopy: A Randomized Clinical Trial. // JAMA Intern Med - 2021 - Vol - NNULL - p.; PMID:33900373
- Pereira P., Santos AL., Morais R., Vilas-Boas F., Rodrigues-Pinto E., Santos-Antunes J., Macedo G. Endoscopic radiofrequency ablation for palliative treatment of hilar cholangiocarcinoma. // VideoGIE - 2021 - Vol6 - N4 - p.195-198; PMID:33898902
- Sampurna MTA., Rohsiswatmo R., Primadi A., Wandita S., Sulistijono E., Bos AF., Sauer PJJ., Hulzebos CV., Dijk PH. The knowledge of Indonesian pediatric residents on hyperbilirubinemia management. // Heliyon - 2021 - Vol7 - N4 - p.e06661; PMID:33898814
- Chen X., Yu L. A haemorrhagic cholecystitis presenting as obstructive jaundice. // Hepatobiliary Surg Nutr - 2021 - Vol10 - N2 - p.299-300; PMID:33898585
- Fraser DD, Patterson EK, Daley M, Cepinskas G. Case Report: Inflammation and Endothelial Injury Profiling of COVID-19 Pediatric Multisystem Inflammatory Syndrome (MIS-C). // Front Pediatr - 2021 - Vol9 - NNULL - p.597926; PMID:33898353
- Adil H., Semedo A., Kessab A., En-Nouali H., El Fenni J., Abdellaoui M. Tuberculous common bile duct stricture mimicking a cholangiocarcinoma: A case report. // Radiol Case Rep - 2021 - Vol16 - N6 - p.1311-1314; PMID:33897922
What are the causes of toxicosis?
Nobody knows for sure. Some doctors believe that it is a consequence of significant changes in hormonal levels in pregnant women, and list hCG (human chorionic gonadotropin), estradiol, and progesterone as the culprits of toxicosis. Others consider it a psychological condition, something like neurosis, and prove their point of view by the fact that toxicosis during pregnancy often occurs against the background of a woman’s stressful state.
There is a theory that toxicosis is not a disease at all, but, on the contrary, an evolutionary advantage. And really, when does it start? In the early stages, i.e. precisely when the fetus is most vulnerable to toxins. At the same time, the pregnant woman’s body reacts to the most dangerous odors - meat, fish (potential sources of parasites, harmful bacteria), alcohol, cigarette smoke, other sharp-smelling foods, household chemicals, etc. It turns out that with the help of toxicosis, the body tells you that, we hope, you already understand perfectly well: during pregnancy, especially in the first trimester, you need to very carefully monitor your diet and health.
Toxicosis: why and for what?
- Nervous system. It has been noticed that toxicosis is most pronounced in anxious women, managers, doctors, teachers, that is, people with increased nervous stress. And, by the way, note that animals do not have such toxicosis as people do. They do not take on “all the world's responsibility” and therefore do not feel sick or vomit. At most, females sleep a lot and retire to save energy.
- Lifestyle. If a woman enters pregnancy not in a resourceful state, tired, exhausted, slagged from poor nutrition and lack of water, and even after some illness, poisoning, herpetic manifestations, ARVI, then the body will try to “put the woman to bed” in order to get enough sleep, rest, gain strength, eat different foods to replenish your reserves. Everything is logical. This is a smart move in the fight for survival.
- Every person has a unique genetic code, which is laid down at the moment of fertilization. And how different it will be from the mother’s code, the toxicosis will be expressed. To make it clearer, there are people who are so similar in this code and protein composition that their organs can be transplanted to each other and they will take root. Others, on the contrary, are not at all similar, and if a kidney is transplanted from such a person, for example, it will be rejected. Also here. If a child has inherited a similar genetic code, then the intoxication from its protein entering the mother’s blood will be less. And vice versa. As pregnancy progresses and the placenta forms between the body of the mother and the child, a placental barrier is formed. And toxicosis decreases: that’s why in most women it goes away by the 12th week.
What are the symptoms of toxicosis?
Nausea and vomiting, if you're lucky - just nausea. Sometimes attacks of malaise occur for no apparent reason, but most often they are a reaction to pungent smells and tastes. Other symptoms, such as abdominal pain, headache, fever, are not typical for toxicosis and are rare. If you have diarrhea along with vomiting, most likely it is just poisoning.
How severe is toxicosis during pregnancy?
Based on the severity of symptoms, there are two types of toxicosis in early pregnancy. A mild or moderate form is when vomiting occurs no more than 5 times a day, and the woman does not lose or almost does not lose weight. It doesn’t sound very easy, but it’s still just flowers 
The severe degree is called Hyperemesis gravidarum in Latin, and in Russian - excessive vomiting of pregnant women. This form is characterized by uncontrolled vomiting, leading to dehydration, weight loss and ketosis (carbohydrate starvation of cells with the formation of acetone and other harmful substances in the liver). Hyperemesis gravidarum is not a very common occurrence, we wish you did not have to become familiar with it. However, you should not completely discount it: excessive vomiting occurs in 0.3–2.0% of pregnant women and causes the following unpleasant consequences:
- Losing more than 5% of weight.
- Dehydration, constipation.
- Nutrient deficiency, primarily vitamins B1, B6, B12.
- Metabolic disorders.
- Physical and psychological stress.
- Significant deterioration in the quality of life during pregnancy, problems at home and at work.
Modern medicine can combat this condition, but previously it led to serious consequences, including the death of the expectant mother. For example, all the facts indicate that the famous British writer of the 19th century, Charlotte Bronte, author of the famous novel “Jane Eyre,” died in the fourth month of pregnancy precisely from complications of severe toxicosis. At the same time, the Duchess of Cambridge Catherine Middleton, although she suffered from Hyperemesis gravidarum in the early stages during all three pregnancies, successfully went through it and pleases us with photographs with the princess and two princes.
Is toxicosis dangerous for the baby?
Usually it does not have the slightest effect on the development of the fetus. Quite the contrary: some studies show a connection between toxicosis and the likelihood of miscarriage: in pregnant women suffering from nausea and vomiting, it is lower than in women who avoided this disease in the early stages. As you can see, everything has its positive sides 
Only very severe cases can become a problem, when toxicosis leads a woman’s body to severe exhaustion. But, let us repeat, modern medicine has in its arsenal therapeutic methods that make it possible to cope with this condition.
How can inpatient treatment help?
Staying in a hospital may be necessary, since frequent vomiting may cause dehydration, metabolic disturbances, a decrease in blood pressure, an increase in heart rate, a decrease in urine output, and constipation. If measures are not taken in time, a violation of water-salt, protein, carbohydrate and fat metabolism, acid-base and vitamin balance, and the functions of the endocrine glands may develop. All this can negatively affect the development of the baby, because it is in the first trimester of pregnancy that the laying and formation of all the main organs and systems of the baby occurs.
Therefore, do not refuse hospitalization under any circumstances if your doctor recommends it.
How to make life easier for an expectant mother during pregnancy with toxicosis?
There are several simple methods that can relieve toxicosis symptoms. Here are some of them:
- Full sleep. Lack of sleep can be an aggravating factor. During this period, pregnant women need to sleep at least 8 hours a day.
- The right diet. Toxicosis “reacts” to strong smells and tastes, so in the early stages the expectant mother needs to exclude fatty, smoked, and spicy foods from her diet, and limit the consumption of fried meat and fish. Simply put, remove everything that poses a serious challenge to digestion even without pregnancy.
- Special diet. For toxicosis, it is recommended to eat little, but often - about 5-6 times a day. Food should not be heated too much: all dishes should be at room temperature or only slightly warm.
- Drink plenty of fluids. Vomiting causes dehydration and lost fluid must be replaced. During toxicosis during pregnancy, you need to drink at least 2 liters of water per day. But not carbonated!
- Walks. Taking leisurely walks in the fresh air can also help. If in everyday life you rarely walk further than a parked car, reconsider your habits.
- Yoga. Active sports are poorly compatible with toxicosis. But yoga is very good, and it can bring relief.
- Ginger. It is not clear what the reason is, but ginger helps. Some mothers also note the beneficial effects of decoctions of mint and chamomile, water with honey or lemon in the early stages. Here is a simple recipe for an “anti-toxic” drink: grate fresh ginger on a fine grater or grind it in a blender, mix with lemon juice, and add boiled water. Start drinking in small sips when it cools down.
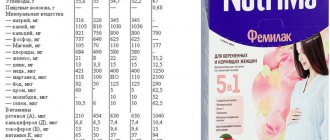
- Vitamins. Vitamin and mineral complexes can also contribute to the fight against the disease. Doctors note that it is easier in expectant mothers who took vitamins in preparation for pregnancy.
What to do if you can’t cope with toxicosis?
In severe cases, toxicosis can cause serious consequences for the expectant mother, and in order to prevent them, doctors often decide on hospitalization. At the hospital, specialists take a number of therapeutic measures, mainly aimed at stopping vomiting and restoring the balance of nutrients in the pregnant woman's body.
A combination of pyridoxine (vitamin B6) and doxylamine is considered a reliable drug treatment. Numerous studies confirm the highest safety of these drugs for a pregnant woman and fetus.
And most importantly, if you have any concerns about morning sickness, don't hesitate to contact your doctor!
How to eat properly?
Changes observed in diseases of the digestive organs are accompanied by disruption of excretory processes, due to which metabolic products of the mother and fetus are retained in the body, which aggravate nausea and contribute to increased vomiting, even indomitable. And yet, it is necessary to take into account that vomiting is a protective reaction aimed at freeing the body from substances that are harmful or poorly perceived during this difficult period. Therefore, nutrition is very important in the treatment and prevention of vomiting:
- Food should be well cooked and pureed.
- Meals should be taken every 2-3 hours, in small portions, so as not to overload or irritate the stomach.
- It is useful to take your first breakfast in the morning, while still in bed.
- It is not recommended to eat dense and liquid foods at the same time.
- It is advisable to warm the food slightly.
You can replenish the fluid lost by the body by daily administration of 1-2 liters of fluid (5% glucose solution prepared in saline solution) in the form of drip enemas. Excessive loss of minerals (especially sodium, chlorine) is compensated by including herring in food in the form of pate and adding salt to food.
You can use a mostly dry diet: baked potatoes with butter, an egg, toasted white bread, porridge with butter. You should not drink half an hour before meals and for an hour and a half after meals. Fasting days help a lot. During the day, you should drink 1.5 liters of compote (one glass every two hours) or eat 500 g of cottage cheese and 100 g of sour cream, divided into 4-5 doses. Fasting days of different fruits in the form of puree are also desirable.