Biliary dyskinesia is a disease as a result of which the flow of bile into the duodenum is stopped or significantly reduced due to uncoordinated work (contractions) of the ducts, gallbladder and sphincter of Oddi. Bile is a special liquid that is produced by the liver and promotes the breakdown of fats and the movement of food through the intestines. Before bile enters the intestines, it passes through the bile ducts - the hepatic and bile ducts, the gallbladder, and the sphincter of Oddi. The latter, due to its contractions, ensures its entry into the duodenum.
Dyskinesia is often observed in children, which is expressed by pain in the right hypochondrium and disturbances in the functioning of the digestive tract. As a result of the disorder, the child experiences a deficiency of bile in the intestines, which entails disruptions in the digestive tract and a deterioration in the general condition of the body. The latter is caused by insufficient absorption of many nutrients and vitamins K, E, A and D, which significantly worsens if bile does not participate in the process.
Causes of biliary tract diseases in children
Biliary dyskinesia does not manifest itself in structural changes in internal organs - liver, gall bladder, ducts. Its cause is a violation of their function, which is caused by malfunctions in the central nervous system and the autonomic system of the body. The causes of the disease should be sought much deeper than it might seem at first glance - in the vast majority of cases, in the emotional state of the child.
Stressful situations, increased emotionality, nervous breakdowns - all this affects the state of the child’s body and leads to excessive involuntary contractions of the gallbladder. Because of this, excess bile accumulates in the area of the bile ducts, which begins to thicken, losing its antibacterial properties and functionality. At the same time, the formation of stones and blood clots begins inside the biliary tract, which interferes with the natural movement of bile to the duodenum. As a result, the disease itself develops and its complications become probable.
Additional factors of psychosomatic causes of the development of the disease may be:
- irregular meals;
- excess fat in food;
- a large amount of spicy, salty, smoked foods in the diet;
- consumption of junk food - nuts, crackers, soda;
- food allergies;
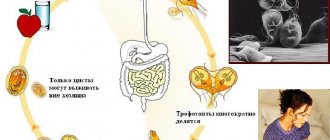
- intestinal parasites. Giardia is especially dangerous;
- side effects of certain pharmacological drugs;
- intestinal diseases and poisoning.
Frequency of meals and healthy foods are very important for children. This should be given the closest attention to anti-parasitic prevention. A specialist will help you adjust your child’s diet.
Why does JVP occur?
Possible causes of biliary dyskinesia include the following factors:
- irregular nutrition, predominance of fatty, salty, spicy foods, foods with flavor enhancers;
- cardiopsychoneurosis;
- food allergies;
- chronic diseases of the gastrointestinal tract;
- parasitosis;
- stress, increased neuro-emotional excitability;
- increased physical and intellectual stress.
Exacerbating factors may be excess weight in the child, a sedentary lifestyle, and functional intestinal disorders.
Types of dyskinesia
Depending on the type of functional disorders in the biliary tract in children, several types of disease are distinguished:
- hypotonic - expressed in a decrease in the tone of the sphincter of Oddi;
- hypertensive - manifests itself, on the contrary, in increased sphincter tone;
- hypokinetic - associated with a slowdown in the outflow of bile;
- hyperkinetic - accompanied by sudden releases of bile.
Mixed types of the disease are quite often observed. Functionally, each type of dyskinesia is characterized by different symptoms and requires a different approach to treatment. In each specific case, a specialist should prescribe procedures based on the results of tests and examinations.
Symptoms of dyskinesia
Depending on the type of disease, its symptoms manifest differently. In the hyperkinetic course of the disease, when contractions of the gallbladder are intensified, acute pain in the right hypochondrium manifests itself most intensely. It can spread to the thigh and also radiate to the shoulder blade. Typically, the pain is not constant, but manifests itself when eating fatty, spicy, fried foods, in stressful situations and during high physical activity.
If hyperkinetics of the gallbladder is combined with hypertension of the biliary sphincters, the pain is expressed somewhat more strongly and can occur without any apparent reason. Often biliary dyskinesia of the hyperkinetic type is accompanied by attacks of nausea and vomiting, worsening after eating.
With the hypokinetic type of the disease, children feel a constant nagging pain in the right hypochondrium. There is also a feeling of heaviness in the stomach, accompanied by loss of appetite. There may be attacks of nausea and a feeling of bitterness in the mouth. Stool disturbances are quite common - diarrhea, constipation or change in the color of stool (it becomes very light).
Symptoms of either type may worsen if children do not eat properly. Therefore, at the first signs and suspicions of the disease, it is necessary to adjust the diet and contact an osteopathic specialist who can diagnose the disease and prescribe effective treatment.
Danger of disease
Diseases of the biliary tract in children are quite dangerous, especially at an early age, when they are difficult to diagnose - the child is not yet able to talk about symptoms such as nausea or bitterness in the mouth. Although the disease itself is not exclusively dangerous, it does have unpleasant consequences. If children are not treated, then:
- the risk of stones forming in the gall bladder or bile ducts in children increases. This occurs due to the bile accumulating in it, which gradually thickens and hardens. Removing stones is not always possible using non-surgical methods;
- food is not digested properly. Bile helps break down fats and digest sweet foods. If this does not happen due to its lack in the intestines, some of the food begins to be absorbed incompletely or improperly. As a result, the body not only receives less nutrients and minerals, but also begins to accumulate harmful substances;
- metabolism is disrupted. Excess fats and sugars that are not broken down properly due to disruption of the biliary tract lead to weight gain and excess weight, and also increase the risk of developing diabetes. The latter is a serious and practically incurable disease, the manifestations of which can only be stopped. But it is impossible to do this without restoring the normal functioning of the bile ducts, gallbladder and liver;
- a digestive system disorder occurs. This is expressed in constant unpleasant sensations - nausea, heaviness in the stomach, pain in the intestines. Although, like dyskinesia itself, all this is not fatal, vomiting, diarrhea or constipation can hardly be considered pleasant moments in life.
Diagnosis of the disease
Dyskinesia, as a functional disease of the biliary tract, is quite difficult to diagnose. This group of disorders does not cause changes in the structure of external organs, which is why many conventional diagnostic methods are not so effective. An osteopath can help diagnose diseases of the biliary tract in children using manual techniques to assess the size and shape of the gallbladder. Additionally, an ultrasound may be prescribed, which will confirm the diagnosis. In some cases, a functional study is also prescribed, for example, using duodenal intubation.
Diagnostic methods
Treatment of biliary dyskinesia in children begins with an accurate and detailed diagnosis. The doctor must differentiate the disease from other gastrointestinal pathologies, determine the type of illness, and assess the child’s general health. At the initial appointment, he will ask several questions regarding the duration of symptoms, medical history, previous diseases and operations. If you already have the results of previous examinations and discharge, take them with you. In addition, mandatory palpation is carried out, this will help the specialist determine the further direction of diagnosis.
For a more accurate examination, laboratory tests (biochemical blood test, coprogram), ultrasound, and in rare cases, CT or MRI may be used. Cholecystography and gastroscopy are widely used.
Fractional examination of gastric juice and duodenal intubation is a reliable method, but is rarely used in pediatric practice.
Surgery
An indication for surgical intervention may be complicated dyskinesia, which cannot be eliminated with drug therapy. Surgery is also prescribed for severe pain and severe digestive disorders. Before surgical treatment, it is important to exclude other pathologies of the gallbladder, such as cholelithiasis or the growth of a malignant tumor. According to modern research, radical treatment is more effective in relieving the symptoms of the disorder.
Depending on the indications and condition of the patient, the doctor may perform an open or laparoscopic cholecystectomy. The operation involves removing the gallbladder. After the intervention, the functions of the digestive system are normalized, but some complications may develop, such as dyslipoproteinemia or dysfunction of the sphincter of Oddi.
Therapeutic diet
The following are excluded from the diet:
- rich chicken, meat and fish soups;
- marinades, smoked meats, pickles;
- fried and spicy foods.
Significantly limited:
- tomatoes;
- chocolate and cocoa;
- sweets;
- baking;
- ice cream.
Allowed:
- vegetarian soups;
- porridge;
- dairy products;
- boiled lean meat and fish;
- marshmallows and marmalade;
- non-concentrated compotes and weak tea;
- crackers and yesterday's bread;
- vegetables, berries and fruits.
How to distinguish dyskinesia from poisoning and intestinal infection?
Some dangerous diseases can masquerade as symptoms of ADHD. Let's figure out how these conditions differ.
| Symptom | JVP | Food poisoning/intestinal infection |
| First signs | Usually they increase gradually or there is a light interval between attacks. | They appear in a healthy child and within a few hours his condition worsens. There is often a relationship with the consumption of poor-quality food or the presence of patients with intestinal infection in the child’s environment. |
| Stomach ache | Paroxysmal and strong - with the hypertensive type. Dull and aching, worse after eating - with the hypotonic type. | The entire abdomen or upper part (stomach area) hurts. Small children show pain around the navel. |
| Nausea/ vomit | Appear during or immediately after eating. | Nausea almost constantly. Vomiting is repeated and profuse. They occur regardless of food intake, but may intensify after eating and drinking. |
| Appetite | Reduced or normal. | The child is bad or refuses to eat at all. |
| Chair | Hypotonic type - constipation. Hypertensive type - diarrhea that occurs immediately after eating or during an attack. | Frequent, does not depend on food intake. It can be watery or foamy. May contain particles of undigested food, mucus or blood (rarely). The color changes: it can be yellow, greenish. |
| Loss of consciousness | No. | Possibly in serious condition. |
| Body temperature | Normal. | It increases from the first hours of illness. |
| Dehydration (dry skin, baby losing weight) | No. | Due to vomiting and diarrhea it increases rapidly. |
Norma: how is everything arranged and how it works?
Knowledge will help you understand what is happening.
Bile
Produced by liver cells. It is a liquid containing special substances that are involved in many processes. Without bile, it is impossible to digest fats and move food through the intestines. Bile also helps destroy pathogens.
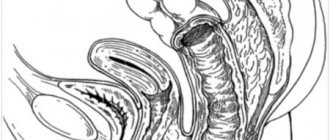
Biliary tract
Provide transport of bile from the liver to the duodenum. They consist of a system of ducts (elastic tubes) and the gallbladder. The walls of the ducts and bladder have a muscle layer, due to which they can contract. In some places, the walls of the ducts are thickened - these are muscle valves (sphincters).
Bile promotion
When we start to eat, the bladder and its ducts contract, and the sphincters relax and open - bile pours into the duodenum. Then, before the next meal, the gallbladder and its ducts relax and the valves close. A coordinated process is controlled by intestinal hormones and the nervous system.
Classification
Gastroenterologists classify gallbladder dyskinesia according to the clinical manifestations of the disease, etiology and nature of the motility disorder. All these signs help to choose the optimal treatment for the disease.
Main types of dyskinesia
- Hypertensive motility disorder, manifested by rapid uncoordinated contractions of the gallbladder walls. In most cases, this form of dyskinesia is diagnosed in children and young patients. The main symptom is acute paroxysmal pain that lasts for several minutes.
- Hypotonic motility disorder, in which the gallbladder muscles contract too rarely or not strongly enough. Hypomotor dyskinesia is usually found in older patients. The pain is less acute and lasts longer.
Another classification includes secondary and primary forms of the disorder. Dyskinesia can occur independently due to a violation of innervation, an anatomical defect or hormonal imbalance, but more often a secondary form of the disease is diagnosed, which develops against the background of pathologies of other organs.
Pathogenesis
Normally, the evacuation of bile is a coordinated process: sequential contraction of the smooth muscles of the body and neck of the bladder leads to the reflux of fluid into the bile ducts. After cholecystokinin stimulates the relaxation of the sphincter of Oddi, the secretion enters the small intestine and participates in digestion. The nervous system provides activation or inhibition of the functions of the gallbladder, depending on external factors. Specialists are rarely able to determine which link of regulation has changed when a pathology occurs.
Dyskinesia of the gallbladder is primarily manifested by uneven contraction of different parts of the organ. Thus, a combination of rapid contraction of the bladder neck with weakened activity of the muscles of the body of the organ is possible. As a result, bile is not completely excreted, and the walls of the bladder are stretched, after which abdominal pain occurs. Additional symptoms are often caused by other autonomic disorders that affect the pain threshold. A long delay in the excretion of bile is complicated by the formation of stones and complete blockage of the ducts.