Planning and preparing for pregnancy
In order for a healthy baby to be born, pregnancy must not only be desired, but also planned. Pre-conception preparation for pregnancy is a set of diagnostic, preventive and therapeutic measures that allow you to prepare a married couple for the upcoming conception and pregnancy.
Where should you start preparing for pregnancy? With a thorough examination of both spouses, which includes:
- specialist consultations. The most important specialist for women is a gynecologist, and for men an andrologist;
- determination of the blood type and Rh factor of both spouses;
- biochemical, hormonal laboratory tests;
- tests for STIs (sexually transmitted infections);
- visit to a geneticist.
A full examination should be carried out 3-4 months before the planned pregnancy. A thorough diagnosis will identify diseases in parents that may affect the unborn child. For example, every second woman has a lack of folic acid in the body. Taking vitamin B9 for several months before pregnancy can reduce the likelihood of developing birth defects in the fetus several times.
During the examination of parents, problems are often discovered that can interfere with pregnancy. Common causes are endocrine disorders, inflammatory processes of the genitourinary system, adhesions in the pelvis, autoimmune diseases, genetic incompatibility of spouses. The sooner treatment for such problems begins, the higher the likelihood of successfully conceiving a child.
Equally important is the psychological preparation of parents for pregnancy. For example, some women are afraid of the onset of this period. The problem lies in the uncertainty of the future, in the fear of possible complications and painful childbirth. In such a situation, a woman needs to contact a perinatal psychologist who will tell you how to overcome fears and be ready for pregnancy .
Stages of the IVF procedure
Before describing how fertilization will occur, it is worth noting the sequence of actions to prepare for it. The donor and recipient are prepared for upcoming procedures by synchronizing their menstrual cycles. To do this, hormonal drugs are used so that the processes of the reproductive system occurring in the bodies of two different women coincide.
This is followed by the introduction of another type of hormonal drugs to the donor in order to stimulate the maturation of several follicles at the same time, in contrast to the physiological menstrual cycle, when only one follicle matures completely.
After which a drug is administered that stimulates ovulation of all mature follicles. As a result, from three to four to eight or more eggs are obtained, which are subsequently removed from the donor under anesthesia by puncture. The entire procedure for preparing and obtaining eggs can take a considerable amount of time, up to several weeks.
And ultimately, fertility doctors begin the most important process - fertilization.
First signs of pregnancy
Pregnancy in a woman occurs after the fertilization of an egg by a sperm in the ampullary section of the fallopian tube. As a rule, this occurs during the period of ovulation, on days 10–16 of the menstrual cycle.
The main sign of pregnancy is the absence of menstrual bleeding. However, even before the onset of a delay in menstruation, a woman may experience indirect signs that allow her to suspect pregnancy:
- increased basal temperature (BT) in the second half of the menstrual cycle. This sign can be noticed by women who regularly measure BBT and plot its changes. During ovulation, due to a hormonal surge, BBT increases to 37–37.6 degrees. If pregnancy does not occur, then after ovulation the temperature readings drop. When conception occurs, BT will remain above 37 degrees;
- scant bloody discharge from the vagina, caused by the implantation of the embryo into the mucous membrane of the uterine body;
- feeling of heaviness in the lower abdomen;
- irritability, mood swings;
- general weakness, drowsiness;
- swelling of the mammary glands;
- low blood pressure;
- frequent urination.
Why are these signs of pregnancy considered indirect? Yes, because they do not give a 100% reliable result. For example, BT values can be distorted by factors such as stress, increased physical activity, and incorrect temperature measurements. Other indirect signs of pregnancy are similar to the symptoms of premenstrual syndrome (PMS), and therefore are also not reliable.
How can you accurately determine whether you are pregnant? You should visit an obstetrician-gynecologist and undergo the necessary diagnostics. Approximately 10 days after the start of the delay, a slight enlargement of the uterus is observed, which the gynecologist will definitely notice during the examination.
Laboratory diagnostic methods include determining the level of hCG in urine and blood serum. The hCG hormone is produced by the chorion (fetal structures). The hormone can be detected in the blood of a pregnant woman approximately 10 days after conception, in the urine - 4-5 days later. Laboratory tests for hCG levels are important elements of screening during pregnancy , which can not only confirm the fact of conception, but also identify some pathologies.
An alternative to a urine hCG test is a pregnancy test performed at home. However, there is a possibility of false negative results. For example, unreliable results may be obtained if a lot of liquid was drunk before the test or the woman has kidney pathologies. In any case, after a negative result, the procedure must be repeated after a few days.
Using an ultrasound examination performed on a high-resolution device, pregnancy can be determined 21 days after conception, which corresponds to 5 weeks of the obstetric period. But to obtain the most accurate result, experts recommend performing the first planned ultrasound at 1 1.0-13.6 weeks of pregnancy. At an earlier date, the results may be erroneous. For example, if a woman has endometrial polyps of the uterus, they can be mistaken for an embryo.
Many women are interested in the question: is it possible to determine an ectopic pregnancy using a test at home? An indirect sign of pathology is a test result in which the second strip looks fuzzy and blurry. However, it is possible to accurately determine the presence or absence of an ectopic pregnancy only with the help of special research methods.
How is the gestational age determined?
It is important for every pregnant woman to understand that there are obstetric and embryonic stages of pregnancy. What is the difference between these two concepts?
The beginning of the embryonic (true) term is considered to be the approximate date of conception of the child. The beginning of the obstetric period is the first day of the last menstruation. It is the obstetric gestational age that is used to determine the date of the upcoming birth and maternity leave.
The question arises: why do gynecologists take into account the obstetric period and not the embryonic period? The thing is that the duration and regularity of the menstrual cycle varies among women. In order not to understand each individual case and not to calculate the date of ovulation, a universal system was invented that is used all over the world and has proven its effectiveness in practice.
Ultrasound examination is also a highly accurate method for determining the duration of pregnancy. When setting the term, the doctor is guided by the diameter of the fetal egg, coccygeal-parietal size and other parameters.
In addition, ultrasound in the early stages of gestation allows:
- diagnose ectopic pregnancy;
- determine the number of fertilized eggs;
- assess the size and vital activity of the fetus;
- examine embryonic structures.
Screenings during pregnancy
Screening during pregnancy is a set of diagnostic measures aimed at identifying disorders in women that can affect the gestation and development of the fetus, as well as the upcoming birth. There are five types of screening:
- biochemical - blood test for biochemical markers: free b-hCG and PAPP-A;
- ultrasonic. Ultrasound screening during pregnancy is carried out to identify abnormalities of fetal development, pathologies of the woman’s genital tract, assess the condition of the placenta, the amount of amniotic fluid;
- immunological. Aimed at identifying possible infections in a woman that could be dangerous for the unborn child. Such infections include rubella, toxoplasmosis, cytomegalovirus and others;
- molecular - a screening program for hereditary pathologies that occur no more often than 1% of newborns;
- karyotyping - determining the likelihood of developing chromosomal abnormalities in the fetus depending on the age of the pregnant woman and family history. Such screening is carried out only if there are certain indications.
A woman undergoes a comprehensive examination three times during pregnancy:
- The first screening is scheduled at 10-13 weeks.
- The second screening is carried out at 18-20 weeks.
- The third screening is performed at 30-34 weeks.
more about screening during pregnancy in our article.
Infections during pregnancy: flu, coronavirus
The influenza virus is an acute viral infection that enters the human body through the respiratory tract and mucous membranes of the eyes. Much less often, infection with the virus occurs through hygiene items and utensils. Pregnant women have an increased likelihood of contracting an infection, because during the period of bearing a child they experience a decrease in the body's defenses.
How dangerous is the flu for pregnant women? A lot depends on the gestational age.
- In the first trimester, influenza poses the greatest danger to the fetus. During this period, the laying of all the internal organs of the embryo occurs. Infection can negatively affect their formation and cause pregnancy to fail.
- In the second and third trimesters, the likelihood of complications in the fetus decreases, because during this period it is protected by the placenta. However, even at this time, there is a threat to the unborn baby: influenza can lead to damage to the placenta, intrauterine infection of the fetus, slowdown in its growth and development, and premature termination of pregnancy.
Coronaviruses are a family of RNA viruses that are transmitted from person to person through airborne droplets, airborne dust, and contact. COVID‑19 is a new type of coronavirus that is highly contagious and has severe consequences. The disease can lead to pneumonia, respiratory failure, disruption of the cardiovascular system, and intoxication of the body.
Do women have an increased risk of contracting coronavirus during pregnancy? What consequences can coronavirus cause during pregnancy? At the moment, there is no exact answer to these questions: COVID‑19 has not yet been studied enough. However, due to the physiological characteristics of pregnant women, it is logical to assume that women during gestation are highly susceptible to coronavirus, and their infection is more severe than in other patients.
The most effective way to combat influenza and coronavirus during pregnancy is prevention. The main preventive measures include:
- Self-isolation during pandemics. During viral outbreaks, it is important to avoid visiting public places.
- Use of medical masks and disposable gloves when in crowded places.
- Careful hand hygiene, use of antiseptics.
Exercising during pregnancy
Physical education during pregnancy improves the general condition of a woman, has a beneficial effect on the autonomic nervous system, helps reduce pregnancy toxicosis, shorten the duration of labor and a more prosperous postpartum period. Its special tasks: strengthening the abdominal muscles; improvement of pushing activity during childbirth; prevention of sagging abdomen and prolapse of internal organs; strengthening and increasing the elasticity of the pelvic floor muscles to prevent prolapse and loss of internal genital organs; strengthening the entire body muscles, especially the back muscles, which bear the greatest load when walking, due to a shift in the center of gravity during pregnancy; increased mobility of the joints of the pelvis and spine; training in breathing skills during childbirth, improving the function of external respiration in order to enhance the oxidative processes of the body necessary for the development of the fetus.
Physical exercise is recommended for all women with a normal pregnancy, as well as for pregnant women with diseases of the cardiovascular system in the compensation stage.
Contraindications for gymnastics and sports during pregnancy:
1) all acute stages of diseases of the cardiovascular system with circulatory disorders, thrombophlebitis, tuberculosis (complicated by pleurisy, hemoptysis), kidney and bladder diseases (nephritis, nephrosis, pyelocystitis);
2) pronounced toxicoses of pregnancy (uncontrollable vomiting, nephropathy, preeclampsia, eclampsia);
3) uterine bleeding;
4) habitual miscarriage.
During pregnancy, those types of physical exercises that involve sudden shaking of the body (jumps, dismounts), sharp turns, and strength exercises are prohibited. Participation in sports competitions is strictly prohibited due to strong physical and nervous tension.
In addition to physical exercise, throughout pregnancy it is recommended to include walks in the general daily routine at any time of the year lasting up to 2 hours with stops for rest. In the second half of pregnancy, the walking distance is reduced, and the time spent in the air increases; in winter it should be at least 1.5 hours, and in summer much more.
Special studies have found that physical exercises carried out during pregnancy improve the course of labor and reduce the likelihood of perineal rupture and other complications.
Changes in the female body and fetal development by trimester
The female body undergoes serious restructuring during gestation. Each trimester brings new physiological changes and increases the risk of developing certain pathologies.
First trimester
The first trimester of gestation is the most difficult period of pregnancy. When a new life is born, all organs and systems begin to function completely differently. So what changes occur in a woman’s body?
- The ovary forms the corpus luteum, which produces large quantities of progesterone. This hormone creates the most favorable conditions for implantation of a fertilized egg into the endometrium of the uterine cavity.
- The chorion of the embryo begins to produce the hormone hCG, which maintains the functionality of the corpus luteum.
- The pituitary gland increases the production of prolactin. Thanks to this, the fat cells of the mammary glands are replaced with secretory ones - this is how the body prepares for breastfeeding. In addition, the hormone regulates the functioning of a woman’s adrenal glands and affects the development of the embryo’s respiratory system.
- Immunity decreases, which increases the risk of developing inflammatory processes and exacerbation of chronic diseases that were observed in a woman before pregnancy.
- The excitability of the central nervous system increases. In this regard, a woman experiences drowsiness, irritability, and fatigue.
- Starting from the 5th week of gestation, most pregnant women experience toxicosis, which is accompanied by nausea and changes in eating behavior.
In addition, pregnant women may experience a decrease in visual acuity, a burning sensation and dryness in the eyes. If you have such symptoms, you should definitely consult an ophthalmologist.
The first trimester of gestation is an important stage in the development of the embryo, when all the organs and systems of the unborn baby are formed. The formation of the brain and spinal cord, digestive system, respiratory organs, heart, blood vessels, and endocrine glands occurs. The skeleton, muscle tissue, and genitals are formed. By the end of the first trimester, it becomes possible to determine the gender of the unborn child. The pregnant woman’s condition is improving: toxicosis and irritability disappear.
more about changes in the female body and embryo development in the 1st trimester in our article.
Second trimester
As a rule, the second trimester of gestation is much more stable than the first. Such unpleasant symptoms as nausea and increased fatigue are already behind us. The pregnant woman begins to feel more comfortable. However, the unborn baby continues to develop and grow, which cannot but affect the woman’s physical condition.
It is in the second trimester that women often experience a lack of calcium, which is spent on the needs of the child. A deficiency of this substance can affect the condition of the teeth. It is important to address any dental problems during pregnancy immediately. All body systems are interconnected, and even caries can cause serious inflammatory processes. Read about the features of dental treatment during gestation .
In mid-pregnancy, women have an increased risk of inflammatory diseases of the genitourinary system. This is due to an increase in the size of the fetus and uterus, specific changes in the condition of the mucous membrane of the genital tract and, of course, a decrease in the body’s defenses. Pathologies that were previously unusual for women may occur: pyelonephritis, cystitis, bacterial vaginosis.
In addition, in the second trimester, the load on bones, muscles and ligaments increases. To avoid the development of pathologies of the musculoskeletal system, it is important for a woman to visit an osteopath. How a specialist can help during pregnancy - detailed information in our material .
Physiological changes in the female body in the second trimester include:
- white vaginal discharge, which occurs due to increased secretion of estrogen;
- false contractions caused by “training” contractions of the uterus. They are more characteristic of the 3rd trimester; their presence in the second trimester may indicate a threat of miscarriage;
- enlargement of the abdomen and mammary glands;
- increased sensitivity of the nipples.
How does the fetus develop during the second trimester? He is growing quickly and gaining weight. The musculoskeletal system, immune, respiratory, reproductive, and urinary systems are improved.
complete information about fetal development in the second trimester in our article .
Third trimester
The last trimester of gestation is accompanied by rapid weight gain of the pregnant woman, which is primarily due to the intensive growth of the fetus. During this period, it is very important to carefully monitor body weight and prevent the development of obesity. Being overweight can cause gestational diabetes, a serious disease that often causes fetal abnormalities and difficult births.
In the third trimester, as in the second, the risk of developing inflammatory processes in the genitourinary area is increased. If kidney pathologies occur during pregnancy, then the woman experiences pain in the lower abdomen, symptoms of intoxication of the body (nausea, vomiting, diarrhea), and painful urination.
Inflammatory processes in the genital area may be accompanied by pathological vaginal discharge, itching in the genital area, and pain in the lower abdomen. The appearance of any of the listed symptoms should be a reason to contact a specialist.
At the end of pregnancy, there is a high probability of developing gestosis, which is characterized by a triad of symptoms:
- high blood pressure;
- swelling;
- the appearance of protein in the urine.
An obstetrician-gynecologist treats the disease and monitors the effectiveness of therapy . For the first degree of gestosis, outpatient treatment is allowed. In case of complicated forms of the disease, the pregnant woman is sent to the hospital.
What happens to the unborn baby during the third trimester? Weight and height increase very quickly. The fetus begins to see and hear better, can respond to light and sounds, focus its gaze, smile and move actively.
For more information about how intrauterine fetal development occurs week by week, read our material .
Changes in UBC during pregnancy
A general blood test (CBC) during pregnancy is a simple and informative test that provides the doctor with valuable information about the functioning of the female body and some information about the condition of the unborn baby. Pregnancy is a specific condition in which the functioning of the circulatory system changes.
What changes in the CBC are observed during pregnancy?
- In late gestation, the hematocrit value, which measures the volume of red blood cells, may decrease. The reason for the drop in the indicator is an increase in the total plasma volume.
- During pregnancy, 40% of women experience erythrocytopenia - a low level of red blood cells per unit volume of blood. The main factor in this phenomenon is an increase in circulating blood volume. This is a completely normal process, but a significant decrease in indicators is considered a pathological sign.
- Pregnant women often have increased levels of white blood cells, which is due to the active functioning of the immune system. A woman’s immunity during gestation does double duty: it protects the pregnant woman and the fetus from infections. A significant increase in the number of leukocytes may indicate acute inflammatory processes or exacerbation of chronic diseases.
- In the second and third trimesters, an abrupt increase in ESR may be observed. But the increase in indicators must be within the limits established for pregnant women. Higher values are observed in infectious diseases, intestinal pathologies, and diabetes.
If deviations from the norm are detected in the CBC during pregnancy, the woman is prescribed a biochemical blood test, which is considered more informative.
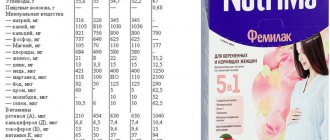
The norms of blood counts during pregnancy in the first, second and third trimesters are presented in the table.
Read more about changes in blood tests during pregnancy .
Lifestyle of a pregnant woman, regime, nutrition and hygiene
The developing fetus receives all the necessary nutrients from the mother. The well-being of the fetus depends entirely on the health of the mother, her working conditions, rest, diet, and the state of the nervous and endocrine systems.
Pregnant women are exempt from night shifts, heavy physical work, work associated with body vibration or adverse effects of chemicals on the body. substances. During pregnancy, sudden movements, heavy lifting and significant fatigue should be avoided. A pregnant woman needs to sleep at least 8 hours a day. A walk before bed is recommended.
A pregnant woman must be carefully protected from infectious diseases, which pose a particular danger to the body of the pregnant woman and the fetus.
During pregnancy, you need to be especially careful about keeping your skin clean. Clean skin helps eliminate metabolic products that are harmful to the body through sweat.
During pregnancy, it is recommended to take a shower and avoid overheating the body. Air and sun baths are recommended for healthy pregnant women.
A pregnant woman should wash her external genitalia twice a day with warm water and soap. Douching during pregnancy should be prescribed with great caution.
During pregnancy, you should carefully monitor the condition of the oral cavity and carry out the necessary sanitation.
The mammary glands must be washed daily with warm water and soap and dried with a towel. These methods prevent cracked nipples and mastitis. If your nipples are flat or inverted, you should massage them.
Pregnant women's clothing should be comfortable and loose: they should not wear tight belts, tight bras, etc. In the second half of pregnancy, it is recommended to wear a bandage that should support the abdomen, but not squeeze it.
A pregnant woman should wear low-heeled shoes.
Obstetric and non-obstetric pain during pregnancy
Pain during pregnancy is a common phenomenon that can accompany a woman throughout the entire gestation period. And most often during pregnancy, women have stomach pain. It is with this problem that many patients come to see an obstetrician-gynecologist, fearing for the health of their unborn baby.
Why does my stomach hurt during pregnancy? Pain that occurs during gestation is usually divided into obstetric and non-obstetric. The former are associated with the functioning of the reproductive system, the latter arise due to extragenital disorders and pathologies.
In turn, obstetric pain can be divided into physiological and pathological. In the early stages of pregnancy, physiological pain appears due to stretching of the uterine muscles, softening of the tissues to support the uterus. In late gestation, they are caused by pressure from the uterus and fetus on the pelvic organs and other factors.
Obstetric pathological pain is often severe and may indicate the following problems:
- ectopic pregnancy . Unbearable pain occurs when the fallopian tube ruptures. Additional symptoms are brown vaginal discharge, the urge to defecate;
- frozen pregnancy. Complications can occur in any trimester of pregnancy. Associated symptoms are bloody vaginal discharge, a decrease in basal temperature below 37 degrees;
- premature placental abruption . The pathology is typical for late gestation. If the area of placental abruption is large, sharp pain in the lower abdomen and heavy bleeding begin.
Possible causes of ectopic pregnancy
Main risk factors:
- infectious and inflammatory diseases - previously suffered or passed into the chronic phase - inflammation of the uterus, appendages, bladder are considered one of the main causes of ectopic pregnancy.
- Inflammatory processes in the ovaries and tubes (previous difficult births, multiple abortions, spontaneous abortions without going to a medical clinic), leading to fibrosis, the appearance of adhesions and tissue scarring, after which the lumen of the fallopian tubes narrows, their transport function is disrupted, and the ciliated epithelium changes. The passage of the egg through the tubes becomes difficult and an ectopic (tubal) pregnancy occurs;
- congenital infantilism of the fallopian tubes - irregular shape, excessive length or tortuosity with congenital underdevelopment are the cause of improper functioning of the fallopian tubes;
- pronounced hormonal changes (failure or insufficiency) - diseases of the endocrine system contribute to the narrowing of the lumen of the fallopian tubes, peristalsis is disrupted and the egg remains in the cavity of the fallopian tube;
- the presence of benign or malignant tumors of the uterus and appendages - narrowing the lumen of the fallopian tubes and interfering with the advancement of the egg;
- abnormal development of the genital organs - congenital abnormal stenosis of the fallopian tubes prevents the advancement of the egg to the uterine cavity, diverticula (protrusions) of the walls of the fallopian tubes and uterus make it difficult to transport the egg and cause a chronic inflammatory focus;
- a history of ectopic pregnancies;
- change in the standard properties of the fertilized egg;
- slow sperm;
- certain technologies of artificial insemination;
- spasm of the fallopian tubes, which occurs as a result of a woman’s constant nervous overstrain;
- the use of contraceptives - hormonal, IUDs, emergency contraception, etc.;
- age of the pregnant woman after 35 years;
- sedentary lifestyle;
- long-term use of drugs that increase fertility and stimulate ovulation.
What should you not do during pregnancy?
The health of the child directly depends on a woman’s behavior during pregnancy. And, of course, it’s not easy for pregnant women, because you need to follow many rules and recommendations.
What should pregnant women absolutely not do?
- Smoking and drinking alcohol. Such bad habits always have a negative impact on the development of the fetus.
- Eating poorly. The developing embryo must receive sufficient amounts of vitamins, minerals and other elements. To avoid vitamin deficiencies, include fresh vegetables and fruits in your menu. Enriching the diet with fermented milk products and legumes is an excellent prevention of calcium deficiency.
- Ignore medical examination. Early diagnosis of diseases allows timely treatment to begin and the development of complications to be avoided.
- Lead a passive lifestyle, which leads to excess weight gain and suppresses the immune system. Light morning exercises, regular walks in the fresh air, visiting the pool - all this has a positive effect on the physical and psychological state of a woman, as well as on the development of the unborn baby.
- Be nervous and panic. It is important to avoid stress and maintain a positive attitude. Negative emotions and experiences will negatively affect not only your health, but also the development of the child. As a rule, overly emotional mothers give birth to restless children who sleep poorly and refuse to breastfeed.
In addition, in late stages of gestation, pregnant women should not sleep on their backs. This can lead to compression of the vena cava, which runs along the spinal column, and fetal hypoxia.
Is it possible to follow a diet during pregnancy? What should you not eat during pregnancy? Read about this in our material .
Genital organs during pregnancy
Uterus. During pregnancy, the size, shape, position, consistency and reactivity (excitability) of the uterus changes. The uterus gradually enlarges throughout pregnancy. Enlargement of the uterus occurs mainly due to hypertrophy of the muscle fibers of the uterus; At the same time, muscle fibers multiply and the newly formed muscle elements of the reticular-fibrous and argyrophilic “framework” of the uterus grow.
The uterus is not only a fruit repository that protects the fetus from adverse external influences, but also a metabolic organ that provides the fetus with enzymes and complex compounds necessary for the plastic processes of a rapidly developing fetus.
the vagina lengthens and widens, and the folds of the mucous membrane become more pronounced. The external genitalia loosen during pregnancy.
Childbirth: preparation and first signs
The process of childbirth and the postpartum period largely depends on proper preparation for childbirth. Preparing for childbirth needs to be done in several directions at once: it is important to prepare psychologically and physically.
The optimal solution for full preparation for childbirth is special courses for pregnant women , where doctors, psychologists, and fitness instructors work with women. Both expectant mothers and fathers can attend such courses.
Where is the best place to give birth?
Before giving birth, it is important to decide where you will give birth: at home or in a maternity hospital. Home births in the presence of an experienced midwife have recently become increasingly popular: they provide the woman with psychological comfort. However, such births, compared to traditional ones, also have disadvantages: a high risk of complications and a wide list of contraindications.
Home birth is prohibited for the following pathologies and conditions:
- multiple pregnancy;
- decompensated diabetes mellitus;
- severe kidney disease;
- arterial hypertension;
- pathologies of the cervix;
- malposition;
- fetal malformations.
Harbingers and signs of labor
At the end of the third trimester, most pregnant women begin to listen to their body in anticipation of the harbingers of labor. What signs indicate that you will soon see your long-awaited baby?
- Abdominal prolapse.
- Removal of the mucus plug.
- Frequent urination.
- Lower back pain.
The birth itself begins with contractions - involuntary contractions of the muscular layer of the uterus, which allow the baby to be born. There is often early rupture of amniotic fluid, without previous cramping contractions. This is a reason to go to the maternity hospital, where they will help mother and baby be born safely.